Reproductive organs, rectal and breast exams
In adults, these exams may be performed to evaluate a specific concern. In selected patients, they may also be used to screen for some cancers. The physical exam you perform for a patient should be based on the clinical concern and the anatomy present. By the time you complete the Patient Care Phase, you should be able to perform the following exams. We introduce the exam in FCM to provide a safe and supportive learning environment and allow you to practice in PCP if the opportunity arises. You will not be expected to perform these exams on a Foundations OSCE.
Penis, scrotum and testes
- Inspect the glans, corona, and meatus, retracting the foreskin if the patient is uncircumscribed
- Compress the glans gently to inspect for discharge.
- Inspect the shaft of the penis.
- Inspect the scrotum.
- Palpate the shaft of the penis.
- Palpate the testes and epididymis gently between the thumb and forefinger.
- Palpate the spermatic cord.
Hernia exam
- Examine for hernias bilaterally by using the index finger or the fifth finger to carry a fold of scrotal skin into the inguinal canal and asking the patient to bear down or cough.
Digital rectal exam
- Examine the anal orifice.
- If applicable, palpate the prostate
- Palpate the rectal mucosa
Examination of the Vulva and Introitus
- Inspect:
- Hair pattern
- Skin
- Labia majora and minora
- Urethra
- Introitus and hymen
- Inspect the perineal region for lesions, ulcers, fissures or scars
- Inspect the perianal region for external hemorrhoids, fissures, and other lesions
Speculum Examination of the Vulva and Introitus
- Choose an appropriate size and shape of speculum, lubricated with water or a small amount of lubricant.
- Insert the speculum
- Examine the cervix
- Examine the vagina
Bimanual Examination of the Uterus and Ovaries
- Palpate the cervix and assess for size, mobility, & tenderness with gentle movement
- Examine the uterus and ovaries
Breast exam
- Inspect
- Breast symmetry, contour, shape, nipple inversion, skin changes
- Palpate
- Breast tissue for any masses
- Axilla looking for lymphadenopathy
Trauma-informed approach to sensitive exams
Although a trauma-informed approach is important for any physical exam, it is particularly important for these exams, which may provoke a significant trauma response for affected people. They can activate overwhelming emotions, unwanted or intrusive thoughts, traumatic memories and feelings of detachment from the body. The patient-provider power differential may be heightened, and many patients will feel unable to inform their physician of these feelings. Because trauma is so common, experts suggest using a trauma-informed approach to every patient.
To provide a safe and supportive learning environment, you will first practice these exams on paid patient models in FCM. They are experienced educators whose goal is to prepare the next generation of providers to perform these sensitive exams in a comfortable and trauma-informed manner. We recognize that performing sensitive exams is stressful for most learners and may activate a trauma response in some people. Please let us know if there is some way we can support you
Trauma informed PE: Before the exam
It is ideal to meet your patient on equal footing, fully dressed, to establish rapport and an agenda for the visit. A new patient’s agenda may not include these exams at the first encounter. If a sensitive exam is planned:
- Ask about past experience.
- Ask for their suggestions. Would they like a support person present? Is there language that your patient prefers to use to refer to their body?
- Advise the patient that they have control over the exam – it can be paused or stopped at any time
- “Is there anything I can do to make the exam more comfortable for you?”
- “Please tell me at any point if I am inadvertently causing you discomfort.”
Trauma informed PE: During the exam
- Foster the comfort and modesty of your patient with appropriate draping and exposure.
- Allow patient to move their own gown, clothing or drape or ask permission before moving it.
- Speak clearly, slowly, and at an appropriate volume
- Appear engaged, pleasant, calm
- Ask for permission before conducting each section of the examination.
- Describe what you plan to do before doing it
- Watch and listen carefully for signs of a trauma response. These can include flushing, trembling, shutting eyes, not responding to questions, or difficulty hearing or seeing clearly. If you observe any of these signs, pause to offer support. The exam may not be able to be completed today
Trauma informed PE: After the exam
- Provide sensitive closure
- Discuss results and ask for questions
Remember that not all patients who may need an exam of the penis, testicles, cervix , etc. identify as men or women- Trans and gender non-conforming people are more likely to have had prior negative experiences in health care setting, making a trauma-informed approach particularly important.
UCSF Center for Excellence in Transgender Health Guidelines for Physical Exam
Physical examination should be relevant to the anatomy that is present, regardless of gender presentation, and without assumptions as to anatomy or identity. Sensitive history taking is required to understand the myriad and individualized changes and characteristics in the context of hormone administration and surgical intervention. Consideration should be given throughout the visit to potential prior negative experiences within the health care setting, including discrimination as well as physical or emotional abuse.
When conducting a physical exam, providers should use a gender affirming approach. Gender affirmation is when an individual is affirmed in their gender identity through social interactions. This includes being referred to by the correct name and pronouns during the entire visit. This may also include using general terminology for body parts or asking patients if they have a preferred term to be used. An examination should only be performed of those body parts that pertain to the reason for a specific visit. For example, examination of the genitalia is not appropriate in the context of an acute visit for an upper respiratory infection.
Male genitourinary exam
Penis, scrotum and testes
- Inspect the glans, corona, and meatus, retracting the foreskin if the patient is uncircumscribed
- Compress the glans gently to inspect for discharge.
- Inspect the shaft of the penis.
- Inspect the scrotum.
- Palpate the shaft of the penis.
- Palpate the testes and epididymis gently between the thumb and forefinger.
- Palpate the spermatic cord.
Hernia exam
- Examine for hernias bilaterally by using the index finger or the fifth finger to carry a fold of scrotal skin into the inguinal canal and asking the patient to bear down or cough.
Exam Video:
Exam steps
External genitalia: Inspection
- Put on gloves
- Inspect the glans, corona, and meatus, retracting the foreskin of the penis if the patient is uncircumcised. If the foreskin is painful or tight, do not retract it. This is called phimosis and is normal in young, uncircumsised children. In older people, it can be caused by infection or inflammation.
- After inspecting the glans make sure to return the foreskin to its usual state covering the glans. Failure to return the foreskin could result in paraphimosis, swelling of the glans, which can progress to a urological emergency.
- Compress the glans gently to inspect for purulent discharge, which can be seen with urethritis caused by an STI or by prostatitis. Clear discharge is often normal if seen.
- Inspect the shaft of the penis.
- Inspect the scrotum.
External genitalia: Palpation
- Palpate the shaft of the penis, observing for nodules or fibrosis.
- Palpate the testes and epididymis gently between the thumb and forefinger, observing for masses and tenderness.
- Palpate the spermatic cord
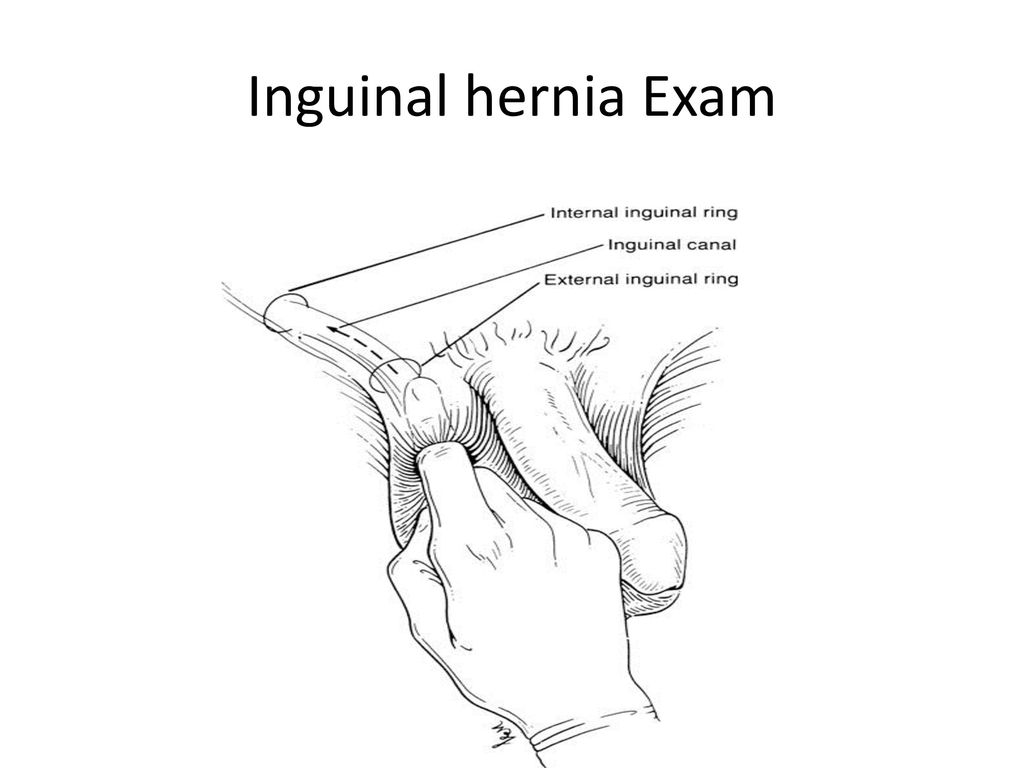 Examine for hernias.
Examine for hernias.
A hernia is a protrusion of the abdominal contents through the inguinal canal.
To examine for hernias, you would ideally be seated on a stool, with your palm facing the patient’s scrotum. Using the index finger or the fifth finger, carry a fold of scrotal skin into the inguinal canal and asking the patient to bear down or cough. Most examiners use the right index finger to examine the patient’s left inguinal canal and the left index finger to examine their right side. With your finger in place, ask the patient to bear down or cough. Feel for a bulge hitting the examining finger from above indicating the presence of an inguinal hernia.
Inguinal hernias are often diagnosed on exam, but distinguishing between direct hernias and direct hernias indirect hernia can be challenging often requires additional imaging. Sometimes the final distinction is not confirmed until the patient is in surgery to treat the hernia.
Rectal exam
Rectal exam
- Examine the anal orifice.
- If applicable, palpate the prostate
- Palpate the rectal mucosa.
If the rectal exam is performed after the exam of the penis and scrotum in the outpatient clinic, the patient is often positioned leaning over the exam table with the legs shoulder width apart. This is the position we will practice with our patient models. Some patients may be more comfortable lying on one side, with one or both knees pulled up towards the chest. The rectal exam may also be performed at the end of the female pelvic exam. You should take into account any preference’s shared by your patient as well as the setting (hospital vs. clinic), the clinical question the exam is addressing, and your patient’s mobility.
 Spread the buttocks and examine the anal orifice. You may note skin tags, anal fissures or hemorrhoids. When in doubt, note their position and seek additional guidance.
Spread the buttocks and examine the anal orifice. You may note skin tags, anal fissures or hemorrhoids. When in doubt, note their position and seek additional guidance.- Using lubricating jelly, press forefinger pad against the anus and then insert gently into rectum.
- As appropriate, palpate the prostate. The prostate exam is usually done to evaluate a specific concern, such as urinary hesitancy or weak stream suggesting benign prostatic hypertrophy, prostate cancer or symptoms of infection suggesting prostatitis. Along the anterior wall of the rectum, first palpate the posterior lobe of the prostate, then examine the lateral lobes. The normal prostate is usually about the size of a walnut and the consistency is similar to that of the tensed thenar eminence of the hand when tensed. Note the size, consistency, symmetry relative to the median sulcus, tenderness, and the presence of nodules. Nodules from prostate cancer may feel like a pebble.
- Rotate the finger clockwise and counter clockwise 180 degrees to palpate the rectal mucosa for masses.
- With the patient straining downward, which helps to relax the external sphincter, withdraw the finger. We no longer routinely check stool for occult blood as part of the rectal exam. If concerned about gastrointestional bleeding it is more important to note the color and consistency of the stool. There are several different colon cancer screening modalities that are used instead of testing for occult blood as part of the rectal exam. Which colon cancer screening test is appropriate depends upon your patient’s risk profile.
- Let the patient know the exam is complete, re-drape, and offer tissues to remove excess lubricant.
Female pelvic exam
The female pelvic exam is performed to screen for cervical cancer and to evaluate abdominal, pelvic, or gynecologic concerns. We will introduce the exam in FCM and you will gain additional experience in the Obstetrics and Gynecology clerkship. On completion of the Patient Care Phase, you will be expected to be able to:
Examine the Vulva and Introitus
- Inspect:
- Hair pattern
- Skin
- Labia majora and minora
- Urethra
- Introitus and hymen
- Inspect the perineal region for lesions, ulcers, fissures or scars
- Inspect the perianal region for external hemorrhoids, fissures, and other lesions
Perform a Speculum Examination
- Choose an appropriate size and shape of speculum, lubricated with water or a small amount of lubricant.
- Insert the speculum
- Examine the cervix
- Examine the vagina
Perform a Bimanual Examination
- Palpate the cervix and assess for size, mobility, & tenderness with gentle movement
- Examine the uterus and ovaries
Stanford Pelvic Exam Video
To prepare for the pelvic exam workshop, please view this video from the Stanford 25.
Past UWSOM students raised concerns about this video as the model’s consent was not clearly indicated. When our colleagues at Stanford put us in touch with her, she sent this message.
“I am a 55 year black woman who has served as a Gynecological Teaching Associate and Standardized patient at The University of Michigan, Stanford University, UCSF, Touro University in Vallejo, California and in Henderson, NV for over 20 years. I am empowered and have chosen to train medical students with my body and share my perspective/experience in a teaching capacity. Because, I know it has and will continue to promote safe, respectful and honoring exams. I have done thousands of breast and pelvic exams, and give my consent freely for teaching purposes… In these sensitive exams I emphasize that they are not to be entered into or held in any sexual way.”
We deeply appreciate her work as well as that of the Gynecological Teaching Associates with whom you will learn the exam.
Choosing appropriate language
As you learn to perform the exam, pay careful attention to the words that you choose. Language should be clinical rather than personal and should avoid any possible sexual connotations. Common phrases you may hear and more appropriate alternatives are summarized below. Adapted from Elisseou, MedEdPORTAL 2019; 15; 10799.
| DON’T SAY | INSTEAD SAY |
| Stirrups | Footrests |
| Sheet | Drape |
| Bed | Exam table |
| That looks good | That looks healthy |
| I want to | I am going to |
| Look at | Inspect |
| Feel or touch | Examine or evaluate |
| Relax | Take slow deep breaths and feel your muscles loosen |
| For me | Do not use this phrase |
| Open your legs | Allow the knees to relax apart |
| Butt | Bottom |
| Your | The |
Identifying an assistant or chaperone
In general, it is good practice to have a medical assistant or nurse in the room during sensitive exams and to document in your note that an assistant was present. Ideally, the assistant would be of the same gender as the patient but sometimes that may not be possible. Always let the patient know the gender of the assistant that is available and ask if they are comfortable with that person. If not, the exam may need to be postponed until an appropriate assistant is available.
Preparing your equipment
- Gown and drape
- Speculum and water-soluble lubricant
- Light source
- Gloves should be worn on both hands throughout the exam
- Cotton swabs
- Specimen collection material for cervical cancer screening, STI testing, and/or wet mount
The speculum separates the walls of the vagina. The Pederson speculum is narrow, with flat blades and should be used first for patients who are not sexually active. The Graves speculum is biconcave with larger blades and allows better visualization of the cervix and vaginal walls for parous or larger-bodied patients who may have more tissue. Both styles of speculum come in different sizes and may be made of metal or of disposable plastic. Patients may know or provider notes may indicate which speculum was successfully used for previous exams.
Patient preparation & positioning
Voiding prior to the exam can make it more comfortable. If indicated, collect a urine sample for pregnancy testing, urinalysis or STI testing. Provide privacy as your patient changes into a gown. A drape is placed over the lap and moved as needed.

Help the patient to the correct position, adjusting their pillow and the exam table as needed for comfort. The feet have historically been positioned in footrests as seen in the video. This position may be uncomfortable and it can be activating for some trans people or for those with a history of sexual trauma. An alternative is to position the feet on the slider board of the extended exam table, which allows the patient to move and change positions more easily. Some providers feel this better positions the pelvis for the speculum exam and some (but not all) patients may find this more comfortable.
The image at right shows feet positioned on the slider board, from Empowering Gynecologic Care: Speculum care without stirrups, used with permission.
Beginning the exam
Position yourself at eye level with your patient and maintain eye contact when possible. Avoid sudden movement and leaving the patient’s field of vision, which can be triggering. Throughout the exam, give the patient as much control as you can, for example, by saying “Please stop me at any point if I am inadvertently causing you discomfort.”
Place your hands outside of the knees at the appropriate distance, then ask your patient to ‘relax the knees to the sides until they touch my hands’ or as far as is comfortable for them. Never push the knees apart, even with gentle pressure.
Ask the patient to move the drape so the area is exposed and adjust as needed to allow the exam. Introduce touch with the back of your hand first, warning the patient as they cannot see your hands. Continue to describe each step of the exam before you perform it, warning the patient before any new area is examined.
Examining the vulva and introitus
Next inspect the:
- Hair pattern over lower abdomen, groin, and mons pubis
- Skin for changes, concerning nevi, and any other lesions
- Labia majora and minora
- Urethra
- Introitus and hymen
Inspect the perineal region for lesions, ulcers, fissures or scars
Inspect the perianal region for external hemorrhoids, fissures, and other lesions
Speculum Examination
The speculum should be lubricated with water or a small amount of water-soluble lubricant.
Insert the speculum as follows:
- Separate the labia gently with your gloved fingers
- Insert the speculum with the “blades” of the speculum closed and oriented horizontally, with some pressure exerted downwards along the posterior wall of the vagina to avoid the sensitive urethral area. Avoid pinching the vulvar tissue or inadvertently pulling pubic hair.
- Pass the speculum along the axis of the vagina
- Open the speculum blades; adjust the speculum and light as needed to visualize the cervix
Examine the cervix:
/Cervix_birth-567fc3053df78ccc15961647.png) Note shape of the os. A nonparous cervix is round and pink, with a central os while the os in a parous cervix tends to be horizontal or even “fish-mouthed” in shape.
Note shape of the os. A nonparous cervix is round and pink, with a central os while the os in a parous cervix tends to be horizontal or even “fish-mouthed” in shape.- The squamocolumnar junction is where the external pink squamous mucosa of the cervix meets the darker colored columnar epithelium of the endocervical canal. BOTH squamous and columnar cells must be sampled for cervical cancer screening to be optimal.
- Obtain a sample for cervical cancer screening. Different clinics use different acquisition techniques so ask your preceptor at each new site.
- Spatula: place longer end of spatula into cervical os & scrape 360°
- Cytobrush: place brush inside endocervix and rotate it in one direction. Attempt to get all bristles within the canal to ensure adequate sample. Only rotate in one direction.
- For liquid cytology medium, place the spatula and cytobrush in the jar and transfer cells into the liquid by swishing for 10 seconds
- For glass slides, carefully wipe the spatula and roll the brush on the slide and immediately place in or spray with fixative
Examine the vagina:
- If indicated, obtain a sample of vaginal discharge from the posterior fornix
- If indicated, swab the vaginal walls to test for gonorrhea, chlamydia, and trichomonas.
- Inspect all four vaginal walls with speculum in place and as the speculum is withdrawn
Bimanual examination
- Gently separate the labia and insert your lubricated and gloved index and middle fingers of your dominant hand into the vagina. Exert pressure downward (posteriorly) to avoid the sensitive urethral area anteriorly.
- Palpate the cervix and assess for size, mobility and tenderness with gentle movement
- With your non-dominant hand on the lower abdomen cephalad to the symphysis pubis, and your intravaginal fingers posterior to the cervix “elevating” the uterus towards the abdominal hand, assess the uterus for position, flexion, size, masses, mobility, consistency, and tenderness.
- Shift your abdominal hand to either side of the midline, and with the intravaginal fingers in first one and then the other lateral fornix; evaluate the adnexa for size, mobility, consistency, and tenderness. Prior to menopause, the normal ovaries are 3.5-4 cm in their longest diameter. After menopause, the ovaries decrease to about 2 cm in size and are usually not palpable.
- Withdraw the fingers, offer a warm washcloth to remove lubricant and help them return to a sitting position
Sample Documentation
Breast exam
The breast exam should be performed for any patient with breast or chest concerns and is sometimes part of a routine wellness screening exam. Some people prefer to use the word “chest” to refer to their own bodies. As with all patient-centered communication, adapt your language and terms to those used by your patient.
We will introduce the exam in FCM and you will gain additional experience in the Obstetrics and Gynecology, Internal and Family Medicine clerkships. On completion of the Patient Care Phase, you will be expected to be able to:
- Inspect
- Breast symmetry, contour, shape, nipple inversion, skin changes
- Palpate
- Breast tissue for any masses
- Axilla looking for lymphadenopathy
Breast Exam Video
Inspection
- With the patient seated, gown lowered to waist, ask the patient to sit with arms relaxed at their sides.
- With the patient’s arms at their sides, inspect specifically for asymmetry in breast contour or shape, nipple inversion and skin changes
- Have the patient press their hands against their hips to contract the pectoral muscles and observe for dimpling of the skin induced by this maneuver.
Tips on Technique:
- Explain to the patient what you are looking for as you complete inspection.
- For patients with large breasts, have them raise their arms overhead as you complete inspection for better visualization.
Palpation (breast)

- Have the patient replace the gown and lay supine on the exam table.
- Have the patient place the ipsilateral hand behind their head, proximal arm against the exam table, to flatten the breast tissue against the chest wall.
- Using the pads of the 2nd, 3rd, and 4th fingers on your dominant hand, palpate with overlapping dime-sized circular movements.’
- Use three different levels of pressure as you examine each region – light pressure for the subcutaneous tissue, medium pressure for the breast tissue that lies slightly deeper, and deep pressure to palpate along the chest wall.
- Start palpating the breast tissue at the axilla, moving in a “vertical strip” pattern superior to inferior, then inferior to superior, and so on, overlapping “strips” as you work from lateral to medial.
- The tissue underlying the nipple should be examined in the same fashion as the other breast tissue.
- Think of the breast tissue as encompassing a pentagonal area on the anterior chest wall, bordered laterally by the midaxillary line, medially by the sternum, superiorly by the clavicle, superolaterally by a line between the lateral clavicle and mid-axillary line, and inferiorly by the inframammary ridge at ribs 5-6. All areas of the breast must be examined thoroughly.
Tips on Technique:
- Make sure your fingernails are trimmed and hands are warm before performing the breast exam.
- For an adequate exam, the breast tissue must lie on top of the chest wall as the examiner is palpating. For patients with large or pendulous breasts, placing a pillow or blanket under the ipsilateral shoulder may help move the breast tissue directly onto the chest wall.
- Squeezing the nipple to express discharge is not diagnostically useful – this can be uncomfortable for patients, and only spontaneous discharge requires further diagnostic workup.
- The sensitivity of the clinical breast exam is directly related to the amount of time spent on the exam. The length of time needed to perform an appropriate breast exam depends on many factors, including the size of the patient’s breasts, and this exam may take up to five minutes in each breast to complete.
Palpation (axilla)
- With patient seated, gown lowered to waist, abduct the patient’s R arm with your non-dominant hand.
- With your dominant hand, place your fingers high in the axilla with your palm against the patient’s chest wall.
- Lower the patient’s arm to their side, then palpate the axillary lymph nodes with your dominant hand: lateral, central, subscapular, and pectoral.
- Use the same technique on the opposite side, using your non-dominant hand to support the arm and your dominant hand to palpate axillary lymph nodes.
- There are four major groups of axillary lymph nodes in the following locations: behind the lateral aspect of the pectoralis major, just against the chest wall, against the medial aspect of the proximal humerus, and at the lateral aspect of the latissimus dorsi.
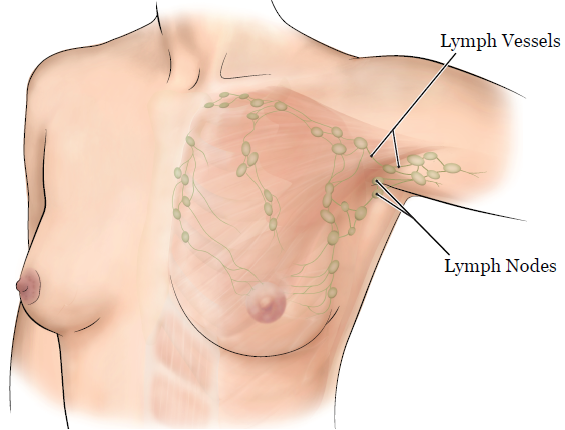
Tips on Technique
- The axillary exam is often combined with the breast exam since some breast cancers present with axillary lymphadenopathy. It is also important in patients with suspected systemic and hematologic malignancies and those with symptoms of localized infection.
- Use a circular motion to palpate lymph nodes. Lymph nodes are enlarged if they are over 1 cm in diameter. When palpated, note the following: location, size, consistency, tenderness, and degree of fixation.
Sample documentation
Knowledge check
Genitals, their function, and sexuality have cultural, religious, and social connotations. For example, “impotent” can mean “powerless” or describe the inability to get or keep an erection. Colloquial terms for the penis and the vagina are often used pejoratively. Advertisements for testosterone supplementation and erectile aids are commonly heard on television and radio.
Before completing the knowledge check questions below, consider taking 5-10 minutes for reflection:
- What comes up for you when you think about genitals and sexuality?
- What expectations do you have of genitourinary examinations? Are they different as a patient and as a student doctor?
- What messages do patients receive from others about genitals and sexuality?
- What can you do to foster a safe space for yourself and your patients around GU concerns?
References & Resources
Ravi A and Little V. Curbside Consultation: Providing Trauma Informed Care. American Family Physician 2017. 95(10): 655-57 Full text
Elisseou s., Puranam S. and Nandi M. A Novel, Trauma-Informed Physical Examination Curriculum for First-Year Medical Students. MedEdPORTAL 2019; 15; 10799. Full text
Empowering Gynecologic Care: Speculum care without stirrups.

