Chronic Disease Management Visits
A chronic disease is a health problem that requires ongoing management over years or even decades. Many clinic visits focus on chronic disease management occur in both primary and specialty care settings. Your approach to these visits is not about a differential diagnosis. It is about how well the disease is managed, how it is impacting your patient’s life, and how you can work together to optimize control while minimizing the side effects of treatment. The purpose of a chronic disease management visit is to assess and update the status of the illness, identify any complications, and adjust treatment if needed.
Impact of Chronic Illness
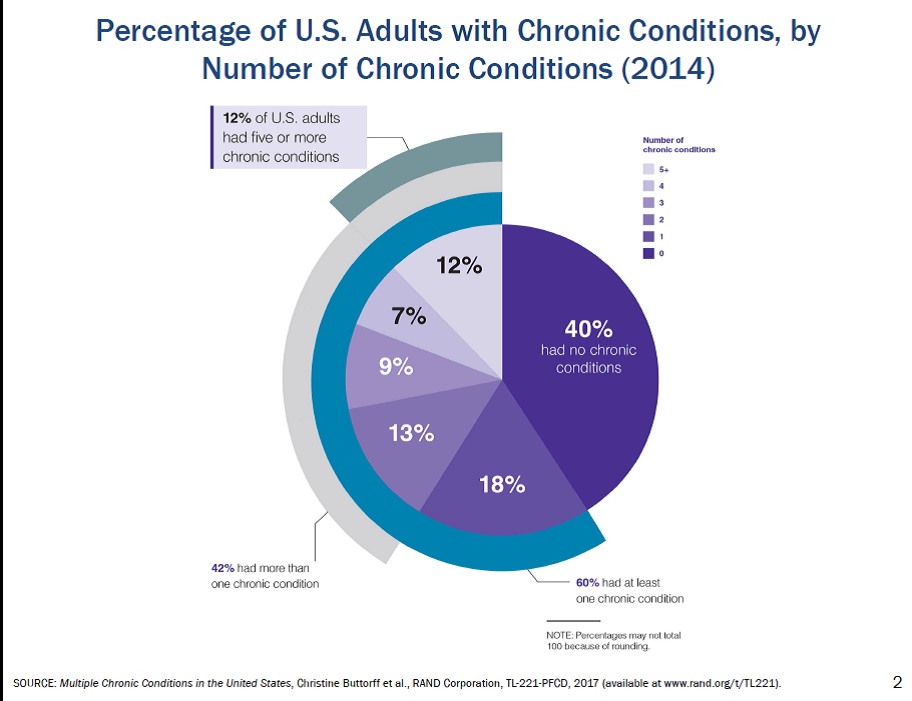
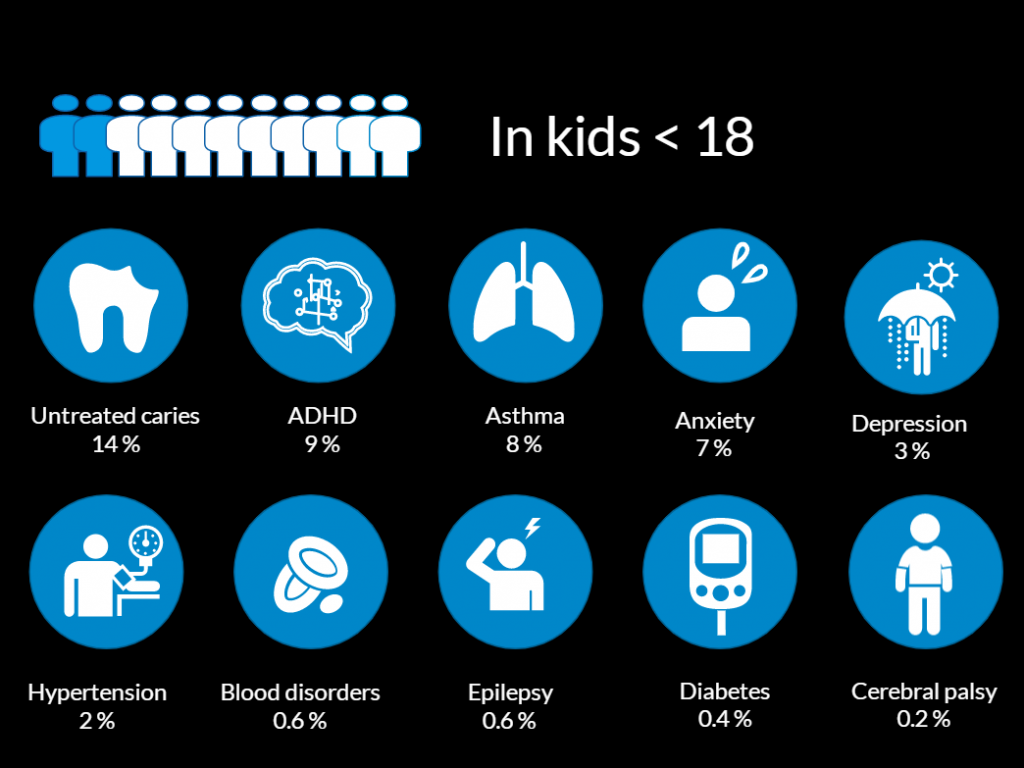
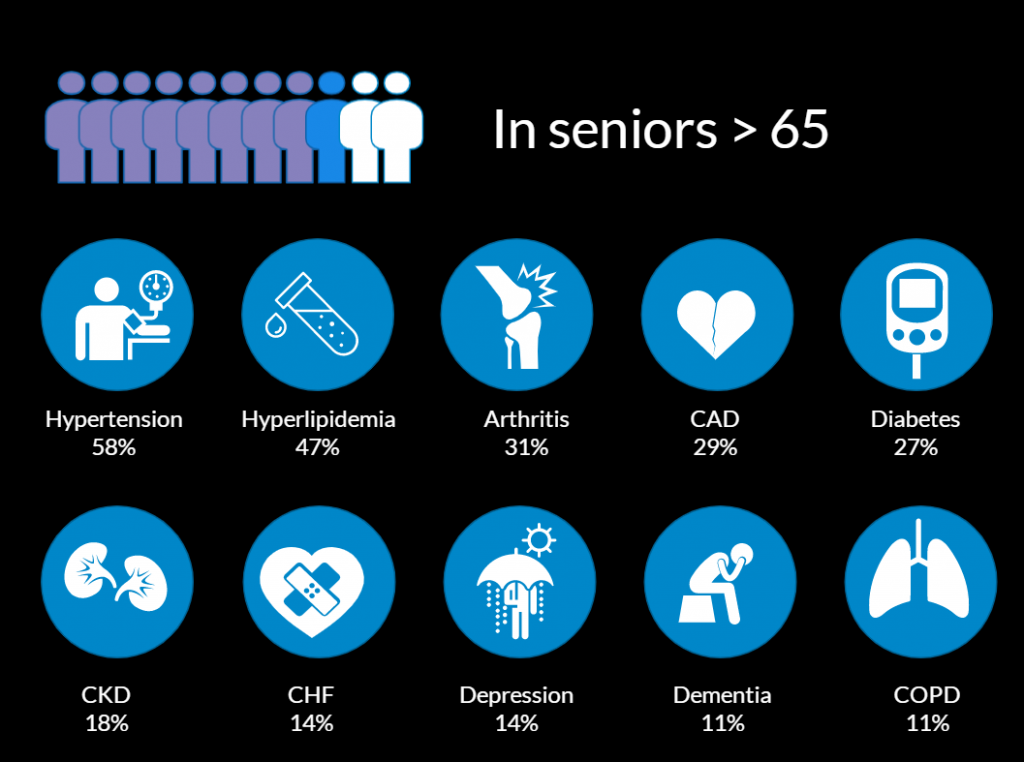
60% of American adults have at least one chronic illness and 12% have 5 or more. Seniors carry the heaviest burden with 8 of 10 living with one of these chronic illnesses and most have more. The prevalence of chronic illness is lower in children under 18. Untreated dental caries affects the most kids and is the most frequent cause of law school days.
No matter what the illness, our goal at the end of the visit is a patient armed with the knowledge, skills, resources and support to take care of themselves at home. Research shows that this ability and willingness to manage one’s own health, often called patient activation, is associated with getting better control of the disease they already have and getting fewer new ones. Working collaboratively with our patients can increase their activation, giving us a chance to make a real impact during a chronic disease visit. Strategies like collaborative agenda setting, tailoring education, using ask-tell-ask, motivational interviewing and negotiating rather than dictating a plan have been shown to increase a patient’s willingness to really take on their chronic illness.
Patient activation
- Better control of chronic illness
- Fewer hospitalizations
- Fewer new chronic illnesses
- It can be changed!
- Agenda setting
- Ask-tell-ask
- Motivational interviewing
- Negotiating a plan
Problem Focused History
The problem focused history for chronic illness should explore how well our patient is able to manage their illness at home and how the health care team can support them in their self-care. Following elements are key to all chronic disease management visits. Each section will be explored further below.
Components of a chronic care visit
Background: onset of illness, current prescribed treatment, and any complications.
Interval history: symptom control, self monitoring, visits with other providers, tests, hospitalizations
Treatment adherence: medications, health behaviors, other interventions
Functional status: activity tolerance and ADLs, quality of life
Social support & psychosocial concerns
Patient goals
You want to start with a little bit of background; the onset of the illness, current prescribed treatments, and any complications. You may be able to review this in the patient’s medical record or you may need to elicit this history.
Background
- Onset & course
- Date of diagnosis
- Recent evaluation
- Prescribed treatment
- Complications
Baseline health status
Get a really good picture of how things have been going at home since the last visit. Try to understand the impact of the illness on their lives. How well of any symptoms have been controlled. What has self monitoring shown? Things like home blood pressure measurements in patients with hypertension, daily weights in patients with heart failure, blood sugars for patients with diabetes, or peak flows in patients with asthma. Have there been any visits with other providers, testing, hospitalization, and what’s their understanding of their illness?
Interval History
- Impact on daily life
- How well have any symptoms been controlled?
- Self monitoring and results
- Visits with other providers
- Understanding of their illness
Treatment adherence
It’s critical to explore how your patient is doing with treatment, both medicines, other interventions, and healthy behavior. Non adherence to medication is incredibly common, estimated at 50% across the board and is even higher for medications for asymptomatic problems like hypertension or hyperlipidemia. There are so many potential barriers to adherence from the individual level up to the systems level. Understanding your patient’s adherence and identifying their barriers can help you and your patient come up with strategies to improve it.
Treatment & adherence
- Barriers to adherence
- Individual: memory issues, side effects
- Interpersonal: caring for others, work responsibilities
- Community & institutions: complex drug regimens, refill delays
- Public policy: co-payments, insurance coverage of consultations with other professionals
Functional Status
People with a chronic illness spend an average of 6 hours a year in their doctor’s office and another 8,756 hours at home monitoring their health, taking medications, and engaging in healthy behavior or not.
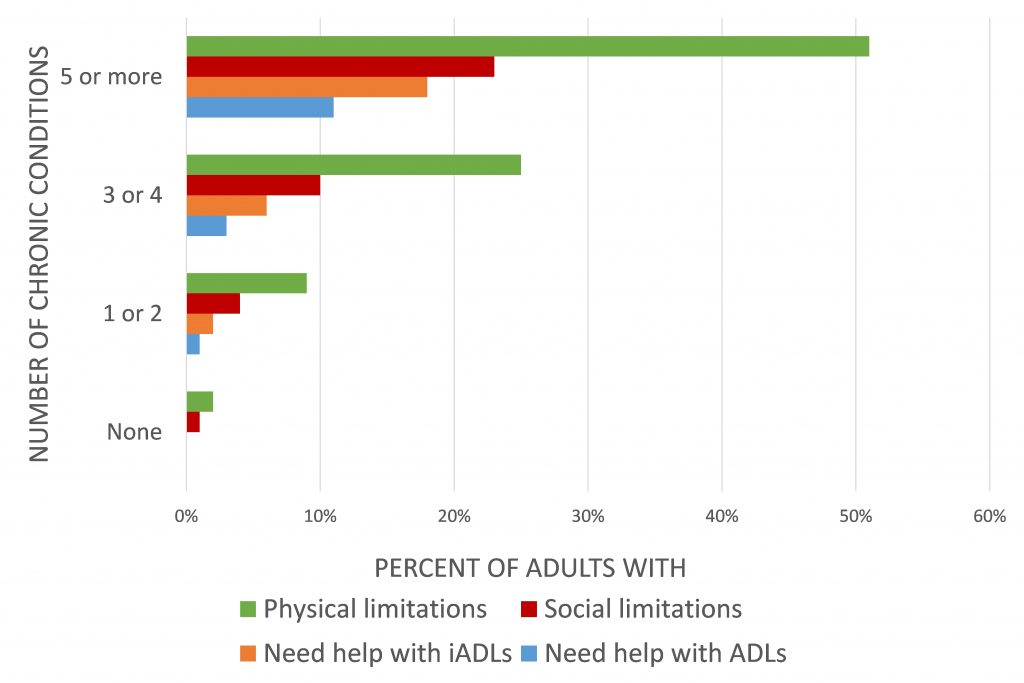
Ask about functional status, especially with patients who have multiple chronic illnesses. Regardless of their age, patients with multimorbidity are at risk for physical, cognitive and social limitations that can really affect their quality of life and their ability to manage their illness. Check in about social supports, plus any psychosocial problems or concerns. Relationships and social roles can really help or get in the way of patient self-management. If something has changed at home that may well be the reason for worsening control. Revisiting and expanding the social history, exploring the patient’s strengths, their responsibilities, stressors, finances, and insurance is especially important when things aren’t going the way you had hoped.
Social support & psychosocial concerns
- Strengths
- Responsibilities
- Stressors
- Finance & insurance
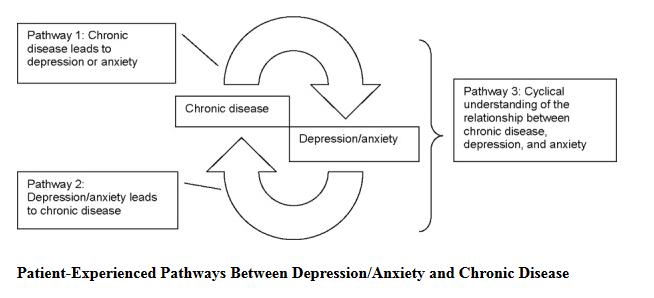
- Mood disorders
Depression is more common in patients with many chronic illnesses than in the general population so regular screening should be incorporated into chronic disease visits either with a clinic administered questionnaire like the PHQ-2 or PHQ-9 or a few questions in your history. Finally, don’t forget to ask about your patient’s life goals like upcoming travel, or supporting a spouse, or for their chronic illness specifically. Knowing these goals and priorities can help you and your patient develop a treatment plan that will work for them.
Physical Exam for Chronic Illness
The exam can help us answer two questions. How well is the disorder controlled and is the patient developing complications.
The exam maneuvers you do will be disease specific. For example:
- COPD: pulmonary exam
- Congestive heart failure: weight, complete heart and lung exam, JVP
- Rheumatoid arthritis: musculoskeletal exam
The examination may focus on whether the patient is developing complications from the chronic illness. For example:
- Diabetes: screening for neuropathy or retinopathy
- Alcohol use disorder: abdominal exam to evaluate the liver, look for ascites, check for leg edema
Assessment
Your assessment will focus on how well the illness is controlled and where it seems to be heading. Include the goals that you and your patient are working toward and comment on any barriers to optimal control that you’ve picked up on.
Plan
The plan for a chronic disease management has the same 4 elements as other visits, emphasizing education to optimize your patient self-care at home.
- Diagnostic tests
- Treatment
- Education
- Follow up
Diagnostics includes any test planned for today or before the next visit.
Examples:
- Laboratory tests
- Hemoglobin A1c in diabetes
- Chem 7 after increasing diuretic doses, starting and ACE-inhibitor in heart failure management
- Imaging
- Functional testing, e.g. repeat spirometry in COPD
Therapy includes both medication and behavior change that address the illness.
Examples:
- Medications
- Stop hydrochlorothiazide and start furosemide 20 mg twice daily
- Health Promoting Behaviors
- Self-monitoring
- Medication adherence
- Diet, exercise, substance use
Education is the key you may be able to do some during a visit but most patients with a chronic illness would benefit from more than we can do in a 15 minute follow up. Getting to know the other health professionals in your clinic and their role in caring for patients will help you come up with the best plan possible.
Education by you and your PCP and other health care professionals, e.g.
- Registered nurse
- Pharmacist
- Dietician
- Social worker
- Other team members
In many clinics, a registered nurse takes the lead on chronic disease education either with individual patients or with groups. Pharmacists are of course the medication experts. They have a lot of strategies that can improve adherence from motivational interviewing, simplifying drug regimens, to developing reminder systems. Dietitians are experts in nutrition education and motivation. Social workers can help address addiction, finances, stressors, and other barriers to care.
Follow up includes referrals to other providers and when they’ll come back to see you. It may also include community resources like the YMCA diabetes prevention program or support groups for patients with the same illness.
The management of chronic illness is the cornerstone of primary care medicine. Learning the approaches above will help you more successfully navigate these visit types in your Primary Care Practicum.