Clinical Reasoning
Clinical reasoning is one of the core skills of a physician, used to diagnose the cause of new symptoms, to guide the choice of tests and treatment, to assess response to therapy, and to recognize patients’ strengths and address barriers to health.
Diagnostic reasoning can be thought of as a process that begins with the patient’s history and leads to a prioritized differential diagnosis, the list of most likely and most serious diagnoses that might explain a patient’s symptoms. This prioritized differential guides diagnostic testing, allowing the physician to focus testing on the illness that are most likely or most urgent. Establishing a diagnosis allows us to provide an explanation of a patient’s health problem and to predict its course.
Diagnostic reasoning begins with gathering information. As an experienced clinician takes a history, the patient’s story activates illness scripts in their memory. An illness script is an organized mental summary of that clinician’s understanding of an illness, based on both their clinical experience and theoretical knowledge. An illness script may be activated almost automatically by pattern recognition, or it may require conscious effort and analysis. Illnesses whose scripts match the patient’s clinical picture are added to the differential diagnosis. By the time an experienced clinician has finished an HPI, they usually have a differential in mind.
Dual process theory
Humans use two cognitive systems make sense of the world around them. System 1 is based on pattern recognition – intuitive, efficient, and so quick that the process of reasoning is subconscious. System 2 is slow and deliberate, consciously and explicitly analyzing information to arrive at a conclusion. Physicians rely on both systems to make their diagnoses.
When a patient’s problem is familiar, system 1 uses pattern recognition to suggest a diagnosis quickly and efficiently. To avoid errors, this first impression can be double checked to make sure everything fits and to exclude more dangerous causes. When a problem is less familiar, system 2 must consciously and deliberately analyze the history to arrive at a differential.
System 1 and system 2 each have advantages and disadvantages. System 1 is quick, requires less cognitive effort, and is generally accurate for familiar problems. System 2 is slower and requires more cognitive energy but can reason through a problem in the face of complexity and uncertainty. Experienced doctors fall back on system 2 when seeing a less familiar problem or one that is more complex or potentially high stakes.
The majority of your reasoning will be System 2 until you gain more knowledge and expertise.
Testing diagnostic hypotheses
Diagnostic possibilities can be tested with focused questions, physical exam, and diagnostic tests. The clinician actively looks for findings that support or argue against the illnesses on their differential. A prioritized differential diagnosis – the most likely or most lethal causes of a patient’s problem, ranked by likelihood – then guides decisions about further testing and treatment.
Practicing clinical reasoning
Clinical reasoning is dependent on medical knowledge. You will build your diagnostic skill through practice with cases – written cases, small group cases, and simulated and real life patients.
FCM simulation workshops are a structured and fun chance to practice clinical reasoning. In each sim, you’ll see several different patients with a chief concern relevant to your block. You’ll practice each step in the process as you manage a simulated patient, get feedback on how you’ve done, and build your approach to these common symptoms.
Medical students tend to use more system 2 thinking, since they have too little knowledge and experience to rely on system 1. You may intuitively come up with diagnostic hypotheses for some of your patients’ problems, like ‘heart attack’ for chest pain or ‘meningitis’ for fever and headache. But as first year students, we expect most of your reasoning to be system 2 – analytic and slow – and it will often happen after you are done with your H&P. Reasoning in real time will become easier as you learn more about medicine, see more patients, and develop your own mental frameworks for common problems.
Learning from patients is another important way to build your reasoning skills, every time you are in the hospital or clinic. If the patient’s diagnosis is known, you’ll begin to recognize the pattern of that illness. You can also build and practice using diagnostic schema, a cognitive tool to help you systematically approach a clinical problem by providing an organizing scaffold. Building these scaffolds for one patient will give you an approach that you can then use with future patients who have the same chief concern.
Diagnostic schema for many problems can be found in:
- The Patient History: An Evidence Based Approach to Differential Diagnosis. A basic overview, great for first years.
- Clinical Problem Solvers, a site devoted to diagnostic reasoning with many contributions from senior medical students. Easier to understand after you’ve finished the relevant block!
Written patient cases and small groups in the block will also help you grow the medical knowledge needed to be a good diagnostician. For more practice, check out the New England Journal of Medicine’s Clinical Problem-Solving series.
A Universal Model of Diagnostic Reasoning : Academic Medicine (lww.com)
Sim 1. Problem representation
Gathering information is the first step in diagnostic reasoning – an accurate history is the key to the correct diagnosis. A 1975 study queried doctors about their leading diagnosis after the history, after the exam and after labs. These were compared to the ultimate, correct diagnosis. Eighty-two percent of the time, physicians arrived at the correct diagnosis after the history alone. The exam led to the diagnosis 9% of the time, and labs and imaging to the other 9%.
This study was repeated in the 1990’s, when diagnostic tests were much more readily available, with similar findings. In four out of five patients, expert clinicians arrived at the diagnosis after the history alone. The physical exam and diagnostic testing are used for confirmation, but a detailed and accurate history is still the cornerstone of diagnostic reasoning.
The correct diagnosis is suggested by the history in four out of every five patients with a new concern.
The problem representation
As a patient tells their story, the most important pieces of data are synthesized into a problem representation in the clinician’s mind. This problem representation activates illness scripts for ‘matching’ diseases that could be causing the patient’s symptoms.
Once a potential ‘match’ is identified, the physician checks it by gathering more information, comparing the patient’s symptoms and signs to what they know about that disease. Key information is added to the problem representation over the course of the H&P, with each iteration (ideally) bringing us closer to a correct diagnosis.
Your problem representations should be 1-2 sentences long and should include this diagnostically useful information.
- Patient demographics and predisposing conditions.
- Time course of illness.
- Clinical syndrome.
Demographics and predisposing conditions
The age of your patient is critically important in diagnostic reasoning – common causes of a given problem differ dramatically across the life span.
For some problems, sex is also important. Lower abdominal pain in a female patient could be caused by ovarian pathology or ectopic pregnancy on top of the appendicitis, diverticulitis and bladder infection that affect both females and males.
Predisposing conditions are medical problems or social conditions that are related to diagnoses that cause your patient’s concern. For example, high blood pressure is a predisposing condition for a patient presenting with chest pain since it’s a major risk factor for heart disease. Recent incarceration is a predisposing condition for someone presenting with fever, as tuberculosis transmission is more common in that setting. A history of recurrent UTIs is a predisposing condition for someone with lower abdominal pain – if it’s happened once it’s more likely to happen again.
You will become more confident in identifying predisposing conditions as you learn about different diseases in your Foundations blocks. For now, you can include major ongoing illnesses in your problem representation.
Timing of illness
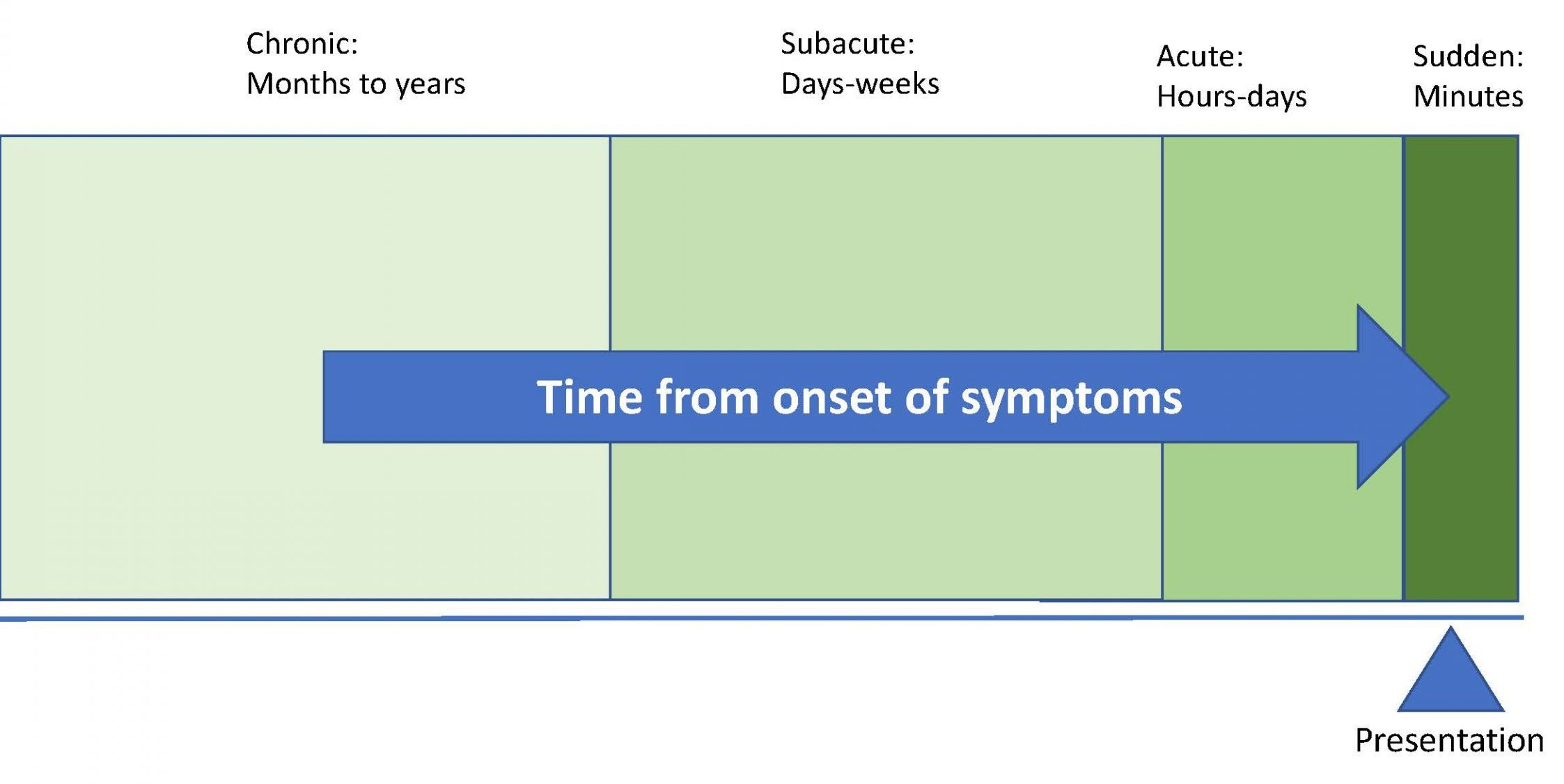
Different diseases have different patterns of onset and progression, so a precise description of onset and time course can narrow your differential diagnosis. The onset of a patient’s symptoms can be described as hyperacute or sudden (minutes), acute (hours to days), subacute (days to weeks) or chronic.
The pattern of symptoms can also be diagnostically useful. It can be described as intermittent or constant; stable, progressive, or improving; relapsing or recurrent, waxing and waning.
Clinical syndrome
The word syndrome is derived from the Greek words meaning “running together.” In medicine, it refers to a collection of symptoms & signs, often with a specific medical term, like “monoarticular arthritis.” You’ll learn about many syndromes over the course of Foundations.
For now, start with your patient’s chief concern and add any other symptoms that came on around the same time and seem important to you.
You should also add appropriate semantic qualifiers to describe the chief concern. Semantic qualifiers are pairs of words that divide causes of a problem into different categories, each due to a different set of illnesses. By limiting the location, severity, and time course of a problem, they make the problem representation more precise, narrow the differential diagnosis, and reduce cognitive load.
Some semantic qualifiers are specific to a single chief concern. For example, chest pain may be pleuritic (worse with a deep breath) or non-pleuritic. A cough may be productive or non-productive of sputum. These two categories of each symptom have a very different differential diagnosis.
Semantic qualifiers that may used across many concerns include:
- Left or right
- Anterior or posterior
- Superficial or deep
- Proximal or distal
- Mild or severe
- Improving or worsening
- Sharp or dull
- Radiating or non-radiating
- Exertional or non-exertional
Placing the problem in context
Siting the current problem in the context of your patient’s overall health can also improve your differential. Your patient’s problem list provides that big picture: Chronic illnesses, health behaviors and risks, acute problems that could recur, and social factors that impact health are all documented on the problem list, often in a specific area of the EHR
To prepare for the back pain simulation
Read Chapter 54, Low Back Pain from The Patient History: An Evidence Based Approach to Differential Diagnosis. Pay careful attention to the diagnostic schema that is presented and to the semantic qualifiers that are important in characterizing back pain. These will support your clinical reasoning as you assess your simulated patients!
Resources and references:
Problem representation overview. Journal of General Internal Medicine. Includes case examples that will make more sense after a few more blocks.
Sim 2. Illness scripts
An illness script is an organized mental summary of your knowledge of a disease. It can be called up from memory almost instantaneously when you recognize a familiar pattern of signs and symptoms. Or it may take deliberate thought to find a script that matches a less familiar problem. When an illness script seems reasonably close to your patient’s presentation, that diagnosis is added to your differential.
Illness scripts are unique to individual clinicians, and most are built without conscious thought. You are already creating illness scripts for every disease you learn about, and you’ll add to it each time you diagnose a patient with that disease for the rest of your career.
Consciously comparing illness scripts can build your diagnostic skills more quickly. In this workshop, we’ll call on illness scripts for diagnoses that present with sore throat, using what you’ve learned in Infections & Immunity to practice thinking like a doctor!
Components of an illness script
The cognitive psychologists who first studied illness scripts identified three categories of information that most clinicians include:
- Fault: the pathophysiology that led to the illness.
- Predisposing conditions: the medical issues or social factors that promote or contribute to the disease
- Consequences: the typical signs and symptoms
Most clinicians also include management in their illness scripts. In FCM, we will focus on predisposing conditions and consequences, which we identify with the history and physical.
Problem representation to illness scripts
During the interview, an experienced physician compares their developing problem representation against illness scripts activated in their memories. Those that seem to ‘match’ become part of the differential diagnosis.
Imagine that you’re in your primary care clinic, about to see a previously healthy 15-year-old. The reason for the visit is listed as “2 days of sore throat and fever”. Your problem representation as you walk in the room is “healthy teenager with sore throat and fever”
Based on this limited information, diagnoses are probably already coming to mind. Strep throat is so common that pattern recognition may have activated this illness script right away.
| Diagnosis | Classical History | Epidemiology & pre | Classic exam findings |
|---|---|---|---|
| Strep throat | Sudden onset
Fever No cough nor rhinorrhea |
15% of adult cases
30% of pediatric cases Most common in 4-15 year-olds Uncommon > 45 unless exposed to kids |
T > 38
Tonsillar exudate Tender anterior cervical adenopathy May have palatal petechiae |
A pediatrician’s illness script for GAS pharyngitis would have much more detail, based on the hundreds of patients that they’ve seen. It would expand beyond the ‘classic’ findings to include less common presentations. Your illness scripts will be richer and more detailed for diseases that you see often.
In your blocks, you usually learn about diseases one at a time, but most patients present with a chief concern that suggests several possible diagnoses. Thinking about these diagnoses in parallel can help you develop your diagnostic reasoning skills. Next term, your FCM write-ups will include the illness scripts for 3 or 4 ‘most likely’ and ‘most lethal’ diagnoses on your differential in a table called a diagnoses matrix.
This matrix allows you to explicitly COMPARE and CONTRAST the different potential causes of your patient’s problem, identifying the history, risk factors and exam findings that might help you differentiate between them. We’ll practice using it in the sim!
| “Classic” History | Epidemiology & risk factors | Classic exam findings | |
|---|---|---|---|
| GABHS | Sudden onset
Fever No cough or rhinorrhea |
15% of adult cases
30% of pediatric cases Most common in 4-15 y.o. Uncommon in > 45 y.o. unless exposure to kids |
T > 38
Tonsillar exudate Tender anterior cervical adenopathy. May have palatal petechiae |
| Viral URI | Associated cold symptoms: nasal congestion, coryza, hoarseness, sinus discomfort, ear pain, or cough | 50% of adult cases | May have nasal congestion, conjunctivitis
Exam findings are typically minimal despite the patient feeling poorly. |
| Mono/EBV | Starts with malaise, headache, fever.
Significant fatigue Sore throat is the most prominent symptom. Other viruses can cause a mono-like syndrome, including acute HIV infection. |
Peak incidence is in the 15 to 24- year old range.
<2% of adult pharyngitis Mono-like syndrome can be caused by other viruses, such as acute HIV infection |
Tender cervical adenopathy.
May have splenomegaly and diffuse lymphadenopathy (peaks in the first week) May have palatal petechiae |
Resources & references
Sim 3. Testing diagnostic hypotheses
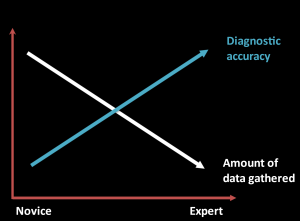
Although expert clinicians gather much less data than novices, their diagnoses are more likely to be accurate. Experts’ knowledge and experience allow them to target questions, exam maneuvers, and testing to the problem at hand. As a novice, you rely on the comprehensive H&P to uncover important details – experts gather less data but their experience allows them to target better data.
To confirm their diagnostic hypotheses, clinicians can test them with questions about specific symptoms or risk factors for the diseases they’re considering. They may look for an exam finding or perform labs or x-rays. The results of each of these investigations – focused questions, hypothesis-driven physical exam, and diagnostic testing – can support or argue against diseases that are on the differential. Comparing illness scripts can help you identify the signs and symptoms that are most useful in differentiating between diagnoses.
Compare the three causes of acute pharyngitis below. Some features, like acute onset and fever, are common to all three, but there are also important differences. Most patients with a viral URI have cough or rhinorrhea while those with streptococcal pharyngitis do not. Exposure to children makes streptococcal pharyngitis more likely in adults. And cervical lymphadenopathy is common in strep pharyngitis and mono but uncommon in routine viral URI.
| Sore throat & fever | History | Epidemiology & risk factors | Physical exam |
| GAS pharyngitis | Acute onset
Sore throat Fever No cough or rhinorrhea |
Common cause of pharyngitis:
Most common in 3-14 y.o. In adults: Exposure to kids |
Pharyngeal erythema
Tonsillar exudate Tender cervical adenopathy May have palatal petechiae |
| Mono (EBV) | Acute: sore throat is the most prominent
Malaise, headache, fever, anorexia Significant fatigue |
Peak incidence: 15 to 24
<2% of adult pharyngitis |
Tender cervical adenopathy
May have:
|
| Viral URI | Acute onset
Usually cough or rhinorrhea Fever less common |
Common cause in kids and adults | Pharyngeal erythema
Nasal discharge No adenopathy |
A novice would learn about the absence of cough, exposure to children and the presence of cervical adenopathy during a complete H&P. Experts, on the other hand, would target their focused questions to uncover these differences, which are diagnostically useful in sore throat. Symptoms or risk factors that change the likelihood of a diagnosis (like cough or rhinorrhea) would be added to your problem representation.
Sometimes, a specific symptom or risk factor is required to make a diagnosis. For example, if a patient with fever has never travelled outside the Northwest, they cannot have malaria. Focused question can also target red flags that require additional investigation, like severe pain with jaw opening in a patient with sore throat. An expert who elicited that red flag would examine and test for an abscess.
Diagnostic utility of clinical findings
Symptoms and physical exam signs can be considered ‘diagnostic tests’, just like a lab test or x-rays. Their validity (or accuracy) refers to their ability to distinguish between people who have and those who do not have a disease. Just as with lab testing, not all positive results are true positives. Some patients with crushing substernal chest pain have a diagnosis other than acute coronary syndrome. A yes or no answer to a focused question usually doesn’t ‘rule in’ or ‘rule out’ a disease, it just changes the probability.
As you learn about the ‘classic’ symptoms of diseases, consider how much each changes the probability of the diagnosis. For some diseases, the sensitivity and specificity of different signs and symptoms have been studied. The JAMA Rational Clinical Exam series and “The Patient History: An Evidence-Based Approach to Differential Diagnosis” summarize the available data on the accuracy symptoms and risk factor in predicting specific diagnoses. As your clinical experience grows, you’ll get a sense of how much certain symptoms change the probability in the patient population that you see.
Likelihood ratios
The utility of a clinical feature can be reported as a likelihood ratio (LR), a number calculated from the finding’s sensitivity and specificity. Likelihood ratios can range from 0 to ∞.
Findings with LRs greater than 1 increase the probability of disease – the higher the LR, the more strongly the feature supports the disease.
Findings with LRs less than 1 decrease the probability of disease – the closer the LR is to zero, the more strongly it argues against the disease. Findings with an LR right around 1 aren’t useful – they don’t meaningfully change the probability of disease.
Here’s an example, from a JAMA Rational Clinical Exam article on lumbar spinal stenosis, a common cause of back pain in older adults.
| LR+ (95% CI) | LR- (95% CI) | |
| Symptoms | ||
| Absence of pain when seated | 7.4 (1.9-30) | 0.57 (0.43-0.76) |
| Improvement of symptoms when bending forward | 6.4 (4.1-9.9) | 0.52 (0.46-0.60) |
| Bilateral buttock or leg pain | 6.3 (3.1-13) | 0.54 (0.43-0.68) |
| Neurologic claudication | 3.7 (2.9-4.8) | 0.23 (0.17-0.31) |
| Signs | ||
| Wide based gait | 13 (1.9-95) | 0.60 (0.46-0.78) |
| Romberg test | 4.2 (1.4-13) | 0.67 (0.51-0.87) |
The authors identified three symptoms that strongly support spinal stenosis if present, with a positive LRs > 5: absence of pain when seated, improvement in symptoms when bending forward, and bilateral buttock or leg pain. A ‘no’ to any of these questions argues only weakly against spinal stenosis because the negative likelihood ratios are ~ 0.5.
Neurogenic claudication – leg pain that develops with standing or walking – supports a diagnosis of spinal stenosis less strongly. The positive LR for this question is lower. But with a negative LR of 0.2, the absence of neurogenic claudication argues more strongly against spinal stenosis.
Knowing this, you can ask each of these focused questions when seeing patients with chronic back pain.
Testing hypotheses with physical exam
A century ago, the gold standard for most diagnoses was, out of necessity, the physical exam. But even with today’s technology, the physical exam is still essential.
Some diagnoses, such as cellulitis, are still made based on physical exam findings – there is no diagnostic test that performs better. Sometimes the exam suggests a possibility that you hadn’t considered – unilateral throat swelling suggests peritonsillar abscess in a patient that you thought had plain old strep throat.
Having diagnostic hypotheses as you start your physical can focus your attention on the most helpful findings. You are much more likely to notice a soft heart murmur if you’re thinking about pulmonary hypertension than if you are just going through a ‘complete’ PE. Your diagnostic hypothesis can also add specific maneuvers to your exam, those with findings that change the probability of the diagnoses on your differential.
Physical exam findings can move the probability of a diagnosis up or down. That might be enough to forego a lab or imaging study because the likelihood of a diagnosis is now so low – or to justify expensive testing because the likelihood is now higher. In this workshop, we’ll discuss some exam findings that are helpful in patients with chest pain, and we’ll return to the hypothesis driven exam in future sims.
Evidence-Based Physical Diagnosis, available full text through the Health Sciences Library, is an excellent summary of the evidence supporting physical exam. For some exam maneuvers, there isn’t any evidence – it has not been formally studied. Sometimes the evidence is just what you’d expect, and sometimes the evidence is surprising.
Resources & references
The Patient History: An Evidence Based Approach to Differential Diagnosis. Henderson, Mark et al. Lange, 2012. LINK
Evidence Based Physical Diagnosis, 5th ed. McGee, Steven R. Elsevier, 2022. LINK
JAMA Rational Clinical Exam Series LINK
Sim 4. Team communication
TeamSTEPPS is an evidence-based set of strategies intended to improve team performance. In this video, Tonya Martino, the Director of Team Performance for the WWAMI Institute for Simulation in Healthcare, introduces TeamSTEPPS and discusses the communication strategies we will practice in this week’s simulation: closed loop communication and SBAR.
SBAR
SBAR is a way to communicate key information efficiently.
Resources & references
A Cognitive Autopsy Approach Towards Explaining Diagnostic Failure – PMC (nih.gov)
Sim 5. Prioritize the differential
Intro (1). Today we’ll talk about prioritizing a differential diagnosis. After defining the problem, you’ve come up with diagnostic hypotheses, and tested them using focused questions and the physical exam. How do you decide which diagnosis is most likely?
Recap of pattern recognition versus analytic thinking (2). Remember there are two ways doctors can arrive at a working diagnosis. The first is pattern recognition. The doctor using system 1 thinking intuitively and rapidly recognizes the problem. A few focused questions and the exam confirm the diagnosis and maybe exclude dangerous alternatives, and that’s that.
The second approach is analytic. The doctor using system 2 consciously and explicitly analyzes information, attempting to match the patient’s problem to the illness scripts she’s built over the years.
Expert clinicians seeing a patient with a familiar problem often use pattern recognition. Even experts fall back on analytic thinking when a patient has an uncommon, atypical, or high risk presentation. We don’t want to rely on our gut instincts alone if the problem’s tough or the consequences of a mistake are bad.
As a novice diagnostician, you should practice using system 2, analytic thinking for any patient with a new concern – at least until you’re a resident, you’re really not allowed to NOT have a differential diagnosis for a patient’s problem. As your clinical experience grows, you’ll find yourself using more pattern recognition.
Differential diagnosis (3). Your goal: a differential diagnosis that includes the most likely and in some cases, the most lethal, causes of your patient’s problem. Our brains can handle only so much cognitive load – we can’t realistically consider more than 5 or 6 diagnoses at once. So how do we figure out which should be on our differential?
A good place to start is with the pretest probability – the relative likelihood of different diagnoses in patients presenting with the same problem. You may have heard the old saying “When you hear hoofbeats, think horses not zebras” (at least in the United States). In general, a common illness is much more likely than a rare one, though the rare ones are sometimes the ones that come to mind.
As you learn about illnesses, pay attention to whether they’re common or rare. Look up the frequency of different causes of your patients’ chief concerns. Over time, you’ll develop a sense of how common each is in your patient population.
An example (4). Let’s say you’re seeing a 42 year old man with difficult to control hypertension. He is on maximum doses of 3 medications – a diuretic, a beta blocker, and an ACE inhibitor. Despite the excellent regimen, his BP in the office is still consistently in the 160-170’s/90s. Take a minute and come up with your differential diagnosis as you walk in the door to see him.
I bet you came up with diagnoses like these. (pheochromocytoma (< 1%), hyperaldosteronism (~10%), Cushings’s (<1%), coarctation of the aorta(<1%)
It turns out that these are all rare causes of resistant hypertension. By far the most common is poor medication adherence. The exact prevalence is hard to pin down, but in one study that used chromatography to measure drug levels, almost 50% of patients with resistant hypertension seemed to have a significant problem with adherence. Sleep apnea, excess salt intake, and kidney disease are also more common than the ‘zebras’ that jump quickly to mind.
Hypothesis testing (5). So walking in the door, maybe your differential diagnosis looked like this.
You test your hypotheses with focused questions. Each answer has the potential to change your differential: to move the probability of a diagnosis up or down, or sometimes, eliminate it completely.
You start with questions about adherence. You remember a Rational clinical exam article – a ‘yes’ answer to one question – have you missed any pills in the last week – supports nonadherence if the answer is yes, and argues against it if the answer is no. (+ LR of 4.3, – LR of 0.5). Your patient is vague about medication names and doses, and says he has missed doses this week. Now nonadherence is even more likely.
You might ask more focused questions about the other items on your differential, to make sure there’s not another diagnosis you SHOULD be considering now.
You perform an exam, again testing your hypotheses. You might check weight and neck circumference to assess sleep apnea risk, or check for striae or hirsutism that might indicate Cushing’s. Assuming you don’t find anything that supports these, you’re left with medication nonadherence and renal disease at the top of your differential. You can check a creatinine and focus on adherence rather than spend many thousands of dollars testing for a whole list of very unlikely possibilities. You might hear this referred to as ‘shotgun’ testing. Hoping to hit the target, but not knowing quite what it is, you aims in a lot of directions at once. The expert shoots right at the target.
Flip the script (6). What if your patient with difficult to control hypertension said yes, he does have intermittent pounding headaches, the most common feature of symptomatic pheos after hypertension. And yes, he does have palpitations associated with his headaches. These ‘yeses’ move the probability of pheochromocytoma up enough to test for it, which is expensive, inconvenient, and often falsely positive. Given the low prevalence of pheo, other diagnoses are still more likely even with headaches and palpitations, but your focused questions have moved you above the testing threshold – it’s a diagnosis you wouldn’t want to miss.
Changing probability (7): As you gather information from the history and exam, the probability of the diagnoses on your differential changes. The more features of your patient’s illness match the typical presentation of the disease, the more likely it is. If your patient with resistant hypertension, headaches, and palpitations also has episodic pallor and diaphoresis, a family history of pheo, and orthostatic hypotension, you really need to get cracking on working it up.
The more common features your patient lacks, the less likely it is. Sometimes, the lack of a single clinical finding will actually rule out a diagnosis – it’s a must have feature. For example, if your patient with fever of unknown origin reports that she’s never left the state of Washington, you can pretty much rule out malaria as a cause. But remember, usually the presence or absence of a features just changes probability rather than ruling a diagnosis in or out.
getting better and worse but never going away
