Trauma informed physical exam
Over the course of their lives, many people have experienced significant trauma, such as abuse in childhood, racism and oppression, witnessing or experiencing violence, and parental separation. A growing body of research shows that trauma has many long-lasting health impacts, increasing the need for health care.
Unfortunately, adverse childhood experiences and trauma can also impact your patient’s feeling of safety during the physical exam. Failure to recognize this can lead well-meaning health care providers to inadvertently re-traumatize their patients, decreasing trust and quality of care. The physical exam can be particularly stressful, and fear and anxiety about the exam can lead some patients to avoid healthcare altogether.
Trauma-informed care emphasizes physical, psychological and emotional safety, to help survivors of trauma rebuild a sense of control and empowerment. Use a trauma- informed approach to the physical exam with all patients to maximize comfort and trust for all patients. Your goal is for patients to feel that they have control throughout the exam.
|
The 4 Rs of Trauma Informed Care |
||
|---|---|---|
| R | ealize the widespread impact of trauma | Over half of people have experienced some type of trauma, and the incidence is still higher in some communities and populations. The long term effects vary person to person. |
| R | ecognize the signs and symptoms | Common clues are avoiding certain exams or signs of anxiety during the exam, which may vary across individuals and cultures. |
| R | espond by integrating knowledge into practice | Commit to learning about various forms of trauma and adapt the care that you and your team provide to the needs of your individual patient and the community that you serve. |
| R | esist re-traumatization | Use a trauma informed approach to the exam with all patients and adapt exam techniques to accommodate the needs of individual patients. |
 |
Before the exam
|
|
During the exam
|
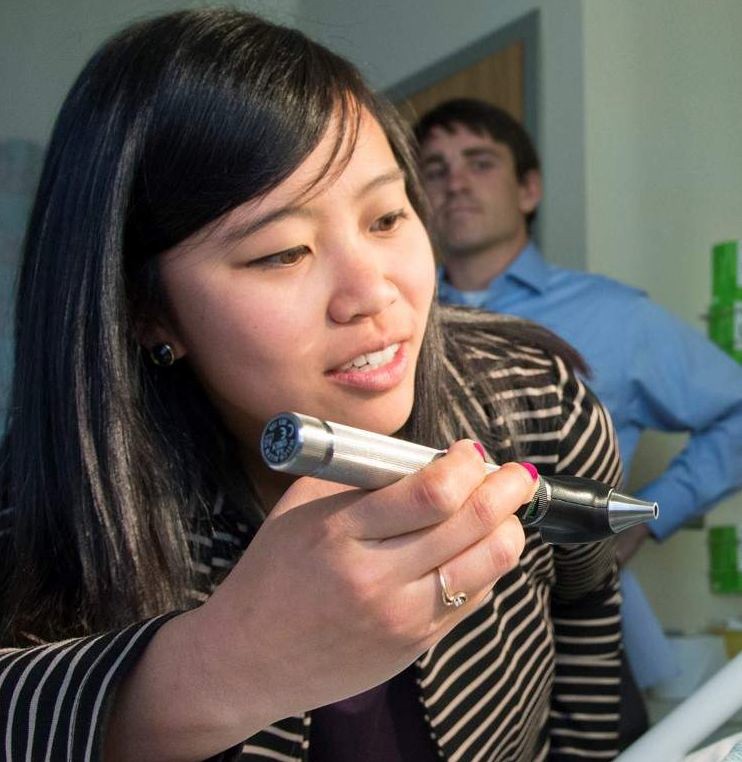 |
Also be aware that some exam elements may feel especially threatening to those who have experienced trauma. The oral exam, the thyroid exam, and the male and female GU exams are examples. Be sure to explain what you will do and why, and ask the patient’s permission. Because of the power differential inherent to the physician patient relationship, some patients may feel uncomfortable speaking up, so in FCM, you can explicitly tell patients that it is okay to decline any aspect of the exam if they are uncomfortable.
