Hospital Tutorial Write-ups
Medical notes record the data you have gathered and your medical decision-making in a concise, well-organized, and standard way. These notes communicate your findings with other members of the team and serve as legal documentation of the care that has been provided. In FCM, your hospital tutorial write-ups will give you practice in writing comprehensive notes, like those you’ll write in third year for new patients.
Almost all health systems now use electronic health records for documentation. We teach you to write notes from scratch because the structure and your clinical reasoning should be very similar in a written and in an electronic note. Written notes will build good habits and allow your mentors to provide you with better feedback. Plus, most of our first year students don’t have access to the EHR at their clinical sites, and even if you did, we want you to learn to collect information from your patient yourself rather than use information collected by others
Your FCM write-ups should have the following structure – more details on each section are included below.
| Section | Content of this section |
| Identifying Information & Chief Concern | Name, age |
| Known medical problems highly relevant to the chief concern (< 4) | |
| Chief concern and duration of symptoms | |
| History of Present illness | Background: Health at the time of symptom onset and details of any chronic illness directly related to the chief concern |
| Details of the presenting problem beginning at symptom onset & proceeding sequentially | |
| Predisposing conditions & risk factors | |
| Pertinent negatives | |
| Optional: Hospital course or evaluation to date | |
| Past Medical History | All active medical problems and any other problems relevant to evaluation or ongoing management |
| Summarize for each major, active problem: diagnosis, current treatment, control, and complications | |
| Medications & Allergies | Prescribed medications and doses |
| Non-prescription medications and complementary therapies | |
| Drug allergies and the type of reaction | |
| Health-Related Behaviors | Substance use: Tobacco, alcohol, recreational drugs
Diet & exercise Sexual history Preventive Health |
| Family Medical History | Family history of illnesses and causes of death affecting first degree relatives |
| Social History | Full social history, including influences on your patient’s health and health care: living situation, social support, occupation and avocation, any financial or other concerns, sexual orientation (if not included in sexual history), gender identity & assigned sex at birth, cultural identity |
| Review of Systems | List all systems and note the presence or absence of each symptom you asked about. For organ system(s) discussed in HPI, write “see HPI” |
| Provide details of positive responses to ROS questions | |
| Physical Exam | General appearance and vital signs |
| Document each organ system in order and report all exam findings, both normal and abnormal | |
| Labs and Imaging | Not part of the FCM write-up. Should be reported after the physical exam in later notes. |
| Summary Statement | Restate the ID & summarize the key features from the history & physical exam |
| Branching Diagram or Diagnosis Matrix | A visual representation of your clinical reasoning process. Not included in Term 3 or later write-ups. |
| Assessment | Format determined by clinical context |
| Plan | Includes diagnostic and treatment plan, monitoring/follow-up and patient education |
Identifying data & chief concern
Purpose: Sets the stage and gives a brief synopsis of the patient’s major problem
Format:
Identify the patient by name and age. You can include gender if it has been confirmed or sex if relevant to the CC.
Include no more than 4 medical problems (sometimes there are zero) that are highly relevant to the chief concern. List only the diagnoses here & elaborate on them in the HPI or PMH.
Report the chief concern and duration of symptoms
History of present illness
| HPI | Background: Health at the time of symptom onset and details of any chronic illness directly related to the chief concern. |
| Details of the presenting problem beginning at symptom onset & proceeding sequentially. | |
| Predisposing conditions & risk factors (‘pertinent positives’) | |
| Pertinent negatives | |
| Optional: Hospital course or evaluation to date |
Purpose: Provides a complete account of the presenting problem. Includes any information from the past medical history, family history and social history that is directly related to the presenting problem.
Format: One framework commonly used to structure the HPI is:
Background
Characterize the patient’s health at the time current symptoms began. If the symptoms are related to a chronic illness, give a brief summary of the illness, including when it was diagnosed, treatment, complications, and how well it is controlled.
Example 1. MR was in his usual state of good health until the day before admission when …
Example 2. ST has a history of coronary artery disease and had a myocardial infarction 6 months ago. He has had stable chest pain with exertion since that time, until the morning of admission when…
Details of the presenting problem
This is an organized and edited version of the patient’s narrative, beginning at the onset of symptoms, and proceeding sequentially to the time of presentation. In FCM, your write-ups should be written as though you were present at the time of admission. Focus on the initial symptoms and presentation, rather than what has happened since hospitalization. This will allow you to practice clinical reasoning more effectively.
Predisposing conditions and risk factors
These are sometimes called ‘pertinent positives’ – the past medical history, health related behaviors, family history, or review of symptoms that is directly related to the presenting problem. For example, a family history of liver problems is pertinent and should be included in the HPI of a patient who presents with jaundice. The same family history would NOT be pertinent to a suspected UTI, so would NOT be included in the HPI.
Pertinent negatives
Pertinent negatives are the absence of symptoms from the organ system(s) involved and negative information from the rest of the history that directly affects your assessment of the patient’s problem. For example, “No family history of liver disease” is a pertinent negative in a patient presenting with jaundice.
Optional – hospital course or evaluation to date:
Here you can summarize what has occurred since the admission – significant events, testing, and how the patient is doing now. Since you will be getting this information from the patient rather than the medical record, you will probably not have all of the details. Save this information until the end of the HPI and practice constructing the first paragraphs as though YOU were assessing the patient’s presenting concern, rather than relying on information about what other doctors have said or done.
Past medical history
Purpose: A comprehensive summary of all medical and surgical problems, both current and resolved.
Format: Use a bulleted list with additional details and explanations when appropriate.
-
- Major childhood illnesses
- Medical problems, including psychiatric illnesses. You can simply list problems that have resolved. For each ongoing problem, outline:
- Onset – date and presenting symptoms or testing if known
- Treatment and current control
- Complications
- Surgeries (type of surgery and date)
- Traumas
- Obstetrical history, if applicable
Medications & allergies
Purpose: Document medications taken at home, to ensure appropriate therapy is being given and drug interactions are minimized. In the EHR, medications are documented in a separate area and should be updated at each outpatient visit. In the hospital, electronic chart notes may include the list of medications that are being administered based on orders and pharmacy records.
Format:
- List all prescribed medications by generic name. Include doses if possible
- List over the counter medications
- List complementary/alternative medicines
- List medication allergies including the reaction
Health Related Behaviors
Format: May be written as a bulleted list or in sentence format in FCM notes. In an EHR, this information is often collected in a separate field. It includes:
- Diet and exercise
- Tobacco (in pack-years, current amount, and stop date if applicable)
- Alcohol (past and current amount, stop date if applicable)
- Drugs (past and current amount, stop date if applicable)
- Sexual history (primarily sexual behavior; sexual orientation and gender identity may be included in social history)
- Preventive health can be included but is more applicable in the clinic. Here you can note immunizations, appropriate screening (Pap smears, colonoscopy, etc.), safety
Family history
Format: List first degree relatives (grandparents, parents, siblings and children) and major diseases each was affected by, including coronary artery disease, cancer, diabetes, alcoholism, genetic diseases, or major psychiatric illness. You may also use a genogram.
Social History
| Social History | This may include influences on your patient’s health and health care: living situation, social support, occupation and avocation, any financial or other concerns, sexual orientation (if not included in sexual history), gender identity & assigned sex at birth, cultural identity |
Length: ~ ½ page
Purpose: To understand the impact of education, culture, religion, income and social support on the patient’s health and health care.
Format: Written in paragraph form and includes at least some of the following:
-
- Occupation and current employment
- Upbringing, education, and family relationships
- Current living situation and sources of support
- Financial and insurance issues
- Stresses, satisfaction, interests
- Religious/spiritual support
- Cultural identity
- Sexual orientation
- Gender identity
Review of Systems
| Review of Systems | List all systems and note the presence or absence of each symptom you asked about. For organ system(s) discussed in HPI, write “see HPI” |
| Provide details of positive responses to ROS questions |
Length: ~ 1/2 page
Purpose: Identify additional symptoms that require attention or evaluation. If you uncover symptoms in this section of the interview that could be related to your differential diagnosis, you report them in the HPI rather than in this section of the writeup. Remember that diagnoses belong in the HPI or PMH; symptoms belong in the ROS.
Format:
List all the review of symptoms for each system not discussed in HPI—for organ systems relevant to the presenting complaint, write “see HPI”
Provide details of positive responses to ROS questions
Physical Exam
| Physical Exam | General appearance and vital signs |
| Document each organ system in order and report all exam findings, both normal and abnormal. |
Length: 1-2 pages
Purpose: to describe your exam findings, highlighting those that support or argue against items on your differential diagnosis.
Format:
Begin with one sentence description of general appearance and comfort level
List vital signs: Blood pressure, pulse, respiratory rate, temperature, oxygen saturation (if known)
List in outline form a system-by-system description:
-
- Skin
- Head, ears, eyes, nose, throat (HEENT)
- Chest/pulmonary
- Cardiovascular
- Abdomen
- Genital/pelvic/rectal (omitted in FCM)
- Extremities/musculoskeletal
- Neurologic
- Skin
Be complete: describe what you found, both positive & negative findings. Do not just write “normal.” We want you to practice the language you would use to document findings important to your differential. You can shorten your writeups later.
Do not interpret findings. Document only what you see, hear or feel
| Labs and Imaging | Results of testing are documented after the physical exam in Clerkships |
Summary Statement
| Summary Statement | Restate the ID & summarize the key features from the history & physical exam |
Length: 1-2 sentences
Purpose: Synthesize the important history and exam findings, to frame the clinical problem and to lead your listener to your assessment. This is not simply a restatement of the ID chief concern as you add key features identified in your H&P. It is similar to the mental ‘problem representation’ created by experienced clinicians as they perform an H&P.
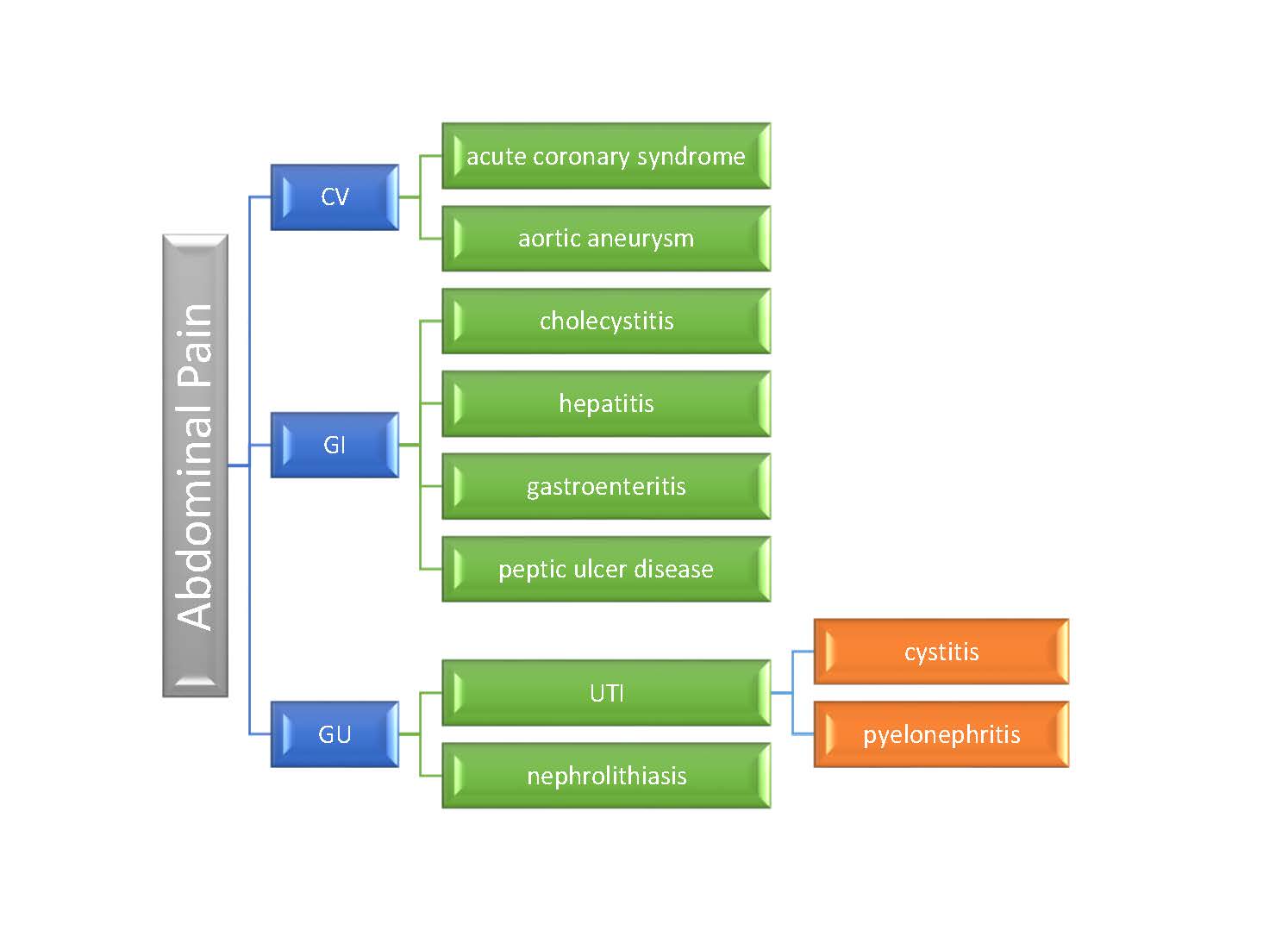
Branching Diagram or Diagnosis Matrix
| Branching Diagram or Diagnosis Matrix | Visual representation of your clinical reasoning process, included in Term 1 write-ups |
Branching diagram
Purpose: A branching diagram is an educational tool that will help you develop and organize a complete differential diagnosis. You will not see a branching diagram in real notes, but you will see your teachers use a similar structure to outline their approach to common concerns.
Format:
Begin with a symptom, physical exam finding, or other interesting feature of the case
Link possible causes to the primary symptom/finding/feature in an organized manner. Templates are available on Canvas.
Diagnosis Matrix
Purpose: Another tool for organizing and elaborating on your differential diagnosis. This matrix format allows you to compare the history, risk factor & exam finding of your leading possibilities. You will include a matrix in your Term 2 writeups. A template is available on Canvas.
Format:
Begin with a differential of the 3-5 most likely or “can’t miss” causes of the patient’s presenting problem
Record the typical or common findings in each section of the matrix, and bold or highlight those present in your patient.
|
BILATERAL LEG EDEMA |
History of Present Illness |
Predisposing conditions & Risk Factors |
Physical Exam Features |
|
CHF |
Edema
Dyspnea, orthopnea, PND Weight gain Decreased exercise tolerance |
Coronary artery disease
Severe lung disease Cardiac risk factors |
Elevated JVP
Enlarged or displaced PMI S3 Crackles Hepatojugular reflux |
|
Cirrhosis |
Edema
Increased abdominal girth Weight gain Jaundice |
Alcohol Use Disorder
Viral hepatitis Injection drug use FHx of liver disease |
Normal JVP
Ascites Spider angiomas Jaundice Splenomegaly |
|
Venous Stasis |
Edema
Skin discoloration or ulceration |
Prior DVT
Obesity |
Hemosiderin deposition in skin
Ulcerations Normal cardiac exam |
Assessment
| Assessment | Format determined by clinical context |
Purpose: Explicitly state your clinical reasoning after you have read about your patient’s chief concern or medical problem.
Format for a new problem:
Begin with a differential diagnosis of 3-5 possible causes of the patient’s problem.
Discuss the most likely cause of the patient’s problem. Link the features of your patient’s history and physical that either support or argue against this diagnosis. It is rare that a disease on the differential is completely “ruled in” or “ruled out” based on the H&P. Use terms like “most likely because” or “very unlikely given” rather than the more definitive “rules in” or “rules out”.
Next discuss the other 2-4 other diagnoses you are considering (based on your branching diagram or matrix). Again, link the features of your patient’s history and physical either support or make each diagnosis less likely
Format for an exacerbation of a chronic problem:
Your assessment would address the most likely reasons for the exacerbation, as suggested by your patient’s history and exam findings.
Plan
| Plan | Include in Term 2 Spring Quarter & Term 3 writeups |
Purpose: To outline your next steps in addressing your patient’s clinical problem(s).
Format: The plan is usually presented as a bulleted list, and may include interventions in these categories:
| Diagnostic Plan | Lab tests | |
| Imaging | ||
| Consultation with specialists | ||
| Treatment (Therapeutic Plan) | Behavior change | |
| Medications | ||
| Counseling | ||
| Referral to another provider (e.g. physical therapy) | ||
| Monitoring and follow-up | Repeat laboratory tests to monitor response to treatment | |
| Routine screening tests | ||
| Primary care clinic follow-up | ||
| Education | Education about diagnoses done by you | |
| Referral to other providers for additional teaching, e.g. diabetes educator, pharmacist | ||
Common Problems with FCM Write-ups
If your patient has a known diagnosis and is admitted for routine therapy
If your patient has a known diagnosis with no new symptoms, for example a patient with cancer admitted for chemotherapy, there is still much you can learn from an interview and write-up. In your write-up, you can approach the case as a new referral – you are documenting the details of their illness even though the diagnosis is already known. Report on the initial presentation and progression of the illness, how it was diagnosed, treatment to date, the impact on patient and family, and what your patient is hoping for.
If two equally important problems were responsible for hospital admission
You can take either of two approaches
- combine the two problems in the HPI and record all symptoms chronologically OR
- separate the two problems in the HPI, first providing a complete history for the first problem and then a complete history of the second.
The chronology is unclear
Approach the patient from the standpoint of their history at the time of admission, when they presented for care. Your history is then presented in a chronology organized on the basis of time “prior to admission” (PTA). You should describe all events using consistent time points, like hours/days/months/years prior to admission.
The physical exam shows up in the HPI
Do not put physical exam findings from your examination into the history portion of the database, or historical information into the write up of the physical exam.
Nonstandard abbreviations are used
Many abbreviations are used differently in different specialties. In addition, abbreviations are often overused – – “the pt is STH prbm c SOB…” translates to “the patient is said to have a problem with shortness of breath” and is inferior to “the patient became dyspneic…”. When in doubt, spell out the word. Unfamiliar abbreviations will only bewilder your reader, and many are not allowed because of patient safety issues.
The Physical Exam and Review of Systems are mixed up
The ROS is part of the “subjective” portion of the medical database, along with the HPI and Past Medical History. This subjective information is given by the patient, or family or caregivers. The PE is part of the “objective” portion, reflecting your own findings and observations. Next year, the ‘objective’ section will also include labs and other testing, after the PE. Never mix the “subjective” and “objective” portions of the database
Recording a “diagnosis” instead of a “finding” in your physical examination
In the physical exam section, you should describe your findings in detail. Diagnoses should be reserved for your assessment and plan. Instead of writing “findings consistent with RLL pneumonia” you should write “Chest: symmetric excursion, non-tender to palpation; dullness to percussion right lower lung field; bronchial breath sounds with occasional mid-inspiration crackles right lower lung field on auscultation.”

