Outpatient SOAP Notes
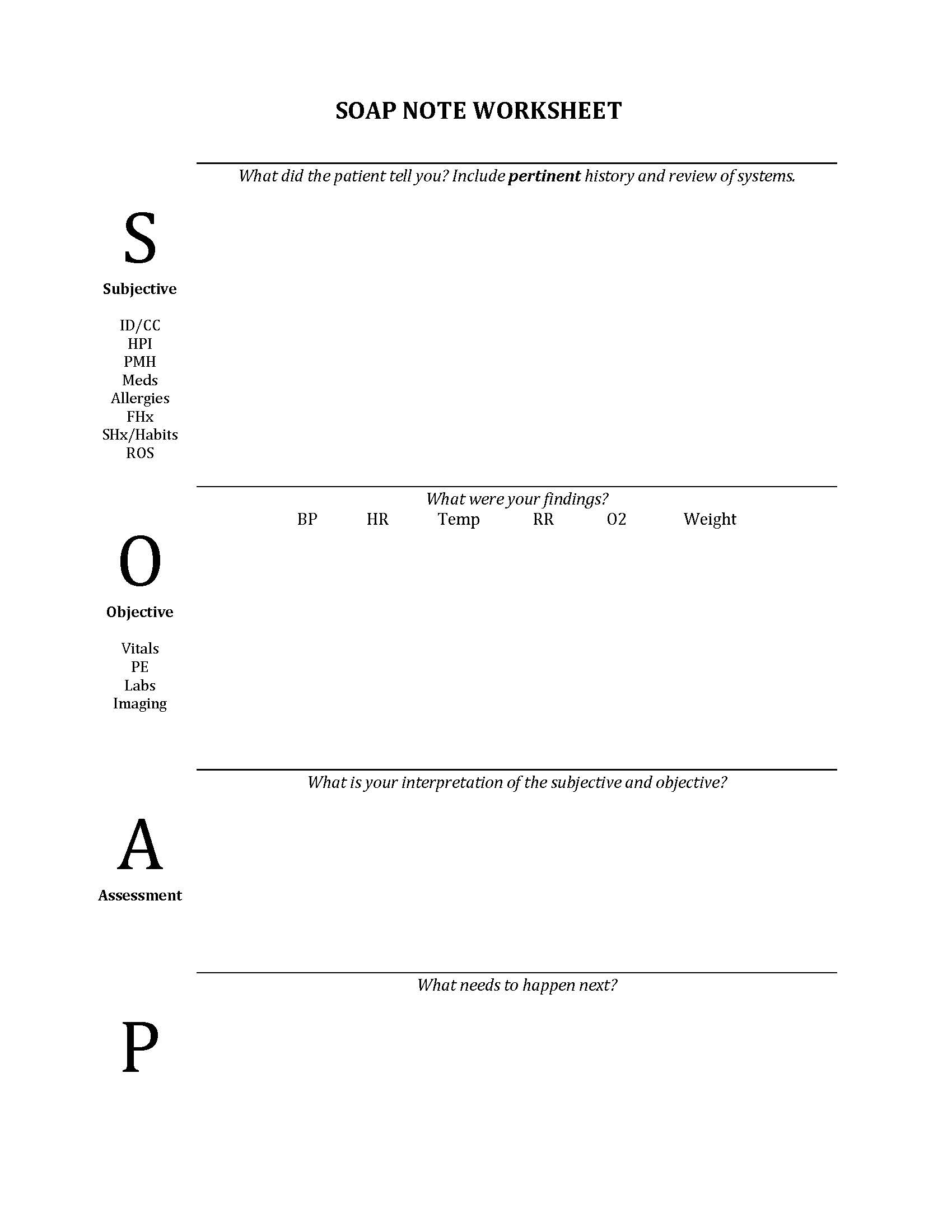
In the outpatient clinic, SOAP is the traditional note structure: S ubjective, O bjective, A ssessment, P lan. Although electronic health records may structure notes differently, this is still the information that you would enter at a problem focused or chronic disease management visit.
You may see some providers move the Assessment and Plan to the top of the note in this this order-APSO. Due to the amount of information automatically included in many electronic notes some providers chose to bring attention the the assessment and plan first.
Subjective
This section begins with ID/CC ( the reason for the scheduled visit) and includes the history of present illness plus any other pertinent history. This pertinent history is often a combination of what may have been elicited from the patient and/or information you’ve confirmed from the medical record.
If you address more than one problem at the visit, the subjective section of the note should be organized by problems, with separate paragraphs for each issue addressed. At times you will be addressing multiple and both acute and chronic medical conditions at the same visit. How to address this in the note will be discussed below.
Use the appropriate medical terms for each problem so that future readers can quickly review its history by glancing at past visit notes. Remember that most patients have access to their medical records electronically and will be reading and reviewing chart notes and telephone encounters. Be mindful about the language you use in your documentation and remain patient-centered.
If there is a separate medication list, discuss with your preceptor if you, a nurse, or the preceptor should update this. If there is not a separate medication list, the patient’s current medications should be documented in the note. Use generic names if possible and indicate strength of medication and how often patient is to take medication. This can be placed at the end of the subjective section. Remember to review allergies in case you need to prescribe any medications during the visit.
| DO INCLUDE…. | DON’T INCLUDE… |
| ID/CC: the reason for the scheduled visit | Results of your physical exam |
| What the patient tells you (symptoms, attributions, etc.) | Lab results |
| What you know to have occurred in the past ( i.e. a medication change you made over the phone, a recent visit to another provider, etc) | Impressions of the patient and data |
| Results of consults | |
| A problem-focused medical/family/social history | |
| A focused review of systems |
The objective section should include:
- vital signs
- your findings on physical exam, organized by system
- results of lab tests or imaging studies performed since the last visit.
For most visits you will perform a focused physical exam based on the problem(s) the patient is presenting with. Performing a complete physical exam in the outpatient setting usually occurs during establish care visits and occasionally during wellness visits (more often the exam is tailored to appropriate preventive health measures. e.g. pelvic exam if cervical cancer screening due, skin exam if at higher risk for skin cancer, etc). Report the presence or absence of findings pertinent to the visit’s concerns, keeping in mind your differential diagnosis. This will almost always include vital signs, general appearance and findings from more than one organ system.
Assessment
This section includes your interpretation of the information you presented in the subjective and objective sections. For an acute problem, it will be a differential diagnosis, which should include at least 2-3 reasonable possibilities. For a chronic disease visit, it should include your assessment of current control, adherence, and/or complications and any gaps or needs that were identified.
Plan
This section includes what you are going to do. When more than one problem has been addressed, many physicians write the assessment and the plan together for each one. The problems in the “assessment/plan” section correspond to those listed in the subjective section. A specific plan for follow up should be included in every note. On every note, indicate the name of your supervising physician (“seen with Dr. Jones”).
WHAT IF:
The patient has come in for a yearly wellness visit?
Update the past medical history, family, social, sexual, health related behaviors, allergies and medication list. Be familiar with the preventive health and wellness measures that are relevant based on the patient’s age, sex assigned at birth and other medical conditions or risk factors. Review any relevant screening questionnaires that may be part of the wellness visit. Often patients will bring up other acute and chronic medical conditions they would like to discuss during the wellness visit. Use agenda setting early on to identify these concerns and negotiate what can be accomplished during the visit. You may need to plan for a follow up visit to address other concerns.
WHAT IF:
The visit addresses multiple issues?
Follow the ID/CC with a statement of other issues raised by the patient or addressed by you.
“Mr. Jones is a 63 year old man with hypertension and diabetes who presents today with an acutely swollen and painful left big toe. He also requests refills on his diabetes medications and a referral for massage for low back pain.”
Organize the Subjective, Assessment, and Plan sections by problem. The first paragraph under S would address the first problem, the next would address the second problem, and so on. The assessment and plan should address each of these problems individually. In this case, the subjective and assessment sections would address:
- Acute L big toe swelling
- Diabetes
- Low back pain
- Hypertension
WHAT IF:
The visit includes follow-up of a known problem(s)?
ID/CC should include the reason for follow-up
“Mr. Jones is a 63 year old man recently diagnosed with gout in the L great toe who returns for follow-up and discussion of prevention.”
The subjective section should include for each problem:
- Interval history: what’s happened since the last visit
- History of an current status of the problem
- Current therapy, adherence and how well it is working
- Any side effects or concerns about therapy
- Any monitoring that’s due
