FCM Sample Write-Up #1
Term 1
Sample A: Acute Problem
ID/CC
Mr. Y. is a 56 year-old man with a history of hypertension and peptic ulcer disease who presents with 5 days of diarrhea and right lower quadrant pain.
HPI
Mr. Y was in his usual state of good health until 5 days prior to admission while on a road trip with his son in Colorado. He developed diarrhea, described as loose, somewhat watery occurring two to three times a day. The volume of the stool was not more than normal. He also had nausea but no emesis, and was able to eat/drink normally. The stool was brown without melena or hematochezia.
At the same time, Mr. Y. also developed a dull, steady, and fairly mild pain in his right lower quadrant; “2 or 3” out of 10. If he pressed on the area, the pain became sharp and more intense. The pain did not radiate and there were no aggravating or alleviating factors. He had no jaundice, odynophagia, change in appetite, dysphagia or heartburn.
Three days prior to admission, Mr. Y.’s symptoms had not improved and he developed intermittent emesis. He developed subjective fevers and sweats. His nausea started to keep him up at night and his appetite decreased significantly. He tried taking acetaminophen for his symptoms but this did not provide any relief.
Mr. Y. returned to Seattle on the day of admission. Having not improved, he saw his family practice doctor who noted an elevated WBC on his blood work and instructed Mr. Y. to go to the ER.
While in Colorado, Mr. Y. stayed with family members who were sick with influenza. He also ate a “questionable” pork sandwich at a football game the night prior to the onset of his symptoms. His symptoms did not feel similar to those he experienced with his previous peptic ulcer disease in the 2000s, and Mr. Y. has never experienced anything like this before. Mr. Y. attributes his current symptoms to food poisoning from the pork sandwich in Colorado, but is also concerned that his appendix might be ‘acting up’.
Hospital Course: Mr. Y. had a CT scan in the ER which showed a partially ruptured appendix and he was admitted. Mr. Y. has been in the hospital for 2 days at the time of this interview. Upon arriving at the hospital, Mr. Y. had a surgical consultation for appendicitis. Surgery was not performed and Mr. Y. was administered IV antibiotics and put on bowel rest. His diarrhea, pain, and nausea all began to resolve within 12 hours of the onset of treatment. At this time, Mr. Y. has few symptoms and is feeling much better.
PMH
Major Childhood Illnesses
- Chickenpox -age 11
Medical Problems
- Hypertension, diagnosed 2013
- Diagnosed with BP approximately 190/110; currently on medications with average BP approximately 160/85
- Patient is unaware of any secondary problems/end-organ injury related to his hypertension
- Hypercholesterolemia, diagnosed 2013
- Currently controlled with simvastatin
- Most recent total cholesterol checked 3 months ago: 240
- Degenerative Disk Disease, diagnosed 2010
- Currently controlled with chiropractic manipulation; no current weakness or numbness
- Duodenal Peptic Ulcer Disease, early 2000s
- Treated with antibiotics, no recurrences since
Surgeries/Trauma
- Fingertip amputation repair- 2001
Psychiatric History
- No history of depression or mental illness
Medications
- Amlodipine/Benazepril, 2.5/10 ; 1 capsule by mouth every day
- Simvastatin, 40mg by mouth every night
- Complementary/Alternative Medication: None
Allergies: No Known Drug Allergies
Health Related Behaviors:
- Tobacco: Never
- Alcohol: 5 drinks/week
- Recreational Drugs: None
- Travel, Exposures: Colorado road trip (see HPI); significant travel to Asia and Europe within the past 20 years, none in the past 3 years.
- Personal safety habits: No firearms, uses seatbelts
- Sexual history: Female sexual partners; monogamous for 30 years; no STD testing
- PCP is family practice doctor in Issaquah
- Regularly visits a Chiropractor
- Visits a Dentist about once every two years
- Diet: Frequently eats out as he travels a lot
- Exercise: No regular exercise program
FHx:
- MGF – prostate CA; MGM – hyperlipidemia; paternal grandparents – unknown
- Father – MI x 2 in his 50s, died @ 82, CVA
- Mother – alive and well @ 84
- Three adult children – alive and well
SH:
Mr. Y. is a pilot for Alaska Airlines. Recently, his pilot’s license has been suspended due to his uncontrolled hypertension. Mr. Y. seems to be handling this well, using his free time to travel to see his sons and spend more time with his wife. He reported feeling excited by the fact that this situation may lead to an early retirement. Mr. Y., whose gender identity is male, has a close relationship with his family, and relies on them for support during stressful situations. His youngest son has just left home for college, and he and his wife are adjusting well to being empty-nesters in their home in Issaquah. He played football and lacrosse when he was younger, and enjoys watching his youngest son play lacrosse on a club team. Mr. Y. has health insurance and finances are not a significant source of stress. He is a Christian, but he reports this does not play a large role in his life.
ROS
General: see HPI
Derm: No rashes, pruritus, changing moles, lumps, lesions
HEENT: no headaches or trauma;
- Eyes: no diplopia, wears reading glasses, no change in vision, eye pain or inflammation
- Ears: no difficulty hearing, tinnitus, vertigo or pain
- Nose: nasal stuffiness/obstruction, no nose bleeds or sinusitis
- Mouth: no sores, sore throat or dentures
Respiratory: no dyspnea, pleuritic pain, cough, sputum, wheezing, asthma, hemoptysis, cyanosis, snoring, apnea, history of TB exposure, PPD
Cardiovascular: positive for HTN(see PMH), no chest pain, angina, dyspnea on exertion, paroxysmal nocturnal dyspnea, orthopnea, peripheral edema, history of murmur, palpitations, claudication, leg cramps, history of DVT
Gastrointestinal: see HPI
Genitourinary: No dysuria, nocturia, hematuria, frequency, urgency, hesitancy, urinary incontinence, urethral discharge, sores, testicular pain or swelling
Musculoskeletal: Positive for intermittent back pain, no other joint pain, swelling stiffness, or deformity; no muscle aches or locking of joints
Neurological: no dizziness, involuntary movements, syncope, loss of coordination, motor weakness or paralysis, memory changes, speech changes, seizures, paresthesias
Psychiatric: no sadness, sleep disturbance, crying spells, anorexia or hyperphagia, anhedonia, suicidal/homicidal ideation, loss of libido, anxiety, history of eating disorders, hallucination, delusions, behavioral changes
Hematologic: no anemia, easy bruising or heavy bleeding
Endocrine: No polyuria, polydipsia, head/cold tolerance
Functional status: Able to complete all ADLS without impairment (bathing, ambulating, toileting, transfer, eating, dressing). Able to complete all instrumental ADLs without impairment (shopping, cooking, mode of transportation, telephone use, laundry, housekeeping, responsibility for meds/finances).
PE
General: Mr. Y. is well-appearing, responds to questions easily and moves without difficulty, with no signs of acute distress.
Vital Signs: BP 160/90; Pulse 60; Resp 16
Skin: Warm, dry, no rashes. Well-healed surgical scar on right forearm. Nails normal without clubbing, cyanosis, or lesions.
HEENT:
Head: Normocephalic. Face, scalp and skull without lesions or tenderness.
Eyes: Vision 20/40 in each eye. Conjunctivae without injection, sclera anicteric. Corneal light reflex symmetrical. PERRLA. Red reflex present bilaterally. Disc margins not appreciated, retinal vessels normal in appearance and configuration. Fundi clear without hemorrhage or exudate bilaterally.
Ears: Left ear canal with small dark lesion, right ear canal without lesions or discharge. Tympanic membranes gray-white in color without bulging or erythema.
Nose: External nose without lesions or asymmetry. Nasal mucosa pink bilaterally without lesions, septum deviated to the left, inferior turbinates visualized bilaterally without lesions or exudates.
Mouth/Throat: Mucosa pink without lesions. Left lower molar dental carries. Uvula midline. Tonsils and posterior pharynx without erythema or exudate.
Neck/Thyroid: No palpable cervical lymph nodes. Thyroid normal in size and consistency, non-tender.
Chest/Lungs: Breathing symmetrical without use of accessory muscles. No tenderness on percussion of spine or CVAs. Lung fields resonant to percussion. Lungs with normal bronchovesicular breath sounds without wheezes or rales.
Cardiovascular:
Regular rate and rhythm, S1 single, S2 physiologic split.
| Pulse | DP | PT | R | C |
| Right | 1+ | 1+ | 2+ | 2+ |
| Left | 1+ | 1+ | 2+ | 2+ |
Abdomen: Normal bowel sounds. Tenderness to deep palpation of the right lower quadrant at McBurney’s point without guarding or rebound. No tenderness on deep palpation of the other quadrants. Liver 12 cm on percussion. Spleen not palpable. No masses.
Musculoskeletal: Normal range of motion of all four extremities. No lower extremity edema.
Genital: Omitted
Rectal: Omitted
Neurologic:
Mental Status: Alert, oriented to person, place, and time. Speech fluent, articulate, and appropriate.
CN II: Tested (vision, pupillary light reflex) and Intact
CN III, IV, and VI: Tested (extraocular eye movements) and Intact CN V: Tested (masseter muscles) and Intact
CN VII: Tested (facial contortion) and Intact CN VIII: Tested (finger rubbing) and Intact CN IX and X: Tested (phonation) and Intact
CN XI: Tested (shrug shoulders/turn) and Intact CN XII: Tested (protrude tongue) and Intact
Motor: Strength 5/5 throughout all muscle groups. Normal, fluid movements observed without tremor.
Sensation: Able to feel sharp and dull appropriately on hands and feet bilaterally.
Romberg negative. Reflexes: Biceps, triceps, knees, and ankles 1+ bilaterally. Toes downgoing bilaterally.
Cerebellum: Finger-nose-finger test smooth bilaterally; heel-shin smooth bilaterally. Gait normal.
Summary
Mr. Y. is a 56 year old man who presents with fever, diarrhea and RLQ abdominal pain of 5 days duration and has a physical exam remarkable for lower right quadrant abdominal tenderness on deep palpation without guarding or rebound pain.
Assessment
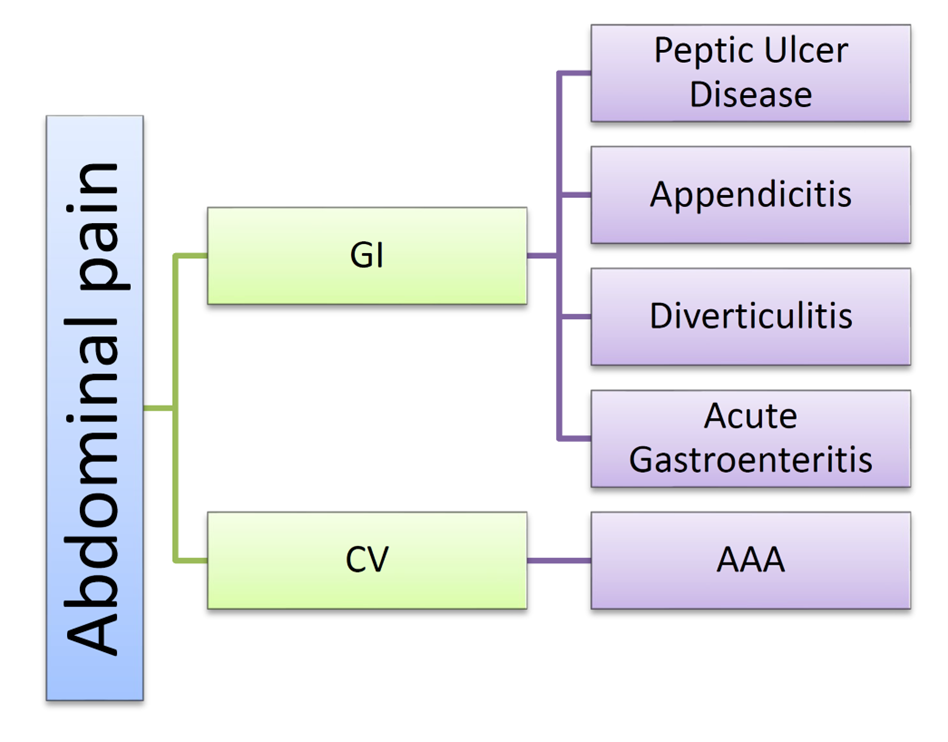
The most likely cause of Mr. Y’s abdominal pain, fever and right lower quadrant pain is acute appendicitis. Less likely possibilities are gastroenteritis, diverticulitis, and peptic ulcer disease.
A diagnosis of appendicitis is supported by Mr. Y’s fever, emesis and the localized pain and tenderness at McBurney’s point. The onset of his pain was somewhat atypical, starting in the RLQ rather than in the periumbilical area, although typical pain is seen in only 2/3 of patients. His loose stools are also unusual, but do not exclude the diagnosis.
Mr. Y’s fever, emesis and loose stools also raise the possibility of acute gastroenteritis, as does his belief that a bad pork sandwich started his symptoms. However, the focal tenderness at McBurney’s point and the 5 day duration of symptoms make gastroenteritis less likely.
Mr Y’s fever, emesis and anorexia could also be explained by diverticulitis. His age, sedentary lifestyle and low fiber diet are all risk factors for this condition. Diverticulitis causes LLQ pain in the vast majority of patients, though, and Mr Y’s pain was in the RLQ. R sided diverticulitis accounts for only 1.5% of cases, making this a less likely diagnosis for Mr. Y.
Although Mr. Y. had a previous history of peptic ulcer disease, the type and location of pain as well as association with fever makes this possibility an unlikely cause for his symptoms.
An unlikely but very serious explanation for Mr. Y’s abdominal pain is a ruptured aortic aneurysm. Mr. Y.’s male gender, age, and history of uncontrolled hypertension are consistent with aortic aneurysm. On physical exam, the lack of abdominal masses and bruits in addition to the lower right quadrant location of the pain make this an unlikely cause.