Substance use history
At preventive health visits, a substance use history can identify opportunities for education and harm reduction to maintain health. At a hospital admission or problem focused visit, a patient’s substance use history could make a diagnosis on your differential more or less likely. For example, heavy alcohol use is a common cause of acute jaundice or cocaine could be the cause of chest pain.
You’ll learn about behavior change counseling in FCM next term and about the diagnostic evaluation and treatment of substance use disorders in the Mind, Brain and Behavior Block next fall. This chapter provides a brief introduction to the prevalence and impact of tobacco, alcohol and other substances as well as an approach to initial screening questions and quantifying use for those with positive screens.
Setting the stage:
Although substance use is often thought of as an individual’s ‘choice’, addiction is strongly influenced by genetics and by adverse childhood experiences, and experts now treat it as a chronic disease.
Despite this, substance use disorder is highly stigmatized in our society. To elicit an effective history, clinicians must inquire about substance use in a compassionate and nonjudgmental way and maintain awareness of their own biases. Otherwise, they risk perpetuating stigma, alienating patients, and missing opportunities for harm reduction and better health.
In general, you’ll elicit less sensitive parts of the history first, and then after building rapport, explicitly transition to this new set of questions. Your transition should:
- make the substance use history routine
- explain the relevance to care
- and ask permission to proceed
If your patient has concerns about confidentiality, there are additional federal protections (beyond HIPAA) for information about sensitive conditions, including drug and alcohol use disorders (42 CFR Part 2).
Screening questions
Screening questions identify patients for whom a more detailed history is needed. This information might be gathered on a paper or electronic intake form completed by the patient, or the provider may ask the questions below. We’d like you to practice the history in hospital visits, with your patient’s permission, to build confidence in this important skill.
Prevalence & impact of screening
Tobacco
Prevalence & outcomes: Fourteen percent of American adults smoke and smoking is responsible for one in five deaths. There is no safe level of cigarette use – as little as one per day increases the risk of heart attack and stroke.
Teens are more likely to vape nicotine daily than smoke. Although vaping avoids exposure to many of the toxins in smoke, it can’t be considered safe. Teens who vape nicotine are exponentially more likely to become cigarette smokers, chemicals and other toxins are still inhaled, and the long-term impact is still unknown.
Impact of screening: Although most smokers say they want to quit, only 6% per year are able to do so on their own. Advice from a provider doubles the chance of quitting, and a combination of pharmacotherapy and counseling can increase the success rate to 30%. Smoking cessation is beneficial for everyone, even for those over 65 and those who have already developed lung cancer. After quitting, excess mortality begins to fall within one year and approaches baseline after 10-15 years. An acute hospitalization, especially one for a smoking related illness, is an ideal opportunity to encourage smoking cessation.
Screening question: In the clinic, an intake form or a medical assistant may already have gathered this information. In other settings, you can ask “Do you sometimes smoke or use other tobacco products?”
Consider an additional question about vaping for teens, who may not consider vaping a ‘tobacco product’.
Next steps for a positive screen: Quantify current and prior cigarette use and report it in pack years (years smoked x packs per day). Total tobacco use impacts the risk of smoking related illnesses, and current use can guide the amount of nicotine replacement therapy for people who are ready to quit. We’ll return to smoking cessation in our Term 2 Facilitating Behavior Change session.
Alcohol use
Prevalence & outcomes: About half of American adults use alcohol regularly and for one in ten, alcohol use is considered unhealthy. As illustrated below, unhealthy alcohol use is a continuum with alcohol use disorder (AUD) at one end and ‘at risk’ use, which increases the risk of both medical complications and future AUD, at the other.
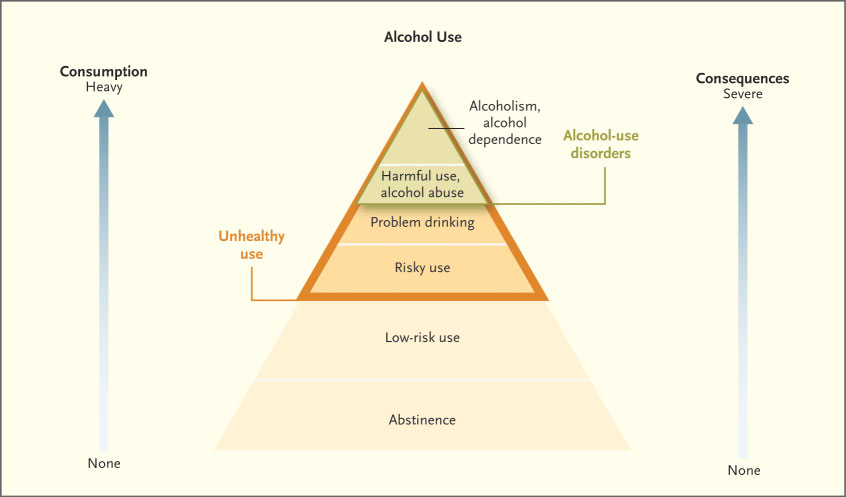
From The New England Journal of Medicine – Unhealthy Alcohol Use
Excess alcohol causes 10% of deaths in working-age adults, most due to alcoholic liver disease, car crashes, falls, and suicide, and 40% of people admitted to trauma units have alcohol in their blood. Because alcohol contributes to medical problems ranging from hypertension to sleep disorders to depression to GI bleeding, the prevalence of AUD in primary care is as high as 1 in 5 patients, and it is even higher in the hospital setting.
Impact of screening: In the primary care setting, screening and a brief counseling intervention can decrease at risk alcohol use by 40%. Primary care-based counseling is also appropriate for those with health problems exacerbated by alcohol, like sleep disorders and depression. Identification and treatment of AUD can lead to a sustained remission in 30% of people.
Screening questions: Begin by asking if your patient sometimes drinks alcohol. If the answer is yes, you can identify those with ‘at risk’ use with a single screening question about the number of drinks consumed at one time. Based on epidemiological data, at risk use is defined as 5+ drinks on a single occasion for male individuals, who typically have greater muscle mass, and 4+ drinks on a single occasion for females.
- For male patients ask, “How many times in the past year have you had 5 or more drinks on one occasion?”
- For female patients ask, “How many times in the past year have you had 4 or more drinks on one occasion?”
Next steps for a positive screen: Quantify current alcohol use per week and assess for alcohol use disorder. You will learn the diagnostic criteria in Mind, Brain and Behavior. Primary care-based counseling is appropriate for those with ‘at risk’ alcohol use while more specialized treatment would be recommended for those with alcohol use disorder.
As shown below, a standard drink is 12 oz of beer, 5 oz of wine, or 1.5 oz of distilled spirits.
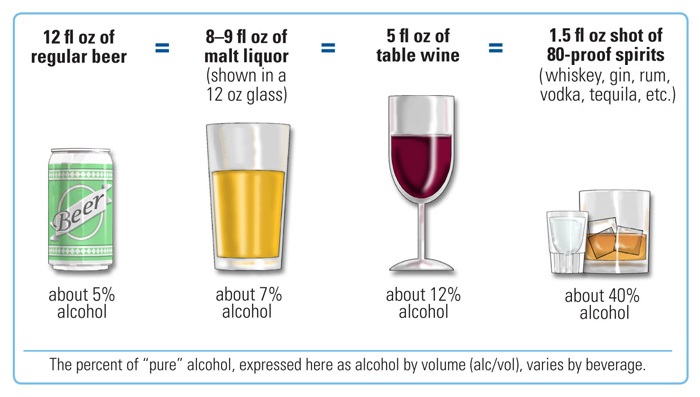
Wikipedia – Standard Drink
Other substance use
Prevalence and outcomes: On average, 115 Americans die each day of an opioid overdose, more than 40% involving a prescription drug. Drug overdose deaths are now the leading cause of death for young adults. Other commonly used substances, including sedatives like benzodiazepines, cocaine and methamphetamine each have their own effects, complications and withdrawal symptoms, which you’ll learn about in your Mind, Brain and Behavior block.
Impacts of screening: People diagnosed with opioid use disorder can be offered effective medication treatment with buprenorphine or methadone. Everyone who uses opioids can also be provided with overdose education and naloxone, which quickly reverses the respiratory depression caused by the drug. Many communities have syringe service programs that offer clean supplies and other resources to individuals with opioid use disorder.
Screening question: You can ask “How many times in the past year have you used illicit drugs or prescription drugs for non-medical reasons?” Any answer over zero is defined as a positive screen.
Next steps for a positive screen: Further history is warranted to identify and quantify substances used, and assess for substance use disorder (SUD). You’ll learn more about diagnosis and treatment of SUD next year.
In the video below, two UW specialists in addiction treatment, Drs. Joe Merrill and Ron Jackson, role play a clinic conversation about alcohol use, triggered by a positive screen on a pre-visit questionnaire. You aren’t expected to move past the first few questions at this point, but it gives an idea of how brief primary care-based counseling could make a difference.
Knowledge Check:
Beyond stigma
You learned a lot about the impact of stigmatizing language in the “The Complete Medical Database” chapter which you reviewed in Immersion. Consider referring back to this chapter and the “Addiction Treatment: Clinical Skills for Healthcare Providers” video which discusses recommended language when communicating about patients with substance use disorder.
The following video demonstrates how the stigma of substance use disorder impacts care from a patient perspective. Please watch the following video “Beyond Stigma: Treating Pain in Opioid Use Disorder”. After the video please share your thoughts to the following questions:
Add knowledge check here. Reflection on the video
Resources and References:
Behavioral Health. A Guide to Clinical Practice
- Chapter 21. Tobacco use
- Chapter 24. Unhealthy Alcohol and Other Substance Use.
- Chapter 25. Opioids
Coursera. Addiction Treatment: Clinical Skills for Healthcare Providers (free)
Screening for Substance Use from Addiction Treatment: Clinical Skills for Healthcare Providers.


