Reporting the exam
The exam is reported in a standard and predictable way, so your reader or listener can anticipate and interpret your findings. To maximize efficiency and patient comfort, a complete exam is usually PERFORMED from head-to-toe. However, it is REPORTED by organ system.
For example, the carotid pulses are checked as the neck is examined and the foot pulses are checked at the end of the exam, but these are both reported with the cardiovascular exam.
In Immersion, you will learn to report typical physical exam findings. During your blocks, you will learn much more about pathophysiology and abnormal findings. We will return to reporting the exam in each advanced physical exam workshop.
Standard vocabulary and reference points
The reference points and terms you have learned in Anatomy are also used to describe physical exam findings. These are based on the anatomic position: standing and facing forward, with the palms facing forward. Here’s a refresher.
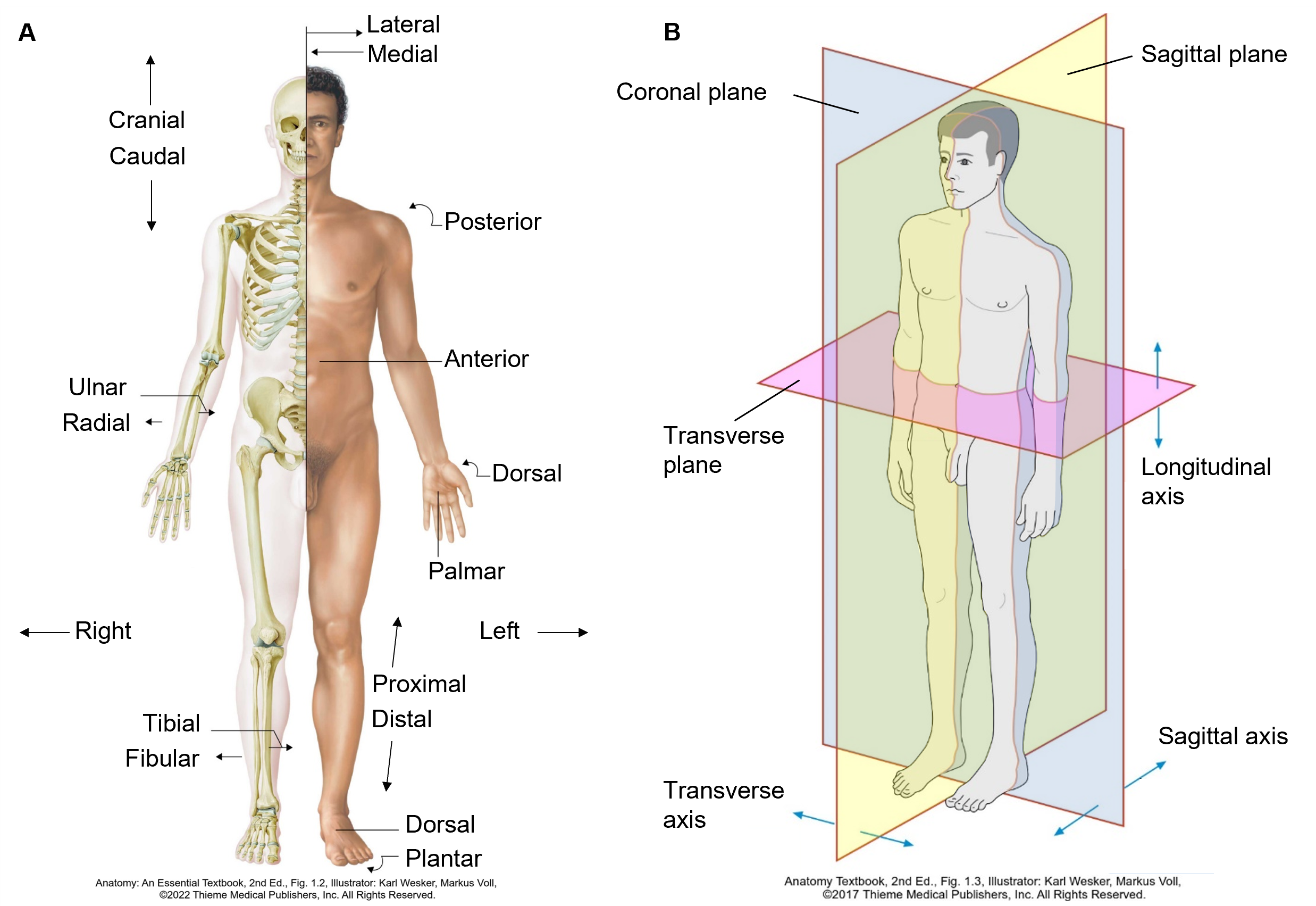
| Anatomic Term | Definition |
|---|---|
| Anterior or ventral | Near the front |
| Posterior or dorsal | Near the back |
| Superior or cranial | Upward, or near the head |
| Inferior or caudal | Downward, or near the feet |
| Medial | Toward the mid-line |
| Lateral | Away from the mid-line |
| Proximal | Closer to a reference point (often the trunk) |
| Distal | Farther from a reference point (often the trunk) |
| Sagittal plane | Divides the body into right and left parts |
| Coronal plane | Divides the body into front and back parts |
| Transverse | Divides the body into upper and lower parts (or cross-sectional plane) |
Reporting typical findings
As you learn the exam in Immersion, you should also learn how to describe the usual findings in a healthy person. The sample document below is for a healthy person with no unusual or abnormal findings.
Reporting abnormal findings
Describe abnormal findings as clearly and concisely as you can. You’ll learn more about abnormal exam findings, how to describe them, and what they mean as you complete each block. This list of common abnormalities can serve as a reference in the mean time (you don’t need to read the whole thing now).
| Skin, hair and nails | |
| Skin | For skin lesions, report location and type of lesion
Additional descriptors:
|
| Nails | Clubbing
Pitting |
| Hair: | Alopecia
Generalized alopecia of scalp, brows and lashes |
| Eyes | |
| Visual acuity | Decreased visual acuity. Note the acuity in each eye.
20/70 R eye. 20/50 L eye. |
| Visual fields | Visual field defect. Note the quadrant(s) affected, using the terms superior, inferior, nasal, and temporal to describe them.
Visual field defect in L inferotemporal visual field |
| Eyelids | Ptosis
Stye Skin lesions (see skin above) |
| External eye | Conjunctival injection
Conjunctival pallor Scleral icterus |
| Pupils | Asymmetric corneal light reflection
Absent red reflex Asymmetric pupils Decreased reaction to light R pupil 3 mm & reactive; L pupil 5 mm and nonreactive |
| Ears | |
| External ear & EAC | Swelling, tenderness or discharge |
| Tympanic membrane | Erythema or bulging
TM bulging and erythematous; landmarks not visible Presence of middle ear effusion |
| Hearing | Decreased hearing. Note method of testing. |
| Nose and sinuses | |
| Internal nose | Palloror injection of mucosa
Nasal polyps Ulcers. Note size and location. Discharge |
| Sinuses | Sinus tenderness
L maxillary sinus tender to palpation |
| Oral cavity | |
| Oral mucosa | Plaque
Ulcers Masses |
| Posterior pharynx | Erythema
Exudate Tonsillar enlargement |
| Dentition and gingivae | Caries
Gingival erythema or swelling |
| Base of tongue | Ulceration or mass (suggesting malignancy) |
| Parotid glands | Swelling |
| Temporomandibular | Tenderness or crepitus |
| Neck and thyroid exam | |
| Lymph nodes | Enlargement. Note size, tenderness, mobility, consistency and location of enlarged node(s)
2.5 cm firm, non-tender, fixed node, L posterior cervical triangle |
| Thyroid | Nodules: 1.5 cm palpable nodule, non-tender in R lobe
Enlargement: Thyroid diffusely enlarged, non-tender |
| Chest exam | |
| Inspection | Evidence of respiratory distress: tachypnea, accessory muscle use, retractions
Decreased chest expansion |
| Palpation | Asymmetric tactile fremitus
Decreased tactile fremitus ½ way up the R posterior chest Vertebral, rib, CVA or chest wall tenderness |
| Percussion | Dullness or hyperresonance to percussion.
Hyperresonant to percussion entire L chest |
| Auscultation | Adventitious sounds: fine crackles, coarse crackles, wheezes, stridor, rubs.
Coarse crackles present in the R lower lung field Decreased breath sounds Decreased breath sounds L lower lung field |
| Cardiovascular exam | |
| Inspection | Abnormal movement of the chest wall. |
| Palpation | Abnormal apical impulse: enlarged, sustained, and/or laterally displaced.
Apical impulse palpable lateral to the MCL in the 5th ICS |
| Auscultation | Abnormal rate – tachycardia or bradycardia
Irregularly irregular rhythm Presence of an S3 or S4 gallop Murmurs should be described with timing, quality location & radiation |
| Pulses | Asymmetric or absent pulses
2+ and symmetric carotid and radial pulses. Absent dorsalis pedis and posterior tibial pulses bilaterally. Bruits |
| Edema | Note the proximal extent of edema and presence of pitting or weeping;
Pitting edema to mid-thigh with weeping below the knee. Often graded from absent to 4+ (scale is subjective) 3+ pitting edema in bilateral lower extremities, up to mid-thigh |
| Abdominal exam | |
| Inspection | Scars. Describe size and location.
Distension |
| Auscultation | Abnormal bowel sounds: Hyperactive or absent. |
| Percussion & palpation | Tenderness. Note location and presence or absence of guarding.
RUQ tender to palpation, with involuntary guarding. Abnormal liver size or consistency |
| Neurologic exam | |
| Mental status | Abnormal level of consciousness: lethargic, obtunded or comatose
Abnormal orientation Oriented x 2 (to self and place only) Abnormal recall Recalls 1/3 items at 5 minutes. |
| Cranial nerves | Note the affected nerve(s) and how each abnormality was detected.
CN II-XII are intact, except for R CN VI. Pt is unable to abduct R eye. |
| Motor: | Abnormal strength. Compare side to side and grade 0-5.
Strength 5/5 in all major muscle groups except 4-/5 in R hip flexors Abnormal bulk: Bulk is normal in UE and LLE. Atrophy of R calf and foot muscles noted |
| Reflexes: | Abnormal Babinski reflex
Toes upgoing on R Asymmetric or changing reflexes. Compare side to side and grade 0-4. Reflexes 1+ at biceps, triceps & patella. L Achilles 1+, R Achilles 4+ |
| Sensation | Describe the location of abnormal sensation and modalities tested
Decreased sensation to light touch from toes to knees bilaterally Positive Romberg |
| Cerebellar | Describe the abnormal test
Finger to nose test abnormal with bilateral dysmetria |
Problem focused exam
In Immersion, you will learn a comprehensive exam but in your Primary Care Practicum, you will rarely see your preceptors perform as complete an exam on one patient. They are much more likely to perform an exam focused on the one or two organ systems most relevant to the reason the patient is being seen. This problem focused exam is used to answer specific clinical questions about the patient you are seeing.
| Examples of clinical questions | Problem focused exam |
|---|---|
| Is my patient with heart failure on enough water pills (diuretics)? |
|
| Is my pediatric patient developing as expected? |
|
| Is my patient with diabetes developing complications? |
|
| Does my patient’s back pain have a serious cause? |
|
