Eliciting Change Talk
Motivational interviewing helps people to talk themselves into a change that they have identified as important. Change talk builds self-efficacy and makes any change more likely to stick. It may be spontaneous or be prompted by a question; either way, follow up with OARS to try to draw out more.
The mnemonic ‘DARN CAT’ can help you elicit and recognize change talk. DARN statements suggest your patient is contemplative. CAT statements, which are usually spontaneous, suggest readiness to make a plan.
This communication technique highlights the ambivalence of people who are contemplating change. Asking about the pros of the current behavior acknowledges the difficulty of change up front and makes your patient feel heard. Sample questions for exploring pros:
- What are the good things about…?
- What are some of the things you enjoy about…?
- What do you like about…?
- What are the good things about…?
After the first response, you could ask again about pros, repeating until there is nothing more to add.
When asking about the cons of the current situation, use words like “enjoy less” or “not so good” rather than “bad”. People at the pre-contemplative stage are often not thinking about negative consequences, so it may be easier for them to agree to ‘less good’. Sample questions to elicit cons:
- What are some of the not-so-good things about…?
- What concerns do you have about …?
- What worries you about …?
- What are some of the things you enjoy less about…?
- What problems have you had so far?
- What do you think will happen if you don’t quit…?
If your patient has mentioned a specific change that they’re considering, you can also explore the cons and finally the pros of the healthier behavior. This order is important: you want to end on the good that could come of change so your patient can build upon that. To wrap up the pros and cons, use a double-sided reflection or summary, again ending in the direction of change.
A simple way to explore pros and cons is with these two questions:
- First: What are the good things, and the not-so-good things about…
- Then: When you think about changing what would be hard, and what would be best?
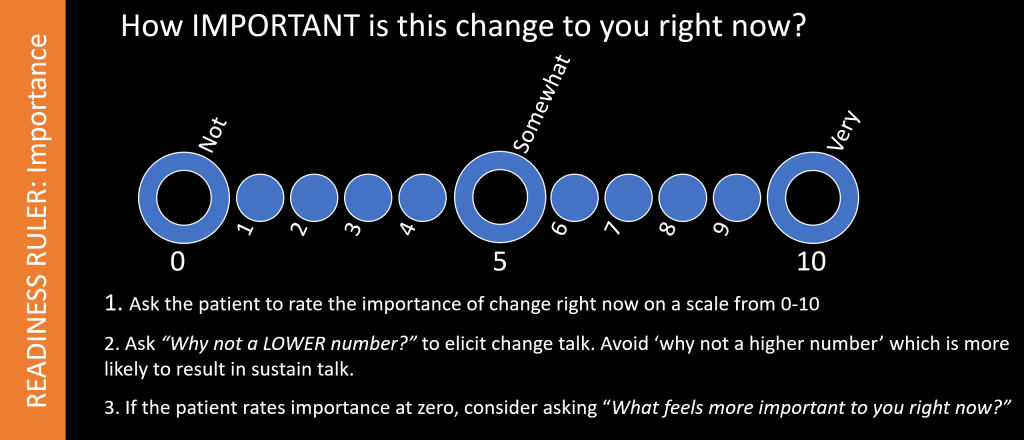
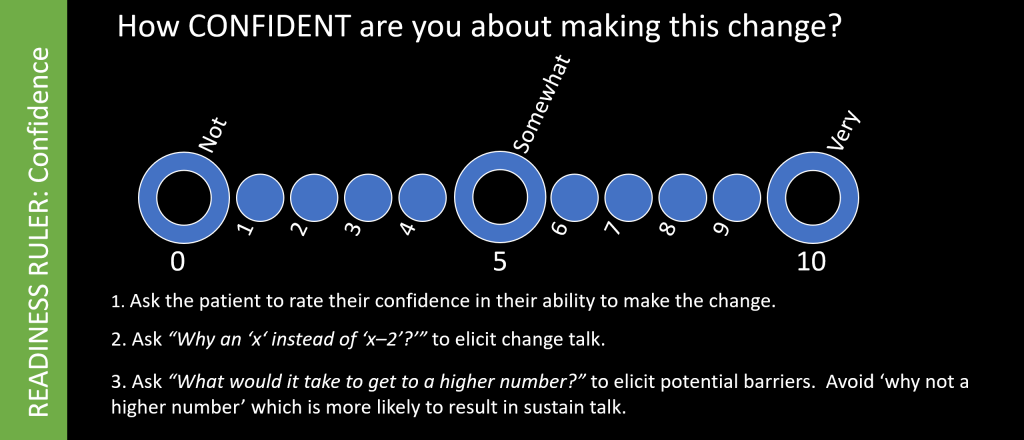
Readiness Rulers
This technique assesses readiness to change, which is a product of a belief that the change is important, and confidence that one can succeed. Rulers can also elicit change talk and uncover barriers that you can address.
Example:
You ask: “On a scale of 0 to 10, with 0 being not-at-all important and 10 being extremely important, how important is it to you to add some exercise to your life right now?”
The patient answers “4/10”.
To elicit change talk, you ask “Why a 4 and not a 2?”
They respond that they feel better when they exercise.
You respond with a reflection (You feel better when you’re exercising) or open-ended question to amplify or elicit more change talk.
Example:
You ask: “On a scale of 0 to 10, with 0 being not-at-all and 10 being very confident, how confident are you that you can quit smoking?”
The patient is 7/10 confident.
You ask “Why a 7 and not a 5?” They respond that they’ve done it before.
You ask what it would take to get to a 9, and they share they’d need something to help manage anxiety.
You’d respond to this information with affirmations, reflections, and open-ended questions.
- To build self-efficacy: “You‘ve quit smoking before! What worked last time?“
- To elicit more change talk: “Quitting has felt important for a while.”
- To address barriers: “What thoughts do you have about managing anxiety?” “Tell me more about times when anxiety drives your smoking?”
Compare the 5-minute video below to the snippet you saw in the introduction. In the first video, the physician used a more directive style, the conversation became confrontational and it ended without progress toward change. In the second example, the physician uses a more collaborative style and calls on motivational interviewing techniques – you can see this conversation guiding the parent toward change. This is what you are aiming for!
Clinicians also elicit change talk in the action and maintenance phases, to support self-efficacy as the patient builds and consolidates new habits. This 4-minute video from the FIU School of Medicine shows a PCP and patient collaborating around behavior change in diabetes. This patient has already made some significant changes, and the visit ends with a plan to build on those next time.