Trauma/Intimate Partner Violence and Trauma-informed Care
In this chapter and workshop, you’ll learn about the prevalence of intimate partner violence (IPV), how it affects our patients, and how this understanding should affect our approach to providing care. Many people are affected by abuse and its long-term impact on survivors. In addition to screening for violence, we suggest a “universal precautions” approach to caring for patients and providing resources.
A note about gender in this session: IPV is experienced and perpetrated by people of all genders, although frequency and impact may be different. Most available research has been done with survivors who identify as female, without differentiation of cis/trans. Therefore, much of the information in this module is about the female experience. We should insist ongoing research include inquiry into the experiences of people of all genders.
The preparatory Pressbook include:
- Trauma across the lifespan & trauma-informed care (TIC)
- Intimate Partner Violence (IPV)
- Child abuse
- Elder mistreatment
Trauma across the lifespan and trauma-informed care
Trauma across the lifespan can affect the way that survivors access and experience healthcare. If trauma is not considered, interactions with the healthcare system have the potential to be re-traumatizing. Affected patients may engage less effectively with clinicians and may be less able to follow through with treatment plans, and serious illness can be overlooked or undertreated.
To begin your study of this critical topic, please view this 22 minute presentation by Dr. Addie McClintock.
Trauma Informed Care
You were introduced to the concept of Trauma Informed Care (TIC) in the chapter on Introduction to the Physical exam. As we learned, over half of people have experienced some type of trauma, such as emotional, physical or sexual abuse or violence in their home or community.
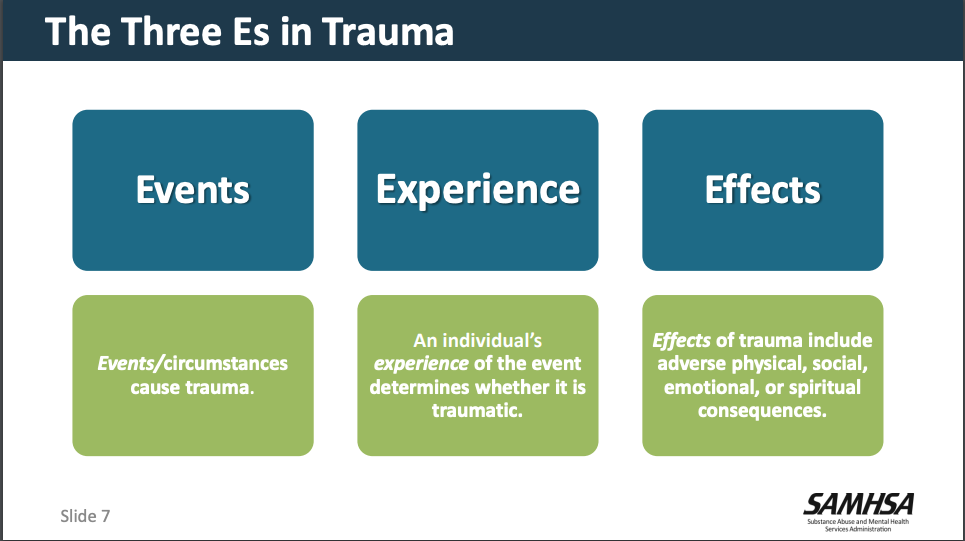
We learned from the video about the three E’s of trauma (Event, Experience, Effect) and how a patient’s experience of trauma can differ based on their own individual factors, environmental factors and the specifics of the event. We also learned about how trauma can impact health acutely and over time.

As doctors, it is important to not make assumptions about whether someone may have experienced trauma in their lives or not. Instead, we should approach all encounters from a trauma informed perspective. There may be, however, some clues of possible trauma in adults such as the following: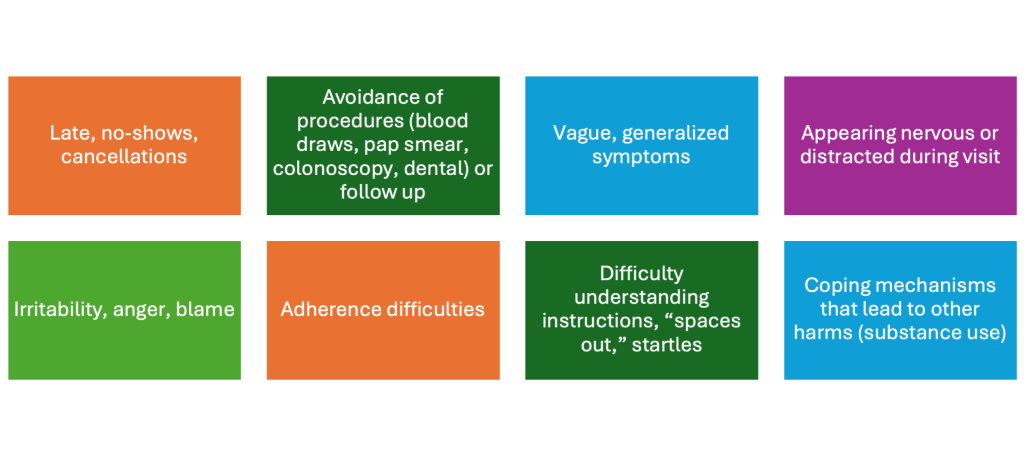
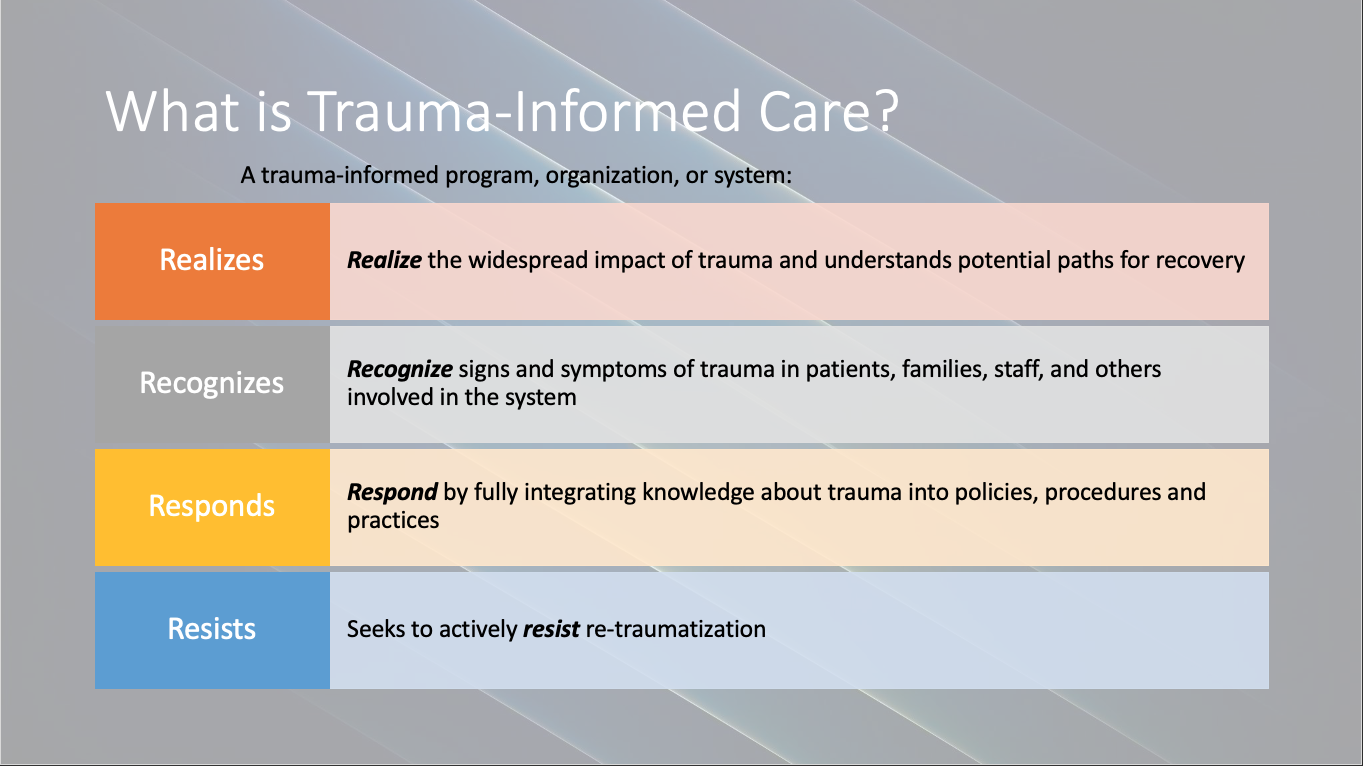
Later in this chapter you will learn more about how trauma may further impact individuals taking into consideration intersections of identity. For now, we will dive deeper into the concept of Trauma-Informed Care (TIC). The primary goal is to engage with people in a way that minimizes the risk of re-traumatization. The 4-Rs approach (developed by SAMHSA) provides a scaffolding for TIC.
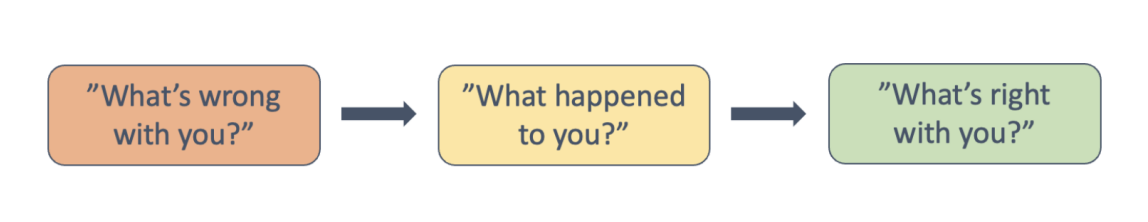
As discussed during the video our goal is to change our perspective when caring for patients in the following way:
To achieve this goal the Substance Abuse and Mental Health Services Administration (SAMHSA) proposes 6 principles of TIC. These principles need to be applied at both an organizational and clinical level. This chapter will focus on Safety and Trustworthiness and Transparency from a clinical perspective.
Six Principles of Trauma-Informed Care
- Safety
- Trustworthiness and Transparency
- Peer Support
- Collaboration and Mutuality
- Empowerment, Voice and Choice
- Cultural, Historical, and Gender Issues
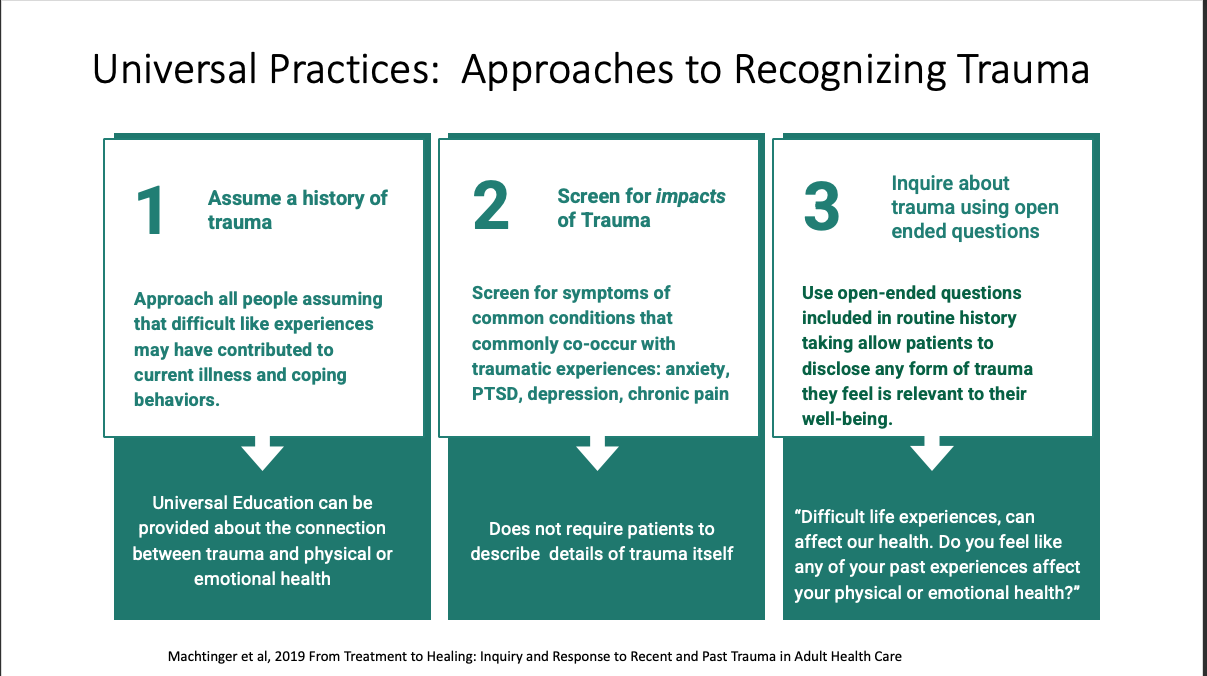
Trauma informed care requires the use of Universal Practices with all patients and Trauma-specific services when trauma or violence is identified. The following provides a trauma informed approach to all encounters. Later in this chapter you will learn more about screening specifically for intimate partner violence and responding to disclosures of violence.
Clinical encounters and physical exams can be especially difficult for patients with trauma. The following are potential triggers for retraumatization in health care settings:
- Being alone with a new clinician
- Invasive questions, exams, procedures
- Removal of clothing
- Vulnerable exam/procedure position
- Being physically touched
- Being unconscious
- Gender of clinician
- Repetitive interviews and exams
When asked, patients have shared ways in which the physical exam impacted them.
The best practice is to apply trauma informed principles every time you take a history and perform a physical exam. It is important to explain what you are doing and why and return control and bodily autonomy to your patients. For additional information, review the Introduction to the Physical Exam chapter on Trauma Informed Care (TIC) for additional tips.
Trauma Informed Care During the History
- Create inclusive environments
- Practice cultural humility
- Ask patients what can be done to make them feel more comfortable (e.g. do they want a support person with them, do they need a blanket to keep warm or cover up, etc)
- Honor personal space
- Be aware of your body language and positioning
- Ask about keeping door open or closed
- Provide notice of changes or delays in care
Trauma Informed Care During the Exam
- Attend to draping and modesty
- Introduce exam components
- Explain what you are doing and why
- Ask permission before touching the patient or moving clothing
- Stay within eyesight
- Respect personal space
- Use simple, clinical language
- Check in
- Use professional touch and language
- Be efficient
The most important thing is for us to be transparent in our words and actions and work to develop trust.
Ways to promote trustworthiness and transparency
- Be open and honest
- Be reliable and consistent
- Be authentic and empathic
- Provide clear and accurate information
- Give patients as much control as possible
- Narrate tasks and procedures
- Make eye contact
- Be clear about when confidentiality can and cannot be maintained
- Maintain appropriate boundaries
The goal is for the development of an open and honest relationship between the clinician and the patient. It takes time to learn these skills and we will all make mistakes. When mistakes happen, acknowledge and apologize and be open to growing and practicing your TIC skills.
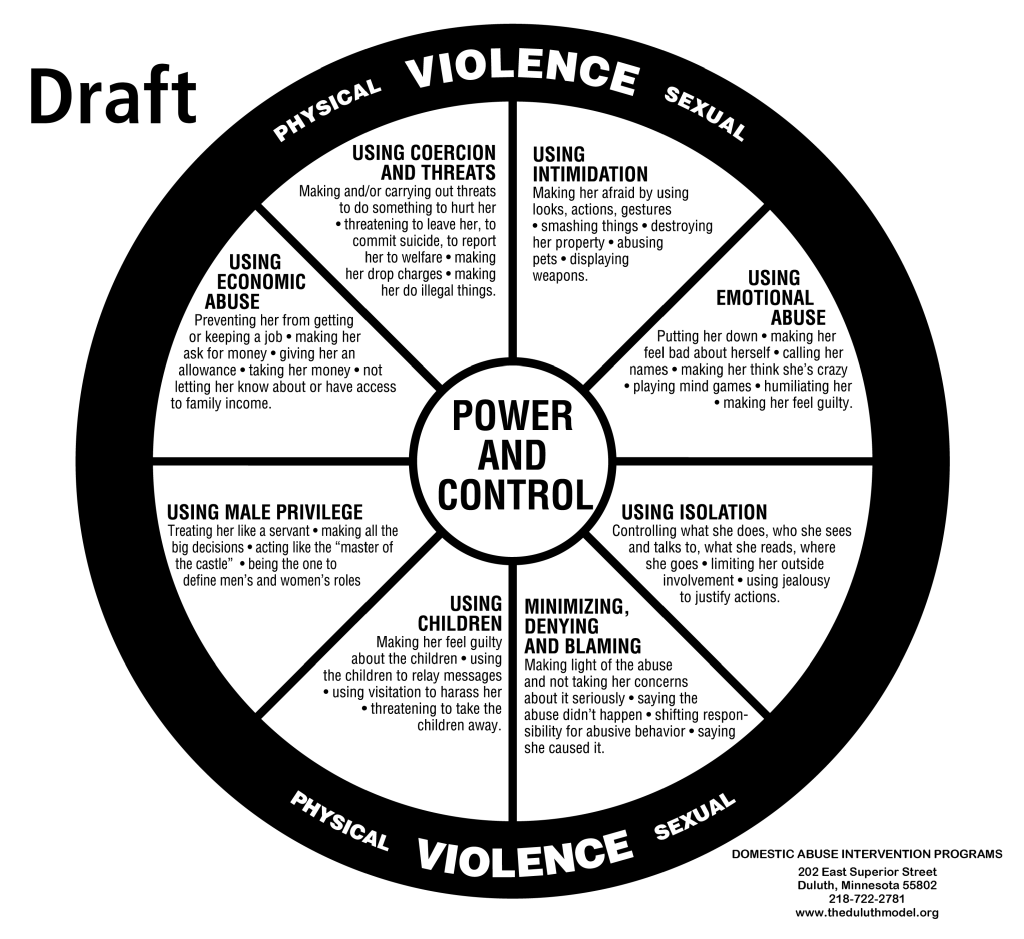
Intimate Partner Violence
Intimate partner violence (IPV) is the use of physical, sexual, economic, or emotional abuse by one person in an intimate relationship to establish and maintain power and control over the other. It includes physical violence, sexual violence, stalking, and psychological aggression by a current or former intimate partner.
If the information in this module raises concerns about your own relationships or those of a loved one:
- Stop and take care of yourself first
- Connect with your medical school counselors
- Explore information about relationships and safety at www.myplanapp.org
- Access University of Washington resources at UW SAFE Campus
- National Domestic Violence Hotline thehotline.org or 800-799-SAFE
- NW Network of Bisexual, Lesbian, Gay and Trans Survivors of Abuse The NW Network
Optional Additional Content
- To learn more about the above illustration, check out https://www.theduluthmodel.org/wheels/faqs-about-the-wheels/ Or go to https://www.theduluthmodel.org/wheel-gallery/ and see how different communities and cultures have adapted the Power and Control Wheel to represent the experience of victims. All wheels approved by DAIP must gather the content through focus groups with those who experience the ongoing tactics of abuse.
- To learn more about resistive violence, visit the Turning Points website at https://dvturningpoints.com/about/
- To explore a national resource library on gender based violence, see https://vawnet.org/
IPV and other types of family violence are forms of Sexual and Gender-Based Violence (SGBV). The United Nations High Commission on Refugees SGBV as any act that is perpetrated against a person’s will and is based on gender norms and unequal power relationships.
- Pre-birth: sex-selective practices, effects of battering during pregnancy on birth outcomes and on maternal bonding
- Childhood: exposure to IPV in family, female infanticide, child marriage, female genital mutilation, physical/sexual/psychological abuse, incest, child prostitution, and child pornography
- Adolescence and adulthood: dating violence, economically coerced sex, sexual harassment, sexual assault, reproductive coercion, trafficking, elder abuse.
Epidemiology of IPV
Intimate partner violence affects one-third of Americans during their lifetime. Nearly half of murdered women were killed by a current or former intimate partner, and serious physical injury affects many IPV survivors. Survivors are more likely to have chronic health conditions, including depression, anxiety, suicidality, GI disorders, chronic pain, and substance use disorders.
The CDCs ongoing National Intimate Partner and Sexual Violence Survey (NIPSVS) reports that 38% of women and 31% of men have experienced sexual violence, physical violence or stalking by a current or former partner. 61% percent of bisexual women, 44% of lesbian women, and 35% of heterosexual women report rape, physical violence, or stalking by an intimate partner at some point in their life.
The NIPSVS is a large phone survey that relies on self-report of demographic variables, and data on gender is reported in binary categories only. Smaller studies have demonstrated that IPV is common in transgender and gender non-conforming patients and may be even more common in those populations than in cisgender patients. Most available research has been done with survivors who identify as women – our hope is that future research will include inquiry into the experiences of people of all genders. Given the prevalence of sexual and gender-based violence including IPV, and relatively low rates of disclosure to providers, a trauma-informed approach to all patient encounters is recommended.
One of the biggest differences in how men and women experience IPV is in fear and consequences. Women are far more likely to report being fearful of intimate partners and are almost four times as likely to be injured by their partners. Impacts of violence may be more significant in otherwise marginalized populations, and experiencing violence exerts negative socioeconomic pressure on survivors and their families. Be aware of your own biases and stereotypes as you consider when and how to screen for and address these issues with your patients.
Screening Recommendations
Because primary care-based interventions for women of childbearing age have been shown to reduce the risk of subsequent violence, the US Preventive Services Task Force recommends screening in this population. Reliable data is not available for other populations or settings. You are likely to see electronic and/or in person screening in your PCP.
Research shows that people who talk to their providers about IPV are four times as likely to access an intervention, like a hotline or shelter, as those who talk to family members or friends. It also shows that women are receptive to IPV assessments. They are best received when:
- there is not a push for disclosure
- the question is tied to education about the impacts of trauma on health and wellness
- providers listen well and are non-judgmental
Screening should only occur if privacy can be assured, an appropriate interpreter is available, and there is ability to respond to a disclosure. Often, disclosure comes after being asked over several visits.
CUES Approach to Screening
Pairing screening with brief education ensures that patients receive valuable information whether they choose to disclose or not. Studies show survivors are most likely to discuss relationship concerns with a friend. Empowering our patients with information therefore also helps protect communities. This approach is called “Universal Education.” In primary care, this can be a patient-centered and trauma-informed approach to educating and supporting all patients.
C: CONFIDENTIALITY
UE: UNIVERSAL EDUCATION + EMPOWERMENT
S: SCREEN AND SUPPORT
CUES: Confidentiality
To ensure privacy, you may want to practice using phrases like “We see all patients alone for part of the visit” or “I’ll show you to the waiting room while we do the exam, then we’ll call you back when we are done.”
You should only screen when an appropriate interpreter is available, and never with kids over age three present.
Disclose the limits of confidentiality, based on your state’s mandatory reporting requirements for IPV. In general, physicians are not legally mandated to report most cases of IPV, with some exceptions for life-threatening or firearm-related injuries. Because they vary state-to-state, we will discuss local laws in class, and you should ask your preceptor about local requirements when rotating outside your home state. IPV is not itself grounds for a Child Protective Services referral.
CUES: Universal Education and Empowerment
As with any sensitive topic, start the conversation with framing and normalizing. Consider a phrase like “I’ve started discussing with all my patients the importance of healthy relationships and the impact of unhealthy ones.”
Here are some additional phrases you could try:
Universal education and empowerment can be facilitated by printed or electronic resources. See the links below for PDFs or to order cards for various populations. Each card reviews aspects of healthy relationships, red flags for unhealthy ones, and shares tips for safety planning and resources for support. The cards are customized for different settings and communities.
Make the connection by opening the card and quickly reviewing: “It talks about healthy and safe relationships…and how relationships affect your health.“
When cards are not available, mentioning or showing the myplanapp.org or thehotline.org can be a good substitute. New Beginnings is a local organization that provides general resources on domestic violence. The NW Network is a local organization with a focus on LGBTQ+ survivors of abuse.
Futures Without Violence Universal Education Cards
CUES: Screening
If you are in a private setting and you can provide referrals and support, you can screen with a question such as “has anything like this ever happened to you?”
If the answer is no, “I’m glad! If it does, or if you have questions, this is always a safe place to talk about it.”
Primary care practices often screen for IPV with an electronic questionnaire completed prior to the visit. Surveys show that many patients prefer this approach over direct questioning. If a patient’s presentation suggests the possibility of IPV, you can also ask direct questions such as:
- Are you ever afraid of your partner or an ex-partner?
- Within the past year, has your partner hit, kicked, choked, or hurt you?
- Has anybody forced you to do something sexual you didn’t want to do, or interfered with birth control?
- Do you feel safe at home, at work, and in your neighborhood?
- Do you think any past or current relationship stress could be affecting your health right now?
CUES: Example
In this video, the provider briefly reviews a negative electronic screen and shares information with two Universal Education cards that the patient can take with her. In this video, the provider discusses sharing resources with all women. We feel it would be appropriate to share these resources with all individuals regardless of gender identity or sexual orientation.
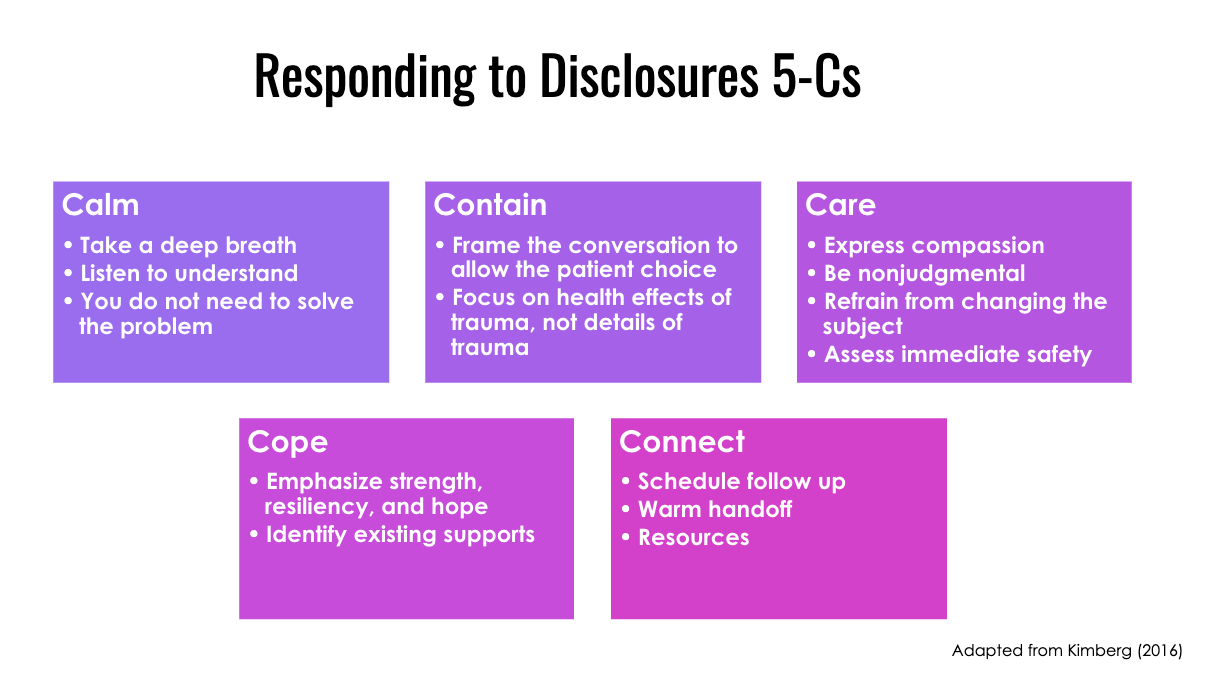
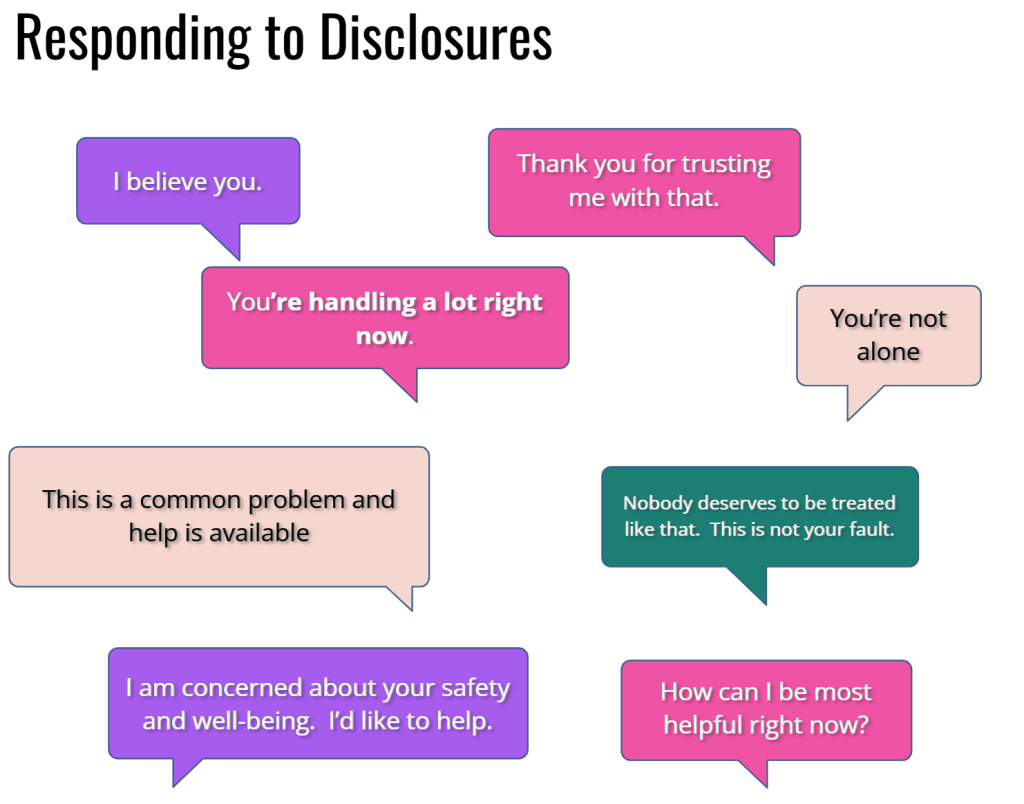
Responding to disclosure
Many of us feel unsure how to help if a patient discloses trauma. Remember that you do not need to elicit details to respond effectively. In fact, experts feel it is better not to ask too many questions, to avoid re-traumatization. You can positively impact patients by demonstrating compassion, setting the stage for referrals, emphasizing strengths, and building their autonomy.
Because of the dynamic of power and control in IPV, it is especially important that medical providers avoid inadvertently reproducing power dynamics within the visit, resisting the temptation to try to make medical or safety decisions for the survivor. In many cases, leaving a relationship is not the best choice for a survivor at this time.
As a student, you are well prepared to thank your patient for disclosing current or past trauma and to show your empathy and compassion. At that point, consider pulling your preceptor into the conversation, especially if the trauma is recent or your patient seems distressed – “I’d like to get my teacher to help us discuss this as safely and supportively as possible.”
The 5-Cs are a way to respond to disclosures of violence from your patients.
Assessing Safety
If a patient discloses IPV, immediate safety can be assessed by asking if they feel safe going home. If not, they need to be connected with their choice of resources immediately.
IPV survivors also have a substantially higher rate of suicidal thoughts and attempts, with as many as 23% having attempted suicide compared to 3 percent of those with no prior exposure to IPV. Suicidal ideation can be explored with a question like “Sometimes when people are handling so many things, they have thoughts that they’d be better off dead or killing themselves. Does that ever happen to you?”
The presence of a gun in the home substantially increases the lethality of IPV. Nearly two-thirds of women killed with guns were killed by their intimate partners, and abused women are 5x more likely to be killed if the abuser owns a firearm.
The presence of a gun also increases the risk of suicide. High-risk gun protection orders have been shown to reduce the risk of gun-related injury and death. Recognizing and addressing the presence of a firearm in such a high-risk situation has the potential to make a difference for your patients.
“Why don’t they leave?”
It can be tempting to tell a patient experiencing abuse to leave a relationship. And it is natural to feel frustrated when there isn’t a simple solution to a patients’ situation. Nonetheless, trusting patients to know what is best for themselves, and empowering them to act on that knowledge is much more helpful. Importantly, leaving is the most lethal time in an abusive relationship. Understanding that leaving may not be the safest or best solution to a complex situation can help relieve the pressure to counsel a patient to leave. Sometimes becoming “safer” – a type of harm reduction- is the best way to think about next steps. Making a safety plan, especially if it includes a plan to leave the relationship is best done with the support of a trained advocate. Know what resources exist in your clinical setting, as well as availability of hotlines and apps that can support you and your patients.
There are many reasons why a person may or may not leave an unhealthy relationship. Many times, relationships that include violence are also sources of love, support and other important resources. There can be fear of losing contact with children or community, as well as justified fear that violence might escalate.
The situation can be even more complex in marginalized communities, for example:
- Lack of culturally responsive support services
- Interpreters and culturally responsive services may be part of small communities
- Less access to housing, health services/quality, jobs, insurance, food, transportation may cause disrupted communities, forced choices
- Linguistically isolated (partner speaks English)
- Differential policing, prosecution and experience in carceral system
- More likely to have CPS involvement and children placed in foster care
- Threat that disclosing violence “reflects badly” on the community
- Leaving may mean loss of small community and natural supports
- Risk of deportation
If interested, the following optional resources discuss reasons for staying.
National Coalition Against Domestic Violence: Why do victims stay?
(Please be aware that the following video describes violent acts and may be upsetting)
Warm handoff
Given how complex this decision-making is, it is best to make a warm handoff to a trained provider whenever possible. A warm handoff significantly increases the chance of follow up. A trained provider has resources for specialized treatment that might be needed, experiencing navigating issues around mandated supporting, have up to date information on laws, resources and best practices that may have changed as well as access to legal, therapeutic, housing and financial resources that may be needed. Connecting to community resources also supports and nurtures resilience. Wraparound services may be available.
When possible, attempt the following:
- Access onsite resources when available. Introduce the patient to the appropriate provider to create an immediate connection.
- When onsite resources are not available ask the patient’s permission to contact a hotline or local agency. Offer to make the call together if that would be helpful, and encourage them to connect while they are still in clinic.
- Patients should only leave with printed materials if they feel it is safe to do so. Consider making a follow up appointment rather than sending home resources.
Examples of warm handoff language
I know a number we can call where they know a lot about helping people going through these kinds of things.
Would you like to call together, from here in the room?
You can tell them as much or as little as you want to, and we can hang up at any time. You’re in control.
Hello, this is doctor… I’m here with a patient who might be interested in talking with someone. Could you tell us what to expect, and what you can offer?
Intersection of Identity, Circumstance and IPV
IPV cuts across all lines, but structural determinants of equity and health increase the risk for some individuals. In this section, we consider how intersecting identities and marginalization contribute to patients’ risk for and experience of IPV. Some issues faced by patients with marginalized identities include lack of culturally responsive support services, less access to resources, language barriers, reluctance to involve the carceral system, and reluctance to lose a small community. It’s important to remember that communities may also have special sources of resilience- such as elders, culturally responsive services, mutual aid groups, and spiritual practices.
Native Women
Murder is the third leading cause of death for native women, making them 10x more likely to be murdered than white women. Of 158 native women surveyed by Urban Indian Health Institute in Seattle, 94% reported a history of sexual assault or rape. A significant amount of violence against native women is perpetrated by non-native assailants. There is a growing awareness of the number of missing and murdered indigenous women and girls (MMIWG) whose cases are often not well documented or prosecuted, for a variety of intersecting reasons. This optional video (6 min) from the National Indigenous Women’s Resource Center (niwrc.org) describes the findings of a study on the prevalence of violence against American Indian and Alaska Native women and men, and briefly examines the impact of violence in that community.
Black Women
The Black Women’s Blueprint describes the sexual abuse to maternal mortality pipeline and explains the connection between childhood and adult trauma. The “weathering” of chronic threats superimposed on the accumulated stress from racism and sexism, compounded by the trauma perpetrated and triggered in healthcare, can impact the full reproductive life course of Black women. Understanding these connections and practicing trauma-informed, resilience enhancing, and culturally sensitive care can mitigate these risks for our patients.
“Adultification” and sexualization of Black girls and young women- sometimes called “misogynoir”- means they are more likely to be seen as provoking assaults and are more likely to experience retraumatization within carceral systems. Among people incarcerated in women’s prisons, past abuse — family violence, sexual violence, and/or domestic violence — is so prevalent, activists use the term “the abuse-to-prison pipeline.” Survivors may be reluctant to invite police and/or state agencies into their families and communities due to the increased risk of violence, incarceration, removal of children, and stigma.
LGBTQI and Anti-Trans Violence
61% of bisexual women have experienced rape, physical violence, and/or stalking by an intimate partner in their lifetime, and 64% of transgender individuals have experienced a sexual assault. There is an epidemic of violence against trans women- particularly Black trans women- that we are just beginning to understand. Fear of being “outed,” losing a chosen family, not being believed, or being retraumatized by healthcare and carceral systems can prevent survivors from seeking care.
People with Disabilities
People with disabilities tend to experience more severe intimate partner abuse for longer periods. They are more vulnerable to prolonged abuse because they are often isolated from community, reliant on abusers for care, and have less opportunity for direct interaction with support services. Women with disabilities are 40% more likely to experience domestic violence, while LGBTQ survivors with disabilities are at particular risk. IPV is also a cause of disability, as the leading cause of injury to women between the ages of 15 and 44.
Pregnancy and postpartum
IPV and reproductive coercion increase the likelihood of unplanned and undesired pregnancies. In addition, during pregnancy and the postpartum period, the frequency and impact of IPV increase, and options available to survivors may be more limited. IPV increases the risk of pregnancy complications, failure to thrive in infants, and postpartum mood disorders. The risk of homicide by IPV is higher in the pregnant and postpartum period.
Sex Workers, Trafficking and IPV
According to UNICEF, Human trafficking takes on a variety of forms and may intersect with domestic violence in multiple ways. For example, trafficking may occur at the hands of an intimate partner, family member, or another member of the household. Additionally, domestic violence at home may become a ‘push factor’ that causes someone to become vulnerable to trafficking. Almost 70% of adult female trafficking victims report experiencing domestic violence prior to being trafficked. Survivors may be reluctant to come forward if they are being trafficked by a loved one. People can be trafficked into any kind of work, including sex work.
Despite the Trafficking Victims Protection Act legislation, current law enforcement practices often result in the incarceration of sex trafficking survivors for crimes committed secondary to their having been trafficked.
It is important to remember that “Not all people who work in the commercial sex industry are trafficked. Some choose to do sex work, while others find sex work to be the best way of supporting themselves and their families, given their circumstances. Many sex workers work independently or in peer networks, without anyone exerting force or confiscating their money. Poverty, gender inequality, and lack of economically viable job options contribute to people entering into sex work.” Sex workers may be less likely to seek support from the police or the state due to increased risks of arrest or victimization within those systems. The downward socioeconomic pressure of IPV also leaves survivors with fewer traditional employment options.
Substance Use
There is a bidirectional interaction between IPV and substance use. Victimization by an intimate partner increases the risk of substance use by 6x. IPV rates among women accessing substance use disorder treatment range from 31-67% in the last year, up to 90% lifetime rates. IPV may be targeted at undermining recovery or promoting addiction.
Impairment from substances can limit a survivor’s ability to protect themselves or their children, to qualify for services such as housing, or to advocate effectively for themselves. They may encounter stigma or bias when seeking healthcare. It may also put them at risk of arrest or loss of custody if police become involved. IPV also significantly increases the risk of overdose from substances.
Key Takeaways
Intimate partner violence is common, affecting one third of Americans over the course of their lives.
Given the prevalence and infrequent disclosure to providers, use a trauma informed approach to all patient encounters.
CUES Universal Education is a patient-centered and trauma-informed approach to screening.
Because of the dynamic of power and control in IPV, it is especially important that medical providers avoid inadvertently reproducing power dynamics within the visit
In many cases, leaving a relationship is not the best choice for a survivor. A warm handoff to a trained nurse or social worker, a local domestic violence advocate, or a national hotline is usually the best approach to individualizing support for each patient.
Additional reading & references
SAMSHA’s Concept of Trauma and Guidance for a Trauma-Informed approach
UN Refugee Agency. Gender-based violence. UNHCR – Gender-based Violence
Intimate Partner Violence. NEJM, 2019. PDF or Online (NetID/login)
Trauma Informed Care. American Family Physician, 2017. PDF or Online
CDC Violence Prevention. Intimate Partner Violence
USDHHS. Violence against women with disabilities. Online.
Patient and community facing websites
National Domestic Violence Hotline thehotline.org or 800-799-SAFE
NW Network of Bisexual, Lesbian, Gay and Trans Survivors of Abuse The NW Network
My Plan. A free app to help with safety decisions for those experiencing abuse www.myplanapp.org
Extreme Risk Protection Orders. gunprotectionorder.org
National LGBTQ Institute on IPV https://lgbtqipv.org/
Recommendations for Screening
USPSTF 2018 screening recommendations Online
AHRQ. Intimate Partner Violence Screening. Healthier Pregnancy Fact Sheet. Online
Reproductive coercion
Miller E, Levenson R, Jordan B, Silverman JG. (2010). Reproductive coercion: connecting the dots between partner violence and unintended pregnancy. Contraception, 81(6):457-9.
Tiwari A, Leung W, Leung T, Humphreys J, Parker B, Ho P. (2005). A randomized controlled trial of empowerment training for Chinese abused pregnant women in Hong Kong. BJOG: an International Journal of Obstetrics and Gynecology, 1-10.
Video: Making the Connection- Reproductive Coercion
Strangulation and head injury in IPV
Video: Head Injury in Domestic Violence: (Trigger warning, explicit firsthand account of potentially lethal assault)
Resources for talking to patients: Has Your Head Been Hurt
Intersection of identity, circumstance and IPV
“Maze of Injustice, an Amnesty International report. Sexual Violence Against Indigenous Women in the USA” (Chapters 1,2, and 4 recommended)
Arrested Justice: Black Women, Violence, and America’s Prison Nation, by Beth E. Richie PhD.
Brief video explaining adultification bias and discussing the report “Girlhood Interrupted” by the Georgetown Law Center on Poverty and Inequity.
An article about misogynoir – a term coined by Moya Bailey at Northwestern University, to describe “the specific hatred, dislike, distrust, and prejudice directed toward Black women.” that leads to black women being shunned, disbelieved and punished when reporting crimes against them
Breiding MJ and Armour BS. The association between disability and intimate partner violence in the United States. Ann Epidemiol. 2015, June.
Child Abuse
Child abuse is defined as any abuse or neglect of a child under 18 by a parent, caregiver, or another person in a custodial role (such as a religious leader, coach, or teacher) that results in harm, potential for harm, or threat of harm. It includes:
- Physical Abuse
- Sexual Abuse
- Emotional Abuse
- Neglect
Child abuse is common, affecting an estimated 700,000 to 1.25 million US children annually. It is the 3rd leading cause of death in children between one and four years of age, and almost 20% of child homicide victims have contact with a healthcare professional within a month of their death. Pediatricians and family physicians are positioned to detect possible child maltreatment, but clinicians may miss physical or psychological abuse injuries at first presentation. It is important to be vigilant for potential abuse while recognizing the potential for bias and errors.
Determining whether a child is being abused is complicated and requires a thoughtful and often multi-disciplinary approach to evaluation. If abuse is suspected, further history about possible abuse should be obtained by a provider with expertise.
Physical findings that suggest possible abuse
Bruising is the most common and most visible sign of physical abuse. It may be the only sign of injury or signal of internal injury. Unfortunately, bruising is missed in up to 44% of fatal or near fatal cases. Children that are not yet mobile should not have falls or other injuries that cause bruising – remember that “those that don’t cruise, rarely bruise.” A bruise in any child under 4 months of age is concerning.
The TEN-4-FACES Bruising Clinical Decision Rule was developed and validated at the University of Chicago. It is intended to be used as a screening tool to improve the recognition of potentially abused children who require further evaluation.

Mandated reporting of suspected abuse
Health care workers, teachers, social workers, counselors, child care providers and law enforcement officers are designated as mandatory reporters, meaning that they are legally required to report suspected abuse to the appropriate state protective services agency. The law and process varies somewhat state-to-state. For more information on laws in your state as well as an overview of how the child welfare system works, visit the Child Welfare Information Gateway
If you are concerned about the possibility of abuse or neglect of a child, please reach out to your preceptors, your attending physicians in clinical years, or your mentors to discuss and to help you navigate the next steps. You’ll learn more about detecting and responding to child maltreatment and abuse in your Pediatric Clerkships.
Resources and references
University of Chicago Stanley Mann Children’s Research Institute. TEN-4-Faces-P. Online.
StatPearls. Child Abuse and Neglect. Online.
CDC Child Abuse and Neglect Prevention: https://www.cdc.gov/violenceprevention/childabuseandneglect/index.html
Child Care Health and Safety Violations: State and Territory Reporting Information: https://childcare.gov/Health-and-Safety-Reporting
Mandatory Reporters of Child Abuse and Neglect: https://www.childwelfare.gov/pubPDFs/manda.pdf
Cribsiders Podcast “Non Accidental Trauma”
Elder mistreatment
Background
Elder mistreatment (including neglect, abuse) has been reported in about 5 percent of the older adult population in the United States. Prior studies suggest that only one in 23 elder abuse cases are reported1. Perpetrators are typically family members, caregivers, and trusted others (such as neighbors, financial advisors). Almost 50% of older adults living with dementia experience elder mistreatment, and older women and socially isolated older adults are more likely to be victims of abuse2.
Types of Elder Abuse
There are many types of elder abuse as outlined in the table below. For additional information on elder abuse, consider reading the following American Family Physician article on “Detecting Elder Abuse and Neglect: Assessment and Intervention”
The tables included in this section are from that article.
| Table 1. Types of Elder Abuse | ||
|---|---|---|
| Types of abuse | Characteristics | Examples |
| Financial or material | Illegal or improper use of funds or resources, exploitation | Theft of debit or credit cards, coercion to deprive the older person of assets (e.g., forcible transfer of property or accounts) |
| Neglect or abandonment | Intentional or unintentional refusal or failure of designated caregiver to meet needs required for an older person’s well-being | Failure to provide adequate food, clothing, shelter, medical care, hygiene, or social stimulation/interaction |
| Physical | Infliction of pain or injury | Slapping, hitting, kicking, force-feeding, restraint, striking with objects |
| Psychological or emotional | Infliction of mental anguish | Verbal aggression or threat, threats of institutionalization, social isolation, humiliating or degrading statements |
| Sexual | Non-consensual genital contact, unwanted sexual talk | Suggestive talk, forced sexual activity, touching, fondling a non-consenting competent or incompetent person |
| Adapted with permission from Perel-Levin S. Discussing Screening for Elder Abuse at Primary Health Care Level. Geneva, Switzerland: World Health Organization; 2008:6. | ||
Signs and Symptoms of Elder Abuse or Neglect
Certain signs or symptoms may raise one’s suspicion of possible elder abuse or neglect. It is important to recognize that many diseases and conditions can mimic abuse or neglect in older individuals. Consequently, a thorough history, review of the medical records and physical exam is important. The Elder Abuse Suspicion Index (EASI) is a screening tool that can be used to screen cognitively intact older adults. When there is concern for abuse or neglect, interviewing patients and their caregivers separately can be helpful. It is important to not jump to conclusions that neglect or abuse is occurring, however, we don’t want to miss opportunities to intervene if it is.
| Table 3. Signs and Symptoms of Possible Elder Abuse or Neglect | |
|---|---|
| Bruising in unusual locations (not over bony Prominences; on lateral arms, face, or back; larger than 5 cm)Burns in patterns inconsistent with unintentional injury or with the explanation provided (e.g., stocking or glove pattern, suggesting forced immersion)
Decubitus ulcers, unless the result of unavoidable decline Dehydration, fecal impaction Evidence of sexual abuse Intraoral soft tissue injuries Malnutrition, medically unexplained weight loss Missing medications |
Patterned injuries such as hand slap or bite marks; ligature marks or scars around wrists, ankles, or neck suggesting inappropriate restraint.
Poor control of medical problems despite a reasonable medical plan and access to medication Subconjunctival or vitreous ophthalmic hemorrhage Traumatic alopecia or scalp swelling Unexplained fractures Unusual delay in seeking medical attention for injuries Urine burns (similar to severe diaper rash), dirty clothing, or other signs of inattention to hygiene |
| Information from reference 28 through 30. | |
Financial Abuse
Financial abuse is a common form of abuse that is not visible. Signs of financial abuse in older adults may include:
- Having a new ‘best friend’ or partner, particularly someone who causes isolation from family and friends
- Change in spending patterns
- Not paying bills or bills bouncing when they are typically paid on time
- An unexpected change in power of attorney or will
- Missing medical appointments when they typically seek medical care
Mandatory Reporting
As with children, physicians and medical students are mandated to report suspected abuse of any vulnerable adult. A vulnerable adult is defined as any person 60 years or older with functional, physical, or mental inability to care for self; or an adult age 18 years or older who:
- Has a developmental disability; or
- Has a guardian; or
- Lives in a nursing facility, boarding home, adult family home, or soldier’s home, residential habilitation center, or any facility licensed or required to be licensed by the Department of Social and Health Services (DSHS); or
- Receives in-home services through a licensed health care agency, hospice, or an individual provider; or
- Self-directs his/her own care (someone who chooses to direct another person, such as a caregiver, to perform care related tasks)
If you are concerned about the safety of a vulnerable adult in the hospital or clinic, talk with your attending physician. Contacting the team social worker is often the next step – they are skilled in assisting with mandatory reporting through Adult Protective Services (APS). While federal laws exist regarding elder abuse or neglect, it is important to recognize that laws regarding elder abuse or neglect can vary state by state.
Elder Abuse Suspicion Index (EASI) tool.
References
- Burnes D, Hancock DW, Eckenrode J, Lachs MS, Pillemer K. Estimated Incidence and Factors Associated With Risk of Elder Mistreatment in New York State. JAMA Netw Open. 2021;4(8):e2117758. doi:10.1001/jamanetworkopen.2021.17758
- Cooper C, Selwood A, Livingston, G. The prevalence of elder abuse and neglect: a systematic review. Age and Ageing. 2008;(151-160). https://doi.org/10.1093/ageing/afm194
