Lumbar spine (Benchmark exam)
Benchmarks for a problem focused exam of a patient with low back pain include:
Inspect: From the back and the side, observing spine curvature, muscle bulk, and symmetry of hip and shoulder height
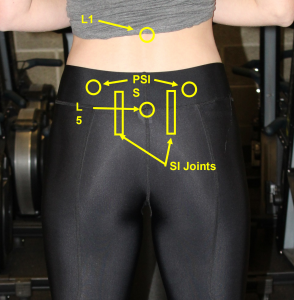
Palpate: Observing for tenderness, spasm, and asymmetry:
- Vertebrae from L1 to the sacrum
- Paravertebral muscles bilaterally
- Sacroiliac joints
Range of motion: Assess flexion, extension, lateral rotation, side bending
Neurovascular testing: To assess for compression of nerve roots or spinal cord, test
- Lower extremity strength
- Lower extremity reflexes
- Lower extremity sensation
Stability and special tests as directed by the differential:
- If you suspect lumbosacral radiculopathy, perform
- Straight leg raise and crossed straight leg raise
- Slump test
- If you suspect spondylolysis, perform the Stork test.
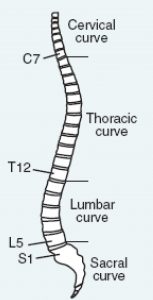
Key landmarks & structures:
Start by identifying each of the following structures, which will guide you as you perform the exam and document your findings.
Inspection
- Curvature of the spine.
- From behind, any lateral curvature of the spine is abnormal and suggests scoliosis.
- From the side, you should expect to see typical lumbar lordosis
- Muscle bulk should be symmetric side to side.
- Swelling, erythema or ecchymosis suggests trauma or infection.
- Asymmetry of hip or shoulder height suggests scoliosis or leg length differences.
Palpation
Palpate the low back, carefully noting any structures that are tender or asymmetric.
- Vertebrae from L1 to the sacrum
- Paravertebral muscles bilaterally
- Sacroiliac joints
Range of Motion
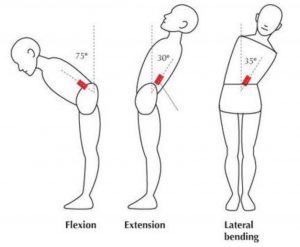 Test range of motion in 4 directions. Normal range of motion for the lumbar spine is:
Test range of motion in 4 directions. Normal range of motion for the lumbar spine is:
- Flexion: 60 to 90 degrees
- Extension: 25 to 30 degrees
- Lateral rotation (twisting): 25 degrees
- Lateral bending: 25 to 35 degrees
Neurovascular testing
Patients with non-specific back pain should have a normal lower extremity neurologic exam. Weakness, numbness or reflex changes are red flags for involvement of nerve root(s) or spinal cord.
Strength
You can assess lower extremity strength by testing each muscle group in isolation or with functional tests like squatting, standing, and heel and toe walking.
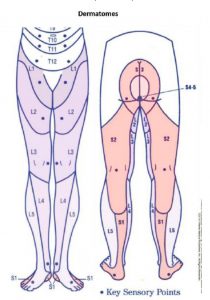
Sensation
To screen, test sensation at several points on each leg. If you are concerned about involvement of a specific nerve root, use the diagrams below to choose the key points at which to test sensation.
Reflexes
Test the patellar, Achilles, and plantar reflexes. Increased or decreased reflexes suggest different causes of back pain.
- Compression of nerve roots causes a lower motor neuron injury and decreased reflexes.
- Compression of the spinal cord causes an upper motor neuron injury and increased reflexes. Upper motor neuron injury also causes an upgoing toe on testing of plantar reflexes (positive Babinski).
Hypothesis Driven Physical Exam
If you are concerned about a lumbosacral radiculopathy
Lumbosacral radiculopathy is a common cause of back pain, usually radiating down one leg. It’s caused by impingement of a nerve root by a herniated intervertebral disc or an osteophyte. The most commonly involved nerve root is L5, followed by S1 and L4.
Findings specific to disc herniation at each level are:
| Pain | Numbness | Weakness | Decreased Reflex | |
| L4 | Back to medial thigh, medial ankle and foot | Medial calf and ankle | Quadriceps, tibialis anterior | Patellar |
| L5 | Back to back of leg, lateral calf, and classically, big toe | Dorsum of foot and big toe | Big toe extension, foot dorsiflexion, thigh abductors | No reflex associated with L5 |
| S1 | Back to back of leg, lateral ankle and sole | Lateral ankle and bottom of foot | Plantar flexion and thigh extension | Achilles |
To efficiently assess for findings of lumbar radiculopathy, test each of the following with the patient seated:
- Inversion of the foot/ankle
- Extension of the great toe
- Eversion of the foot/ankle
- Reflex at the patellar tendon
- Reflex at the Achilles tendon
- Sensation at key sensor points below
Straight leg raise (SLR)

With the patient supine, the examiner lifts the leg with the knee straight. If a bulging disc or osteophyte complex is present, this maneuver will stretch the L5 and S1 nerve roots over it, reproducing pain that radiates down the leg (not just to the back or hip).
- The SLR is positive if it reproduces pain in the lifted leg at < 70 degrees of hip flexion. This finding has a high sensitivity but a low specificity. If the SLR is negative, it argues strongly against lumbosacral radiculopathy.
- The crossed SLR is positive if pain is reproduced in the opposite leg. This test has a low sensitivity but a high specificity. If positive, it supports a diagnosis of lumbosacral radiculopathy.
Slump Test
The patient is seated on the table, leaning forward and with the head tucked (L and C spine flexion). The knee is then extended. Leg pain, numbness, or tingling is considered a positive test and supports a radiculopathy

Red flags in back pain
Signs and symptoms of cauda equina syndrome
- new urinary retention, fecal incontinence or saddle anesthesia
Significant neurologic deficits
- progressive motor weakness or significant motor deficits not localized to a single unilateral nerve root
Current or recent cancer
- especially if a history of or high risk for breast, prostate, lung, thyroid, kidney cancer or multiple myeloma
Signs or symptoms of spinal infection
- objective fever, current immunosuppression or hemodialysis, current or recent bacteremia, injection drug use, endocarditis, invasive epidural/spinal procedures
Risk for vertebral fractures
- history of trauma
- known history or high risk for osteoporosis