Immersion Cardiovascular Exam
Diseases of the cardiovascular system are common, and they can often be identified on physical exam. In Immersion, you’ll practice the basic technique and learn to recognize normal findings. During your circulatory systems block, after you’ve studied physiology and pathophysiology, you will learn more advanced maneuvers and abnormal findings. Use headphones or earbuds to listen to the heart sounds in this chapter.
After Immersion, you should be able to perform each of the following:
Inspection
- Inspect the anterior chest and neck for skin lesions as you perform the exam
- Inspect the precordium for abnormal movement
Palpation
- Palpate the carotid arteries, one at a time, observing strength & symmetry (may also be done with H&N exam)
- Palpate the apical impulse if you suspect valvular disease or cardiomyopathy
Auscultation
- Listen at each of the primary listening areas with the diaphragm or firm pressure on the adult side of the stethoscope:
- Right 2nd intercostal space (R upper sternal border)
- Left 2nd intercostal space (L upper sternal border)
- Left lower sternal border (along the sternum at the 5th intercostal space)
- Cardiac apex (midclavicular line in the 4th – 5th intercostal space)
- Listen with the bell or light pressure on the adult side of the stethoscope at the cardiac apex
- Listen for bruits over each carotid artery
Key Landmarks & Structures
Identify each of the following structures on yourself or on your physical exam partner.
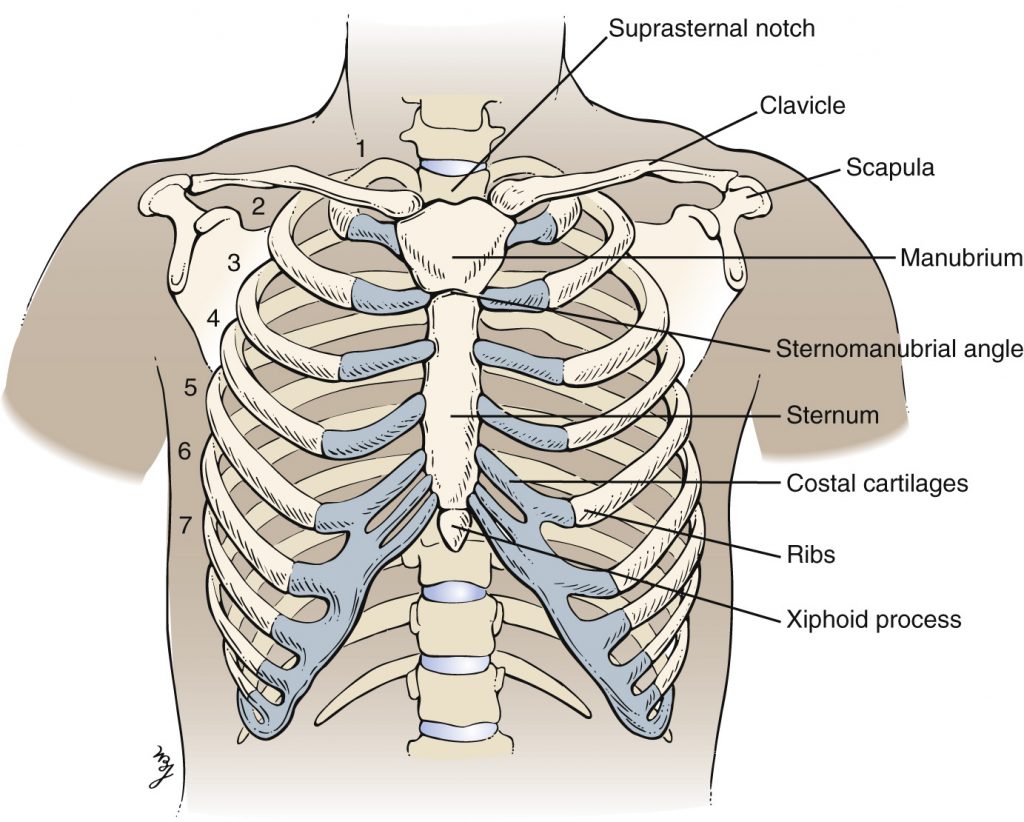
Suprasternal notch. Depression at the base of the neck, formed by the medial ends of the clavicles and top of the manubrium.
Sternomanubrial angle (a.k.a sternal angle) From the suprasternal notch, palpate down the sternum to find the place where the angle changes.
Midclavicular line (MCL). The line that runs through the midpoint of the clavicle towards the feet.
Four classic areas for auscultation:
- Right 2nd intercostal space. often referred to as R upper sternal border (RUSB). The space between ribs to the right of the sternomanubrial angle. Sounds from the aortic valve are often best heard here.
- Left 2nd intercostal space, often referred to as L upper sternal border (LUSB). The space between ribs to the left of the sternomanubrial angle.Sounds from the pulmonic valve are often best heard here.
- Left lower sternal border, in the area of the 5th left intercostal space. Palpate the 3rd, 4th and if possible the 5th left ICS. Sounds from the tricuspid valve are often best heard here.
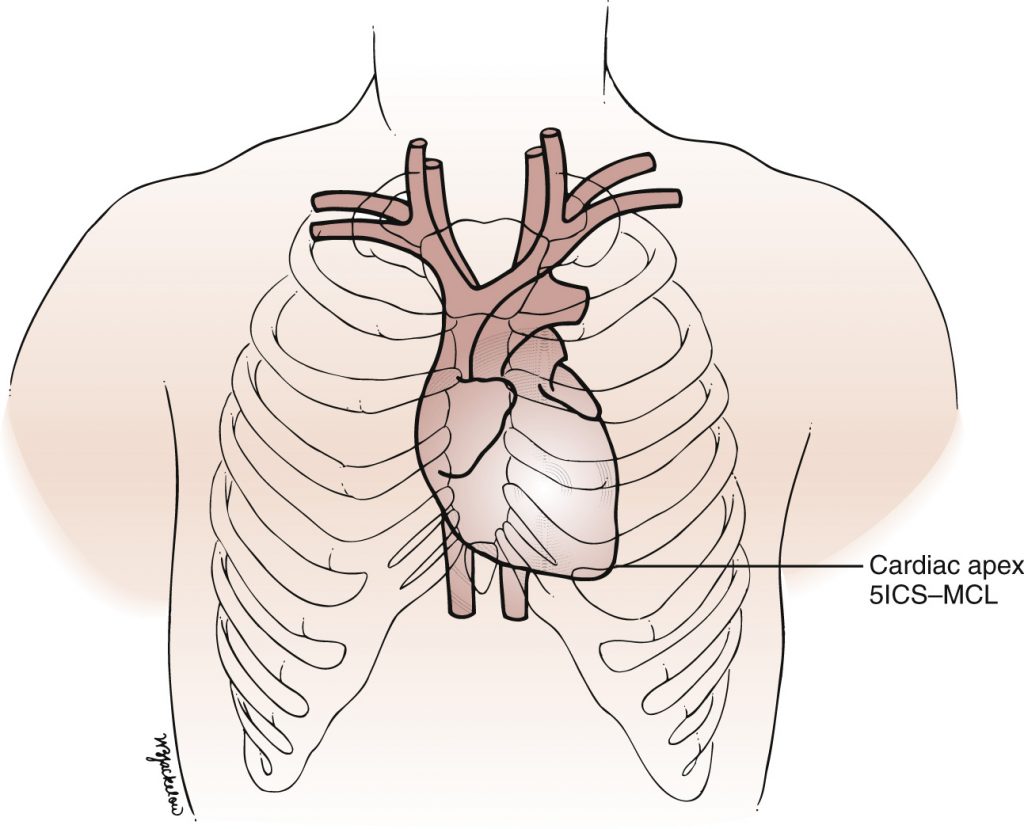
- Cardiac apex, the tapered tip of the left ventricle, which should lie at or medial to the MCL in the L 4th or 5th intercostal space. Sounds from the mitral valve and extra heart sounds are often best heard here, and on some people, the apical impulse can be palpated
Image from Chapter 13 of Textbook of Physical Diagnosis: History and Examination, Eighth Edition, Copyright © 2021. See link at the end of this chapter.
Image from Chapter 13 of Textbook of Physical Diagnosis: History and Examination, Eighth Edition, Copyright © 2021. See link at the end of this chapter.
Preparation & Positioning
Use appropriate draping to preserve patient comfort, adjusting as needed to maintain coverage. Avoid making assumptions that male patients are comfortable baring the torso. Ask permission or ask your patient to move their gown as needed, lowering from the neckline and/or raising from below to complete the exam appropriate for your individual patient. It is often easiest to inspect the precordium, palpate the apical impulse, and auscultate at apex with the gown raised from below. It can be lowered at the neckline to listen at the sternal borders.
For a complete cardiac exam in the hospital, start with your patient positioned at about a 30° angle, with the examiner ideally on the right. In the primary care clinic, many exams are performed with the patient sitting up on the exam table, which will detect abnormal cardiac rhythms like atrial fibrillation and some murmurs. The supine and partial left lateral decubitus position will allow you to better detect most abnormal sounds.
Inspection
Inspect the skin of the precordium as you perform the exam. Note any movement of the chest. In healthy people, the beating of the heart doesn’t usually cause any visible movement. In people with enlargement of one or more chambers of the heart, abnormal movement may be seen or more commonly felt.
Palpation
If you are concerned about valvular disease or cardiomyopathy, palpate the anterior chest for the apical impulse. In Immersion, if your PE partner is comfortable with this, you can also palpate it to identify the optimal location for auscultation.
Palpate to the L of the sternum, at the MCL in the 4th or 5th ICS. Palpate medially and then laterally if you are unable to find it initially. You may be able to palpate the apical impulse over breast tissue, or you may need to ask your patient to lift the breast to allow palpation.
The normal apical impulse is:
- palpable in < 50% of normal adults in the supine position
- less than the size of a quarter, or 2 cm in diameter
- at or medial to the mid-clavicular line in the 4th or 5th intercostal space
Healthy people with thin chests or high cardiac output states, like fever or pregnancy, can also have palpable movement just to the L of the lower sternum. Obvious or sustained movement in this area is caused by pressure overload of the right ventricle, which lies underneath and to the left of the sternum, or by an enlarged, overloaded left atrium.
Auscultation
Listen to the heart in a quiet room with a quiet patient. Listen at each of the four primary listening areas with the diaphragm of the stethoscope applied firmly to the chest. At each location, listen for normal heart sounds as well as extra heart sounds like murmurs or gallops. Then listen again at the cardiac apex with the bell or with the diaphragm of a tunable stethoscope applied lightly to the chest. If your patient has breasts, you may be able to hear heart sounds at the apex through breast tissue or you may need to ask them to lift the breast.
Use headphones to “auscultate” the normal heart sounds below. At each listening area, you should hear the “lub dub” of the normal cardiac cycle. Closure of the mitral and tricuspid valves, which connect the atria to the ventricles, creates the first of each pair of heart sounds, S1. Closure of the aortic and pulmonic valves, which connect the ventricles and the great arteries, creates the second heart sound, S2.
Systole is the period between S1 and S2, and diastole is the period between S2 and the following S1, when blood from the atria is filling the ventricles. Differentiating the two will become automatic with experience. For now, use the following clues to help you recognize systole and diastole:
- Systole is shorter than diastole at heart rates < 100
- S2 is almost always louder than S1 at the RUSB
- The beat of the carotid pulse happens during systole
Sample documentation: CV exam
Apical impulse is < 2 cm at L midclavicular line in the 5th intercostal space
Regular rate and rhythm. Normal S1 and S2, no S3, S4, or murmurs
Pulses 2+ and symmetric: carotid, radial, dorsalis pedis, and posterior tibialis***
No edema in the bilateral lower extremities***
*** Note: Palpation of carotid pulses may be performed in the head and neck exam. Palpation of dorsalis pedis and posterior tibialis pulses and for edema is usually performed with the lower extremity exam.
CV Exam Video
References & resources
left anterior chest
narrowing or leaking of one of the 4 heart valves
abnormal function of the heart muscle