Applied Neurologic Exam
After the Advanced Neurologic exam workshop, you should be able to:
- Perform the Immersion Neurologic exam and interpret your findings
- Recognize and interpret common abnormal findings
- Perform hypothesis-driven exam maneuvers
- Assess muscle tone
- If you suspect cognitive impairment, perform the Mini-Cog
- If you suspect a disorder of the eye or visual pathways, test visual fields.
- If your patient reports sensory changes, assess multiple sensory modalities
Findings to recognize and interpret
Mental status
Decreased level of consciousness
Normal LOC is defined as alert. Decreased levels of consciousness are:
- Lethargy: Patient is sleepy, requiring stimulation to maintain an awake state.
- Stupor: Patient cannot be aroused to a fully awake state but may respond semi-purposefully to stimulation.
- Coma: Patient demonstrates no purposeful response to any type of stimulation.
Abnormalities of language or speech:
- Aphasia is a disorder of language caused by stroke and other brain disorders affecting the language areas of the cortex. It manifests as problems with comprehension, fluency, naming, arithmetic and/or writing. You will learn more in the section on Communication in Disability.
- Dysphonia is a disorder of speech, specifically voice production caused by abnormal larynx or vocal cord function.
- Dysarthria is a disorder of speech, specifically articulation caused by abnormal motor control of the pharynx, palate, tongue, lips and/or face.
Cranial nerves
Anisocoria (unequal pupils)
Pupillary size is determined by the balance of parasympathetic and sympathetic input. The parasympathetics constrict the pupil and arrive at the eye via CN III. The sympathetics dilate the pupil and arrive via the nerve plexus along the internal carotid artery.
To determine the cause of unequal pupils, compare the degree of asymmetry in light and dark. If the degree of asymmetry is:
-
- The same in light and dark: The patient has physiologic anisocoria, a normal variant occurring in 20% of the population. An old photo can confirm it’s longstanding
- Greatest in light: The patient has a parasympathetic problem in the larger pupil. Look for other signs of CNIII dysfunction, especially EOM weakness
- Greatest in dark: The patient has a sympathetic problem in the smaller pupil. Look for other signs of Horner syndrome, decreased facial sweating and ptosis.
Extraocular muscle weakness.
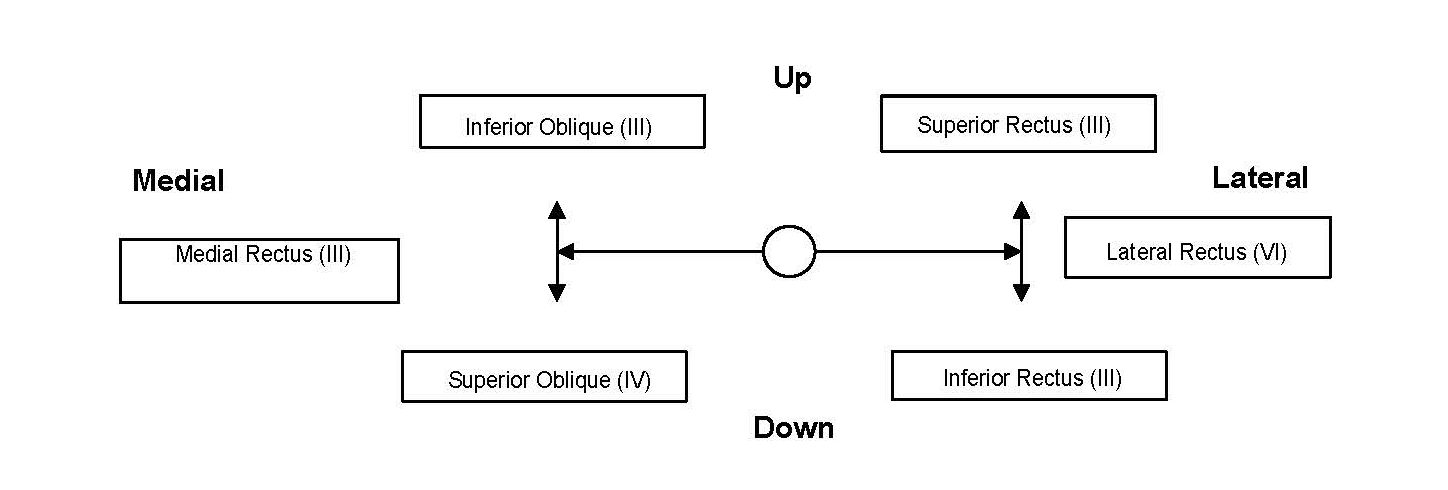
You may identify this on exam or your patient may report of diplopia with EOM testing. Diplopia can indicate more subtle weakness than you can see. The muscles responsible for movement in each of the 6 cardinal directions is shown below, for the left eye.
Facial weakness.
Unilateral facial weakness can be caused by either a central or peripheral lesion of the 7th cranial nerve. These can be differentiated by how much of the face is involved. The motor neurons innervating the forehead receive input from both sides of the brain, while those innervating the lower face receive input only from the contralateral brain. A peripheral facial nerve lesion (Bell’s palsy) causes weakness of both the upper and lower face. A central facial nerve deficit, which is usually caused by stroke, will affect only the lower face.

Facial nerve paralysis – Wikimedia Commons
Tongue weakness.
Each genioglossus muscle pushes the tongue out and to the opposite side, so the tongue deviates to the side of weakness. Unilateral atrophy and twitching are also signs of weakness.
Motor system
Increased tone
There are two types of increased muscle tone: rigidity, which is caused by extrapyramidal disorders like Parkinson’s disease, and spasticity, which is caused by central nervous system disease. Rigidity can be an early and diagnostically useful finding in Parkinson’s and other extrapyramidal disorders. Patients with spasticity usually have other findings of upper motor neuron disease, like weakness and upgoing toes. In this short video, Dr. Kraus differentiates the two.
Hypothesis-driven exam maneuvers
If you suspect cognitive impairment, perform the Mini-Cog.
- Give your patient a list of three items like Apple-Penny- Ball. Ask them to repeat immediately and remember them for 5 minutes.
- Give the patient a piece of paper with a circle drawn on it. Instruct them to draw a clock, placing the numbers on the clock face, with the hands pointing to a certain time. Then ask them to recall the 3 items.
- Three item recall and mini-Cog (for more on scoring the Mini-Cog)
- Recall of 0 items indicates cognitive impairment.
- Recall of 1-2 items with an abnormal clock face indicates cognitive impairment.
- Recall of 1-2 items with a normal clock face indicates no cognitive impairment.
- Recall of all 3 items indicates no cognitive impairment.
If you suspect a disorder of the eye or visual pathways, test visual fields.
Abnormal visual fields can be caused by problems anywhere along the visual pathways. Here’s a recap of Dr. Kraus describing and demonstrating.
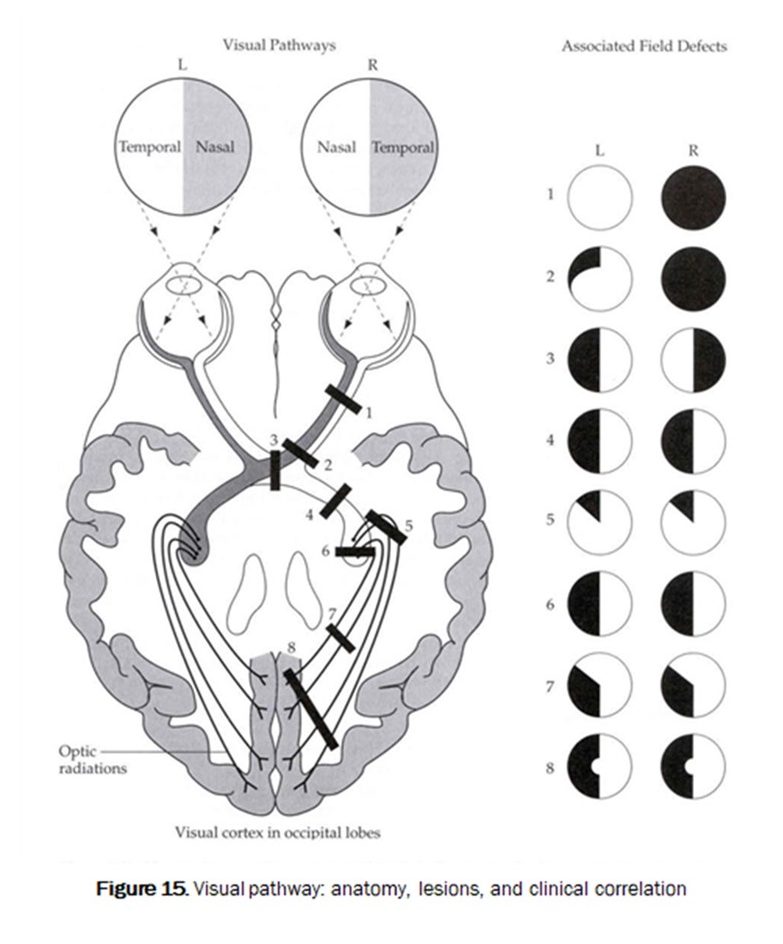
Lesions at different locations cause characteristic patterns of visual field loss. Diseases localized to the eye can cause loss of peripheral vision (as in glaucoma) or complete loss of vision in that eye. Optic nerve lesions, pituitary tumors that compress the optic chiasm, and brain lesions lead to different patterns of visual field loss.
If your patient reports sensory changes, assess multiple sensory modalities:
The goal of a more detailed sensory exam is to localize the abnormality to an anatomic site.
- Light touch and pinprick are carried in the spinothalamic tract. Break a clean cotton swab in half. Use the soft tip to assess light touch and the sharp handle for pinprick.
- Vibration sense is tested with the 128 Hz tuning fork.
- Proprioception is tested by moving the joint.
Clues to localization of the problem:
Brain or brainstem. Findings include sensory loss in large parts of one side of the body that can’t be explained by a single nerve or dermatome. Light touch and pinprick are good modalities to test, looking for symmetry from side to side.
Spinal cord. Findings include a sensory level on the trunk and asymmetric findings of vibration/proprioception loss on one leg with pinprick loss on the other. Light touch, pinprick, vibration and proprioception are good modalities to test in the legs. Light touch and pin are good modalities to find a sensory level on the trunk.
Peripheral nerve. Findings include a length-dependent sensory loss or sensory loss in small parts of one side of the body that can be explained by a single nerve or dermatome. Light touch, pinprick, vibration and proprioception are good modalities to test for a length-dependent process. Light touch and pin are good modalities to find a focal nerve process.
Putting it all together: Localization
When patients present with neurologic symptoms, your exam is used to localize the cause of their findings, which could range from the brain to the neuromuscular junction. Localization narrows the differential diagnosis and directs next steps in testing. Here, Dr. Kraus gives an overview.
Resources & references
https://edtech.westernu.edu/3D-eye-movement-simulator/
