Immersion Abdominal Exam
After Immersion, you will be able to:
Inspection
- Observe your patient for increased discomfort with movement.
- Inspect the abdominal contour, observing for distention or masses.
- Inspect the skin as you examine the abdomen, noting scars and skin lesions
Auscultation
- Listen in one place with the diaphragm of the stethoscope until you hear bowel sounds.
Percussion
- Percuss all four quadrants, observing for tenderness and tympany
- Percuss the upper and lower liver margins in the R mid-clavicular line
Palpation
- Palpate all 4 quadrants for tenderness or masses
- Palpate the lower liver edge
- Palpate for an enlarged spleen
Key landmarks & structures
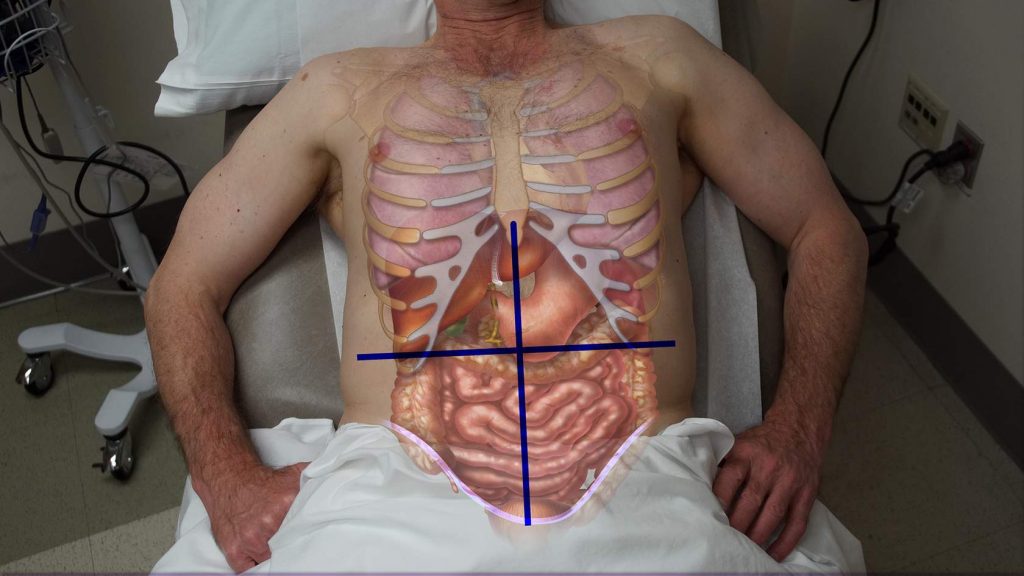
Identify the four quadrants of the abdomen and consider the organs that are found in each one.Tenderness that localizes to one quadrant suggests a different set of diagnoses than pain in another quadrant.
Imaginary lines cross at the umbilicus, dividing the abdomen into right upper, right lower, left upper and left lower quadrants. The liver and gallbladder are in the right upper quadrant (RUQ). The stomach is in the LUQ, with the spleen behind it. The colon is the large tubular structure below, which loops from the RLQ, up to the RUQ, across to the LUQ, and down again to the LLQ.
 |
 |
-
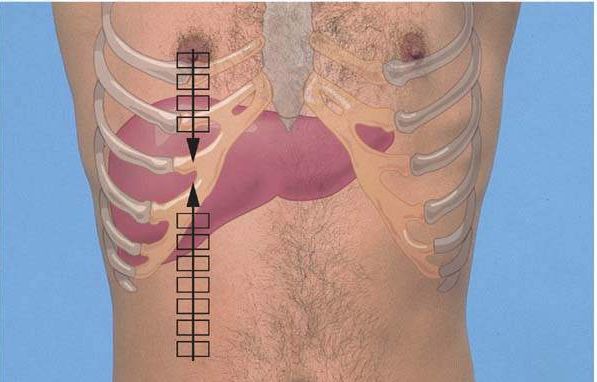
- Craniocaudal: from just below the diaphragm to the right costal margin
- Side-to-side: from the right chest wall almost to the left midclavicular line
Preparation and Positioning
Stand on the right side of your patient, who should be supine and double draped so only the abdomen is exposed.
To relax the abdominal muscles and improve the quality of the exam, your patient’s head should be supported by a pillow, their knees should be slightly flexed and their hands should be on the chest or by their sides. Your hands should be warm and any painful area of the abdomen should be examined last.
Inspection
Observe the contour of the abdomen for distention. Note any scars.
Auscultation
In contrast to other organ systems, auscultation is done before palpation and percussion. Palpation might increase intestinal motility despite a serious illness and falsely reassure the examiner.
Normal bowel sounds are gurgling, lower pitched, and vary over time and from person to person. The frequency is anywhere 4-34/minute. Keep your stethoscope handy and listen to your own bowel sounds before and after a meal and at other times during the day. To say that bowel sounds are truly absent, you must listen for two minutes. Absent bowel sounds suggest a serious intra-abdominal problem.
Percussion
Percuss all four quadrants assessing tympany.
The normal abdomen is tympanitic to percussion over gas-filled bowel and dull over areas filled with fluid or stool. Your findings may shift and change with time and movement of the contents of the stomach and intestine. Masses are also dull to percussion and will not change.Percussion may also elicit tenderness in a patient with abdominal pain.
Percuss the liver.
Percuss along the R MCL from the mid-abdomen up toward the liver. The transition from tympanitic to dull estimates the lower edge of the liver. If your exam partner is comfortable, you can also percuss the upper edge of the liver. Begin in the mid-thorax and percuss along the R MCL down toward the liver. The normal liver span on percussion is < 13 cm.
Palpation
Palpate all four quadrants.
Position your patient flat on their back, with the knees bent to relax the abdomen. Start with light palpation, using the flat part of the hand and the pads of the fingers. Lift the hand to move it from one point to another, to avoid tickling your patient. If the patient has pain, palpate the painful area last.
Next palpate more deeply, to detect any masses. Place your non-dominant hand on top of the dominant hand, using the top hand to push the examining hand inwards.
Palpate the liver edge.
Place your right hand on the abdomen in the R mid-clavicular line, below the inferior border of the liver you found by percussion. Ask the patient to inhale as you feel for the liver edge coming down to meet your fingertips. If you don’t feel it, move your fingers 2 cm up and repeat until you reach the costal margin.
The liver edge may be palpable just at the costal margin or may not be palpable at all. In patients with hyperinflated lungs, the normal liver edge may be felt lower down.
Palpate for an enlarged spleen.
Reach across the patient’s body. Place your left hand under the patient’s lower left rib cage and lift slightly. Palpate for the tip of the spleen with your right hand. If you suspect splenomegaly, begin at the level of the anterior iliac crest and move up – the enlarged spleen can extend to the pelvis and into the right lower quadrant.
The normal spleen is not palpable in adults but may be palpable in some healthy children.
Sample documentation:
Abdomen: No scars or distention. Active bowel sounds present. Minimal tenderness to deep palpation in the left lower quadrant without palpable masses. Liver span 9 cm to percussion at the mid-clavicular line, with non-tender, soft edge palpable at the right costal margin with deep inspiration. Spleen not palpable. No inguinal adenopathy.
