Term 1 Sample Write Up
CC/ID:
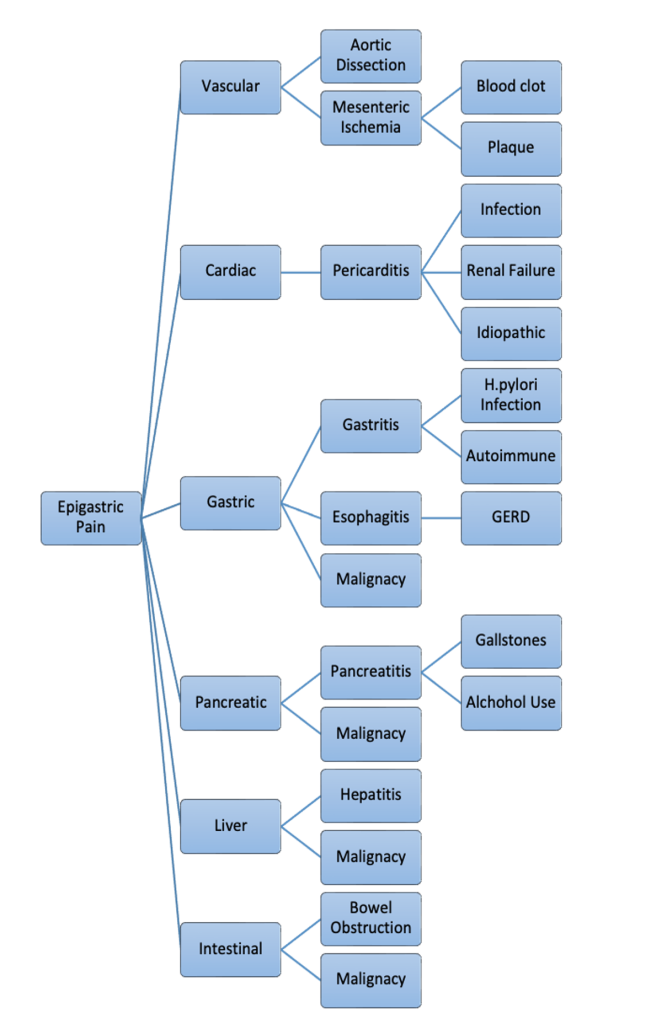
SP is a 60-year-old woman with a history of pancreatitis and pancreatic cysts who presented with acute, stabbing epigastric pain, vomiting, and diarrhea.
HPI:
SP was in her usual state of health until yesterday around 5PM when she sat down for dinner. Just prior to eating, she described that she started to feel “unwell” with “flu-like” symptoms that quickly developed into more severe nausea, vomiting, and diarrhea accompanied with the stabbing epigastric pain that she rated at a 10/10. SP further explained that the epigastric pain felt as though it was moving toward her back and would become more severe when she took a breath. There were no alleviating factors to help with the pain. SP’s husband quickly brought her into the ER, where she was diagnosed with pancreatitis.
This episode of epigastric pain, vomiting and diarrhea was very similar to an incident 4-5 years ago. During this first episode, SP experienced the same progression of symptoms with nausea, vomiting, diarrhea, and stabbing epigastric pain, but she rated the pain less severe at an 8/10. With this first occurrence, she also went to the ER where she received oral pain medications and found cysts on her pancreas, which were biopsied and found to be benign.
Since this time, she has had regular 6-month checkups to assess the status of the cysts. They have not changed in size over the last 4-5 years, so she will now receive yearly imaging. The status of the cysts has also remained the same through this current pancreatitis episode. SP denies any other attributing factors that preceded either episode of pancreatitis.
No known history of gallstones. She drinks 1-2 glasses of wine every night. One regular bottle of wine lasts 3-4 nights. Her alcohol consumption was significantly higher prior to the patient turning 30
Hospital course
SP is currently on IV pain medication, which is controlling the pain. She tried eating ice cream on 10/11, which she threw up and has not had anything else to eat while in the hospital. She has been drinking water.
Past Medical History:
Major Childhood Illnesses:
Patient denies any childhood illnesses
Medical Problems:
- Pancreatic cysts, diagnosed about 4-5 years ago
- Biopsy was benign
- Patient has regular imaging to check the status
- Pancreatitis, diagnosed around 4-5 years ago
- Controlled with pain medication and currently hospitalized with first recurrence
Surgeries/Trauma:
- Hysterectomy- 2012 (should clarify why hysterectomy occurred)
- Uterine Suspension- 1982
Psychiatric History:
- History of anxiety
- Controlled with escitalopram (lexapro) taken as needed.
Medications:
- Thyroid medication: unknown dosage
- Estrogen: unknown dosage
- Omeprazole (Prilosec): unknown dosage taken as needed for gas
- Vitamins
- Escitalopram (Lexapro): 0.5 mg taken as needed (should confirm if takes as needed on daily bases or as needed for a temporarily daily dose just during episodes of worse anxiety)
Allergies: I forgot to ask what her reactions were to the medications
- Sulfa
- Hydrocodone
Health Related Behaviors:
- Tobacco: Started smoking at 18 years old, around 5-6 cigarettes per day.
- Quit smoking 7 years ago
- Alcohol: 1-2 glasses of wine every night
- One regular bottle of wine lasts 3-4 nights
- Alcohol consumption was significantly higher prior to the patient turning 30
- Recreational Drugs: None
- IV Drug Use: None
- Diet: no specific diets
- Exercise: No regular exercise program
- Tries to go for walks but does not enjoy exercising
FHx:
- Father: heart arrhythmia, heart stents, type II diabetes, asthma
- Mom: high cholesterol
- Brother: asthma
- Grandparents: unknown
SH:
SP lives in a house in X with her husband of 4 years. SP is currently working as a business manager for a dental clinic and has been in this position for the last X years. She is planning on retiring this summer. Her husband is retired and does a lot of housework. She has one stepdaughter and three step-grandsons. They live in X, and SP and her husband watch the youngest grandson weekly. SP enjoys fishing, gardening, camping, crocheting, watching football and hanging out with her youngest grandson. SP and her husband are financially stable and do not have any major concerns.
ROS:
General: see HPI
Derm: No rashes, lumps, or lesions to note. No yellowing of the skin
HEENT:
- Eyes: no diplopia, no change in vision. No yellowing of the eyes
- Ears: no difficulty hearing, tinnitus, or vertigo
- Nose: no nose bleeds, sinusitis, or rhinorrhea
- Mouth: no sores, gingival bleeding or other dental changes
Respiratory: no SOB, cough, wheezing or cyanosis
Cardiovascular: no chest pain, palpitations, or edema
Gastrointestinal: See HPI
Genitourinary: no dysuria, change in frequency of urination, hematuria, urinary incontinence, or vaginal discharge
Endocrine: no polyuria or polydipsia
Musculoskeletal: no joint pain, or myalgias
Hematologic: no unusual bruising or lymphadenopathy
Neurological: no headache, speech problems, seizures, numbness, ataxia, or falls
Psychiatric: no insomnia or changes in frequency of anxiety
PE
General: SP looks comfortable and well, responds to questions without difficulty, experiences some discomfort with movements, but no signs of acute distress.
Vital Signs: BP 145/86; Pulse 88; Resp 14
Skin: Warm, dry, no rashes. No jaundice
HEENT:
- Eyes: no scleral icterus and palpebral conjunctiva are well-perfused (not pale)
- Nose: external nose without lesions or asymmetry
- Mouth/Throat: Mucosa is pink without lesions. The floor of the mouth is dry with very little salivary pooling.
NeckThyroid:
- No visible lesions or asymmetry
- Did not palpate for thyroid
Chest/Lungs:
- Quiet breath sounds bilaterally likely due to pain experienced when taking deep breaths.
- No visible lesions or abnormalities on chest
Cardiovascular:
- Regular rate and rhythm. No murmurs or rubs or gallops heard with auscultation
Abdomen:
- Non distended abdomen. Bowel sounds present but infrequent and soft. Tenderness to light palpation of the epigastric area without guarding. No tenderness to light palpitations in other quadrants. LIver is 7cm on percussion. No masses. No splenomegaly
Musculoskeletal:
- MSK exam was not performed
Gentital: Omitted
Rectal: Omitted
Neurologic:
- Not performed
Summary
SP is a 60-year-old woman who presented to the ER with acute epigastric pain, vomiting and diarrhea. This was the second presentation of these symptoms which were both attributed to pancreatitis. No attributing factors were mentioned; however, the alcohol use history may be of note with SP reporting she drinks at least 1 glass of wine each night with more alcohol being consumed regularly before her 30s and liver. Her physical exam was remarkable for epigastric tenderness.