Key Communication Skills & Strategies
Physicians often use a directive communication style, leading with their own expertise, advice, and power. If there’s an emergency or a clear best treatment, this may be appropriate, but telling someone what to do doesn’t usually lead to change. Motivational interviewing, on the other hand, is guiding rather than directive. The clinician knows the benefits of change in preventing and treating illness. But instead of telling the patient what to do, they use strategic questions and reflections to guide the patient in finding their own ideas and motivation for change.
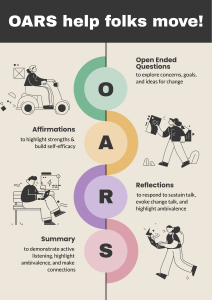
These communication techniques are already part of your toolbox, but in behavior change conversations they are used in a specific way.
- Open-ended questions are used to explore concerns, goals and ideas for change
- Affirmations are used to highlight strengths & build self-efficacy
- Reflections are used to respond to sustain talk, evoke change talk and highlight ambivalence
- Summary is used to demonstrate active listening, highlight ambivalence, and make connections
This excellent 10-minute video from the Yale/Coursera Addiction course reviews key principles of motivational interviewing and demonstrates how OARS skills are used to support these principles. These same skills and principles are applicable to any behavior change you might discuss in your PCP.
Open ended questions
In a typical interview, you’ve used OEQs to gather information and explore patient’s attribution and perspectives. Here, they are also used to explore goals and values, elicit change talk, assess stage of change, and bring out ideas for change. Here are some examples:
- To ask permission: Could we talk for a few minutes about your (behavior)?
- To explore goals and values: What are your goals for your health? Family? Work? Finances?
- To explore goals and values: What would you like your life to be like 5 years from now?
- To develop discrepancy: How does continuation of (behavior) fit in with these values?
- To assess stage of change: How likely are you to change your (behavior) in the next 6 months?
- What has worked for you in the past?
- What would you be willing to try?
- What do you intend to do?
Reflection
In a typical interview, you’ve used simple reflections to confirm what you’ve heard (sounds like…). As you saw in the video, reflection can be used in several other ways in a behavior change conversation. It may be a neutral response to patient statements arguing against change (remember this sustain talk is expected for ambivalent, contemplative patient.) Reflections respond in a way that doesn’t feel like an argument.
Because these reflections are statements rather than questions, your voice should go down at the end. This is key – if your voice goes up as if you are questioning, it completely changes the meaning and can increase rather than lessening resistance. Compare these two clips – hear the difference?
Reflection can also be used to respond to change talk, encouraging your patient to build on what they’ve already said. While simple reflections repeat or rephrase what your patient has said (sounds like…), complex reflections can deepen the conversation and move it forward.
Complex reflections may:
| Goal | Patient Statement | Sample Reflection | |
| Reframe | Suggest a new positive way of looking at something negative your patient has said – to try to help them get unstuck | I’ve tried so many times and failed | You are very persistent, even in the face of discouragement |
| Reflect Feeling | Reflect feelings that have either been stated or implied | I haven’t had my hemoglobin A1c tested in over a year, I guess I’ve been avoiding it | You’re worried what the results will be. |
| Use Metaphor | Create a picture that clarifies your patient’s position | I don’t want to take pills. I should be able to handle this on my own. | Drugs seem like a crutch to you. |
Double sided reflections
This skill is used to mirror your patient’s ambivalence about change back to them, highlighting the gap between their goals and values and their current behavior, which is also called discrepancy. Recognizing this gap can help people move towards change.
An effective double-sided reflection ends in the direction that supports change. Your patient’s response will likely follow up on the last thing that you said so this structure can promote change talk. Double sided reflections should always use the conjunction “AND” (or “at the same time”) rather than “but”. AND holds both sides of the reflection to be true, as they really are for ambivalent patients. BUT can change the feeling completely, making the patient feel like you’re skeptical rather than collaborative. Compare this example to the one above – hear the difference?
Phrases you can try out in reflections:
- It sounds like…
- What I’m hearing is…
- So you’re saying that…
- You’re feeling like…
- For you, it’s a matter of….
- From your point of view,…
- You are…
- I would imagine you…
- Must be…
- Through your eyes,…
- Your belief is that…
- Your concern is that…
- It seems to you that…
- You’re not terribly excited about…
- You’re not much concerned about…
- The thing that bothers you is…
- The important thing as you see it is…
Summary in behavior change conversations
As in other interviews, summary demonstrates active listening and allows the patient to reflect on what you’ve discussed, correct misunderstandings, or add new information. In behavior change conversations, summary can also be used to reflect underlying meaning and feelings, highlight ambivalence, and help your patient make connections between things that they’ve discussed.
- A collecting summary brings together several related things that the patient has talked about.
“So your strengths as a parent include a lot of patience, true enjoyment of playing with your kids, and setting clear boundaries”
- A linking summary may help the patient see connections between something they’ve said and an earlier conversation.
“Earlier you said you wanted to think about cutting back on alcohol and you’re also noticing difficulty with sleep.”
- A transitional summary marks and announces a shift, often at the end of the visit.
An example
You saw this video of Ron Jackson and Joe Merrill in the Substance Use chapter. Now watch through the lens of motivating change – Ron uses open-ended questions, reflections and summary to guide Joe in identifying his own reasons and plans for change, as well as a couple more techniques that you’ll see in the next chapter.