FCM Sample Write-Up #2
Term 1
Sample B: Chronic Problem
ID/CC:
KM is a 73-year old patient with a history of diabetes, hypertension and post-traumatic stress disorder who presents for scheduled chemotherapy for lymphoma diagnosed 6 months prior to admission.
HISTORY OF PRESENT ILLNESS
KM was diagnosed with lymphoma 6 months prior to this admission, after a six-month history of slowly progressive dyspnea which then rapidly worsened over the course of a few days. This “devastated my health.” At that time, KM found himself unable to lay flat or walk more than ten feet without experiencing extreme dyspnea, which nothing would alleviate. His family physician in Bremerton identified a mass in KM’s left lung field on CXR and fluid in the chest. He was transferred to the VA Medical Center in Seattle, where a CT confirmed a chest mass and a pleural effusion; upon further testing he was diagnosed with lymphoma.
Five months prior to the current hospital admission, KM began chemotherapy treatments every 3 weeks which included fludarabine and other chemotherapy drugs. Between diagnosis and one month prior to this hospital admission, KM was “in and out” of the hospital and ER and in relatively poor health. He needed to have a thoracentesis done every 4 days and he still experienced nearly constant dyspnea which was unrelieved with oxygen via nasal cannula. One month prior to hospital admission, “everything turned around”; KM experienced a decline in his dyspnea, his lung mass saw a more significant reduction in size, and he no longer required thoracentesis.
His oncologists plan to continue his chemotherapy for two more rounds. KM has had several complications of chemotherapy. He had an acute reaction to fludarabine during his first treatment which caused him to spend two days in the ICU. He does not recall the details of his reaction to fludarabine. KM also developed an “irregular heart beat” as a consequence of one of the medications in his chemotherapy regimen. One month prior to this hospital admission, KM was diagnosed with candidiasis in his mouth and nose; he recovered from this infection one week prior to this hospital admission.
KM’s review of systems at the time of admission was positive for recent nausea, vomiting, weight loss and gain, diarrhea, constipation, and dizziness (all as a consequence of his chemotherapy treatments). His respiratory review of symptoms was positive for pleuritic chest pain, cough productive of sputum (clear to yellow), wheezing, and snoring. He denied fever, chills, recent dyspnea, asthma, hemoptysis, cyanosis, history of sleep apnea, and history of TB exposure/positive PPD test.
KM attributed his diagnosis of lymphoma with his exposure to Agent Orange during his military service in Vietnam (1966-68).
PAST MEDICAL HISTORY
Childhood Illnesses
+measles, mumps, varicella zoster
Adult Medical Illnesses
- Post Traumatic Stress Disorder (PTSD)— diagnosed in 1980s. KM served in Vietnam from 1966-68, and has suffered with PTSD ever since He reports “self-medicating” with daily alcohol intake, until he quit drinking in 1984. He currently suffers with depression, crying spells, anxiety, sleep disturbances (nightmares), and hallucinations. KM claimed to not be on any medications for his PTSD, but is currently on prazosin for his nightmares (which he related to his PTSD).
- Diabetes—KM was diagnosed with diabetes 15 years ago when his roommate found him unconscious on the floor in the middle of the night. He was taken to the hospital where it was discovered that he had a blood glucose of 900 mg/dL. His diabetes is currently managed with insulin twice a day and “2-3 other diabetic medications.” He regularly sees an eye doctor, does self-foot exams, and has no neuropathy.
- Hypertension—diagnosed ten years ago. His hypertension is currently managed with “2-3 daily BP meds”
- Hypercholesterolemia—diagnosed ten years ago, currently managed with a daily “anti- cholesterol” medication.
- Osteoarthritis of knees since the early 2000s. He has had three arthroscopic procedures done on his right knee with minor symptom relief. He complains of current pain (4, on a scale of 1- 10) and swelling in his knees bilaterally. He also has some minor pain in his shoulder joints (2, on a scale of 1-10).
- Chronic abdominal pain—KM has had diffuse, constant abdominal pain (4, on a scale of 1-10) for five years. He had a thorough work-up done with a gastroenterologist two years ago, with no significant findings. KM requested to forgo the abdominal exam due to his discomfort.
- Obesity—KM is currently obese. He acknowledged both rapid weight loss and gain as a consequence of his chemotherapy treatments. He does not follow a special diet or exercise regimen.
Surgeries/T rauma
2002, 1998, and 1993—arthroscopic surgery of right knee (VA, Seattle)
Medications:
- NPH human insulin (HUMULIN® N)—unknown dosage twice a day
- regular insulin (HUMULIN® R)—unknown dosage twice a day prazosin—unknown dosage daily
- other diabetic medications—2-3 medications daily
- “cardiovascular”/anti-hypertensive medications—2-3 medications daily
- anti-cholesterol medication—unknown medication daily
- blood thinner—unknown medication daily
- chemotherapy—unknown name every 3 wks
- **no supplements or OTCs
Allergies: fludarabine—patient is unsure of rxn details, but woke up in the ICU after it was administered to him
Health Related Behaviors:
Tobacco—1 pack year history “during combat” (1966-68)
Alcohol—drank 1.5 fifths daily for 15 years; quit cold turkey in 1984 “on Mother’s Day”
Drugs— Never
Cardiac Risk Factors—cholesterol levels monitored annually (currently on “anti-cholesterol” med); hypertension since 50s, currently medicated by “2 or 3” antihypertensive meds; diabetes since late 40s, currently medicated by insulin and “2-3 other diabetics medications”
HIV Risk Factors—10-12 blood transfusions (11/07-4/08); no IV drug use
Occupational Exposures and Travel—worked as a welder in the Bremerton shipyards with significant exposure to asbestos; exposure to “Agent Orange” in Vietnam (1966-68) Immunizations: Influenza—annual Pneumococcal—two years ago Tetanus—current
Cancer screening tests—colonoscopy with no significant findings (KM uncertain when this was done); biannual digital rectal exam (prostate cancer)
Exercise/Diet—KM states that he tries “to watch my carbohydrate intake”); prior to the onset of his lymphoma, KM would walk 15 miles/day and enjoyed hunting and fishing—he currently follows no exercise program
Family Violence —not elicited from patient
Regular medical providers—Family Physician (Bremerton, WA) every 3
Sexual History
KM has not been sexually active “for a number of years;” he is currently unable to sustain an erection (he attributes this problem to the numerous medications he takes). In the past he has only had female sexual partners and has tested negative for STDs.
FAMILY HISTORY
- Father (d. 63): myocardial infarction; history of exposure to silo gases with significant restrictive pulmonary disease
- Mother (d. 74): stroke; history of diabetes
- 2 daughters, 1 son: no significant health problems
- brother (d. 63): myocardial infarction
- 2 brothers, 1 sister (78): history of diabetes
SOCIAL HISTORY
KM was born in 1945 in Iowa. His family moved to Bremerton in 1950, and KM has lived there ever since. KM graduated from high school in 1963, and did military service in Vietnam from 1966-1968. This was a traumatic experience for him), and so KM has been mostly retired since 1974. He attended Olympic Community College in Bremerton and earned 3 associate degrees. He also attempted to earn a bachelor’s degree at UPS, but stopped attending classes when his PTSD got overwhelming. He currently occupies himself with gardening (which he finds peaceful) and helping a local church volunteer group do home repairs; he enjoys this latter employment as he can be there when his PTSD allows it. Religion is not important to KM. His cancer diagnosis has caused him significant stress.
KM has been married and divorced three times (1964-66 with one son; 1970-77 with two daughters; and 1982-84 with no children). He currently lives alone, but receives social support (through daily visits) from his stepson and two daughters, who all live locally. His son lives in Oregon and is a physician. KM receives his health benefits through Tricare and does not describe medical expenses as a major stressor currently.
REVIEW OF SYSTEMS
Gen: positive for fatigue, night sweats (every other night related to nightmares), weight change (fluctuating gain and loss of ten pounds since initiation of chemo treatment); no fevers/chills
Derm: no pruritus, rashes, changing moles, lumps/lesions
HEENT
Head: no headaches, loss of consciousness
Eyes: positive for inflammation related to annual spring pollen allergies, wears glasses for distance vision; no vision changes, diplopia, blurry vision, pain
Ears: positive for hearing loss with bilateral hearing aids (he left them at home due to concern about losing them in the hospital); no tinnitus, vertigo, pain, discharge
Nose: no epistaxis, obstruction, post nasal discharge, sinus pain
Mouth: sees dentist twice a year no dentures, sores/ulcers, sore throat, voice changes (hoarseness), bleeding/inflamed gums
Resp: see HPI
CV: positive for chest pain (he attributes to cancer), dyspnea on exertion, orthopnea (he cannot lay flat), paroxysmal nocturnal dyspnea, peripheral edema; no history of murmur, palpitations, claudication, leg cramps
GI: positive loss of appetite, nausea/vomiting, diarrhea, constipation, changes in bowel habits (all related to chemotherapy treatments), history of hemorrhoids; no odynophagia, dysphagia, heartburn, hematemesis, jaundice, hematochezia, melena
GU: positive for occasional dysuria and urgency, nocturia (2+ nightly); no hematuria, frequency, hesitancy, incontinence, urethral discharge, sores, testicular pain/swelling
Musculoskeletal: positive for joint pain and stiffness (bilateral knees and shoulders), swelling (bilateral kness); no erythema/warmth, deformity, myalgias
Neurologic: positive dizziness (related to chemotherapy treatments); no involuntary movements, syncope, loss of coordination, motor weakness, paralysis, memory/speech changes, seizures, paresthesias
Psychiatric: positive depression, sadness, sleep disturbance (nightmares related to PTSD), crying spells, possible suicidal or homicidal ideation (KM stated “we don’t talk about that”), anxiety, hallucinations (auditory and visual); no anorexia, hyperphagia, anhedonia, loss of libido, eating disorders, delusions, behavioral changes
Hematologic: positive anemia, bruises; no bleeding
Endocrine: positive heat intolerance, polyuria, polydipsia; no cold intolerance
PHYSICAL EXAM
PE: KM is alert and sitting comfortably in a chair receiving an IV treatment
Vital Signs: BP R arm 116/62, resp 16, pulse 80
Skin: warm, dry; numerous small puncture scars in the left lower portion of his left posterior lung field; nails normal in appearance without clubbing, cyanosis or lesions
Lymph: no palpable cervical, axillary or inguinal adenopathy.
HEENT
Head: normocephalic; atraumatic, without scalp lesions
Eyes: visual acuity without glasses: 20/50 OD, 20/50 OS, 20/40 both eyes with pocket screener; fields intact to confrontation; conjunctivae non-injected; sclerae non-icteric; PERRLA; fundoscopy: red reflex bilaterally, retinal vessels–no av nicking or hemorrhages, macula appreciated
Ears: no pain on manipulation of helix or tragus bilaterally; hearing intact to normal voice tone bilaterally (rubbed finger exam not performed); TMs clear bilaterally
Nose: external nose without lesions or asymmetry; internal nose erthythematous and dry; nares patent, septum midline, no discharge
Mouth/Throat: tongue dry; uvula midline; no lesions on buccal mucosa; no pharyngeal erythema or exudate
Neck/Thyroid: neck – normal muscle strength and ROM; thyroid normal by palpation; no masses or nodules apparent
Chest: spine symmetrical without curvature; no tenderness to percussion of spine or CVAs; respiratory excursions symmetrical; lung fields clear to percussion on right side, distant breath sounds heard in left lower lobe, no crackles or wheezes appreciated.
Breasts: not performed
CV: Apical impulse not appreciated; regular rate and rhythm, normal S1 and S2, no S3 or S4, no murmurs
Pulses: carotid pulses regular; radial and femoral pulses regular and strong bilaterally, dorsalis pedis and posterior tibialis pulses present faintly bilaterally
Abdomen: central obesity; normal bowel sounds; tympanitic to percussion, non-tender to palpitation. Liver edge not palpable, but span was 8 cm by percussion; spleen tip not palpable, no masses appreciated.
Genital: not performed
Rectal Exam: not performed
MS: no obvious asymmetry or atrophy of muscles; full range of motion; joints without evident swelling, heat, erythema; 2+ edema in lower extremities
Neurologic:
Mental Status: alert, cooperative, appropriate, oriented to person, time, place
Cranial nerves:
II: vision intact (tested with pocket visual screener)
III,IV,VI: full extraocular movements
V: masseter strength normal, sensation intact to light touch
VII: face symmetrical, motor strength normal
VIII: not performed beyond hearing being intact to normal voice tone
IX,X: palate elevates symmetrically; gag not performed due to patient request
XI: motor strength normal bilaterally (trapezius and sternocleidomastoid muscles)
XII: tongue protrudes symmetrically without fasciculations
Motor Strength: 5/5 strength all major muscle groups UE and LE bilaterally
Sensation: intact to light touch and pinprick bilaterally on the hands and feet
Coordination: gait and balance steady: normal finger-nose-finger testing and heel shin testing bilaterally
Deep Tendon Reflexes: symmetrical reflexes (biceps, triceps, patellar, Achilles) 1+ throughout, plantar response down going
Summary: This is a 63 year old patient with a history of PTSD, diabetes, and hypertension who presents to the hospital for a scheduled chemotherapy regimen for his lymphoma, diagnosed six months prior to this admission. His physical examination reveals decreased breath sounds in the left lower lobe and bilateral lower extremity edema.
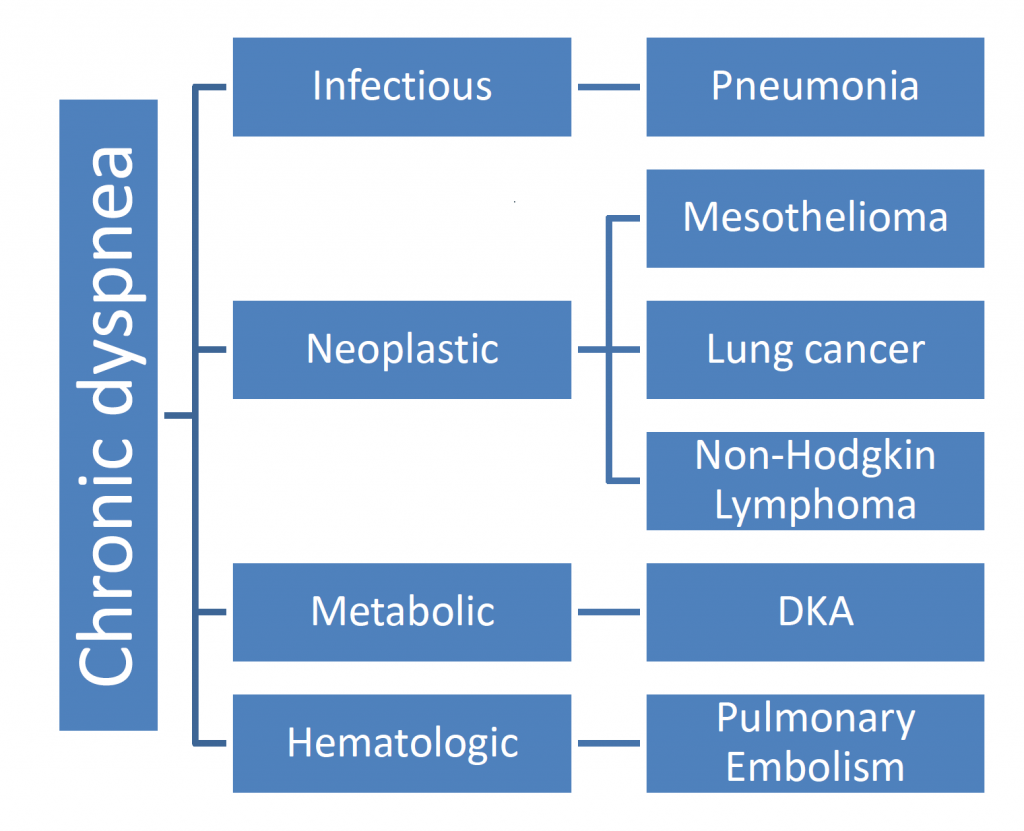
BRANCHING DIAGRAM:
ASSESSMENT:
Since KM is being hospitalized for chemotherapy treatment of his lymphoma, the differential diagnosis for progressive dyspnea at the time of his initial presentation 6 months ago will be discussed. Possible etiologies would have included pneumonia, diabetic ketoacidosis, a pulmonary embolism, or a neoplasm in his lung, in particular mesothelioma and non-Hodgkin’s lymphoma because of his exposures.
Since KM had asbestos exposure while working in the Bremerton shipyards, malignant pleural mesothelioma is on the differential. KM is 63, right within the typical age range of presentation. He had dyspnea, a common presenting symptoms of pleural mesothelioma but did not have chest pain, another common symptom. Common physical findings at the time of diagnosis include unilateral dullness to percussion at the lung base, palpable chest wall masses, and scoliosis towards the side of the malignancy. X-ray typically shows a unilateral pleural abnormality with a large, unilateral pleural effusion, which KM has had. However, thoracentesis and examination of cells can usually distinguish mesothelioma from
KM’s exposure to Agent Orange during the Vietnam War puts him at increased risk of developing non-Hodgkin’s lymphoma (NHL). The most common presenting symptom of NHL is a painless, enlarged swelling of the cervical, axilla, or inguinal lymph nodes, but NHL is localized at diagnosis only 10-20% of the time. I did not ask KM about lymph node swelling, but I did not identify any adenopathy on current physical exam. Other presenting symptoms include the classic B symptoms—fever, night sweats, weight loss, and pruritus, but can also include symptoms such as shortness of breath, chest pain, cough, abdominal pain and distention, all of which KM had.
Diagnosis can only be made by biopsy. KM did not tell me whether a biopsy was done, but we can presume it was part of his initial workup at the VA six months ago.
Since KM is diabetic, another cause for his rapid onset dyspnea could have been diabetic ketoacidosis (DKA). DKA is characterized by the rapid evolution (over a 24-hour period) of hyperglycemia, an anion gap metabolic acidosis, and ketonemia. KM had had 6 months of progressive dyspnea before the more rapid progression, though, so the rapid-onset picture of DKA doesn’t quite match his clinical picture. It is possible his slowly progressive dyspnea had another cause, but the DKA caused the rapid decline that led to diagnosis. A precipitating event, such as infection or discontinuation of insulin therapy typically precedes the onset of DKA. The earliest symptoms of marked hyperglycemia are polyuria, polydipsia, and weight loss, all present in KM. Patients with DKA may also have a fruity odor due to the exhalation of acetone, which I did not evaluate in KM).
Pulmonary embolism (PE) is another etiology for acute dyspnea. It is usually seen in patients with risk factors for venous thrombosis. These include: immobilization (positive for KM, who had experienced increasing difficulty in mobility due to his dyspnea), stroke, preexisting respiratory disease, obesity (positive in KM), hypertension (positive in KM), and cigarette smoking (negative in KM). The typical presenting symptoms for PE include: dyspnea, pleuritic chest pain, and cough (all positive for KM). Signs for PE include: tachypnea, rales, tachycardia, and S4 (I am unable to evaluate these, six months after KM originally presented). The diagnosis of PE is typically made by initially evaluating whether the patient has an elevated d-dimer. Pulmonary angiography is the gold standard for diagnosing PE, but CT scans are increasing being used to evaluate for PE (with the advantage of being able to identify other pulmonary abnormalities that could be causing the patient’s dyspnea). It is not apparent whether KM had a d-dimer measurement done during his initial clinical presentation, but his physician did do an x-ray and then sent him for CT evaluation.
Pneumonia also presents with dyspnea. Other typical presenting symptoms associated with pneumonia include: cough (positive in KM), angina, and fever. Since treatment can be successful with antibiotics, it is not surprising that KM’s physician evaluated him via physical exam when he initially presented. I can imagine that she heard dull percussion in his left lung field and sent KM for x-ray as the next logical step (an x-ray can typically rule in pneumonia).
On his initial presentation for dyspnea, a FULL respiratory physical exam that included tactile fremitus and egophony would have been appropriate to perform in addition to a complete history, that evaluated for exposure risks and elicited when his symptoms began and how they developed over time. An x-ray could have ruled in pneumonia (treatable) or cancer (sometimes treatable, but good to identify). Before sending him to radiology, his blood sugar could have been checked (cheap!), as well as bicarbonate, and d-dimer, to rule out ketoacidosis and/or pulmonary embolism etiology (recall that ketoacidosis can be brought on by an infection, so KM would have concurrently had pneumonia AND metabolic acidosis). However, since KM’s dyspnea had been progressive, cancer (or progressive heart failure—not discussed in the differential), is the most likely.