9 Functional Divisions of the Nervous System
Functional Divisions of the Nervous System
All of the hormones and endocrine systems discussed so far are subject to some degree of direct or indirect regulation by the nervous system, particularly the autonomic nervous system. Before discussing the neural regulation of endocrine systems, it is important to have a rudimentary understanding of the functional divisions of the nervous system itself.
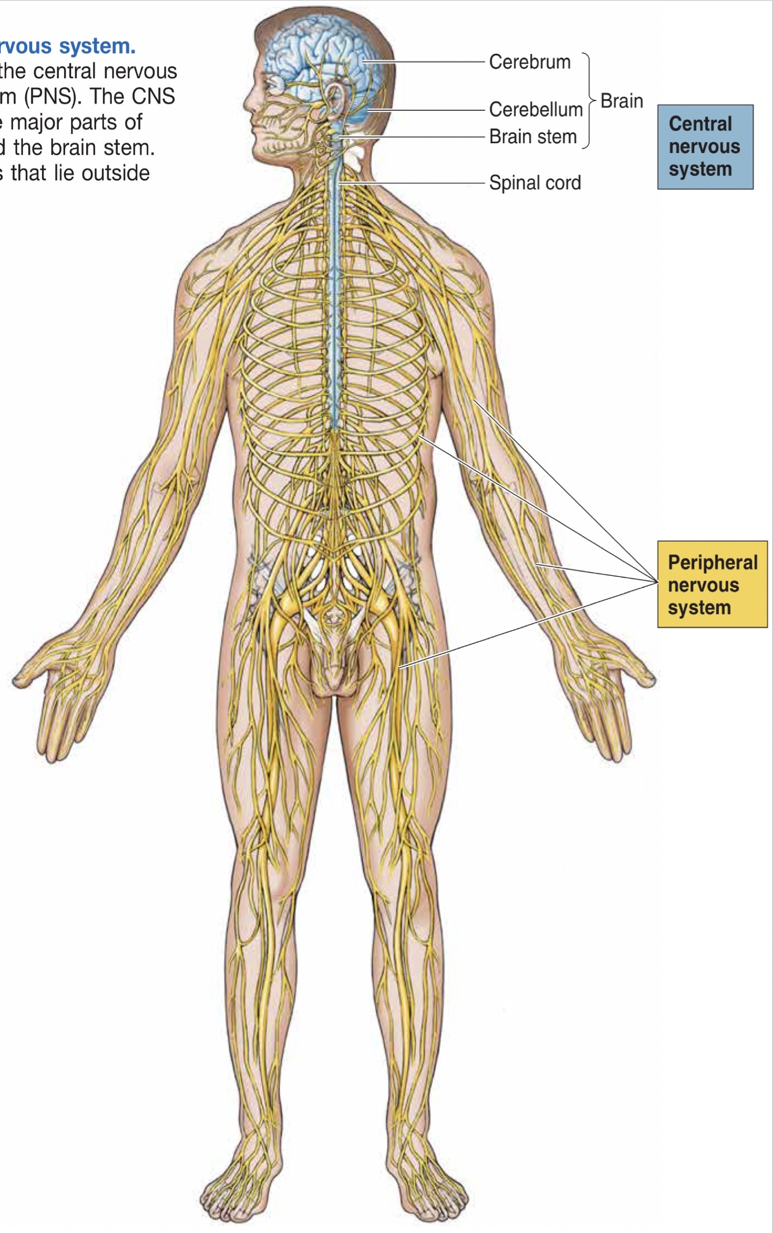
The nervous system provides control and communication throughout the body and is characterized by a constant struggle between excitation and inhibition. The Central Nervous System (or CNS) consists of neurons in the brain and spinal cord. The simplest processing of sensory information occurs in the spinal cord and becomes more sophisticated and complex in regions more rostral in the CNS (i.e., further up the spine and towards the frontal cortex). The tissue composing the CNS can be classified based on its appearance. Gray matter (grey matter) within the CNS exhibits a “gray” appearance due to the dense concentrations of cell bodies and dendritic extensions, whereas white matter is composed of collections of axons that have a lighter color due to the lipid-based myelin encasing them.
The peripheral nervous system (PNS) contains neurons outside of the brain and spinal cord and consists of the somatic nervous system (SNS), the autonomic nervous system (ANS), and the enteric nervous system (ENS). While CNS neurons cannot be regenerated if damaged, neurons of the PNS can recover, though they often fail to re-form connections made prior to damage.
The somatic nervous system, under conscious control, contains sensory neurons bringing information to the CNS, and motor neurons carrying commands from the CNS. The ANS controls almost every other tissue in the body, including cardiac muscles, smooth muscles, organs, etc.
The ANS is an extensive neural network operating without voluntary, conscious control. It is divided into two opposing systems that continually monitor and antagonistically control physiological systems. The two components of the autonomic nervous system are the sympathetic nervous system (SNS) and the parasympathetic nervous system (PSNS). Very generally, the SNS is engaged during times of increased distress or danger, while the PSNS operates while the body is at rest. In other words, the SNS is involved in fight-or-flight responses, whereas the PSNS is involved in rest-and-digestion. It may be helpful to think of the sympathetic response as being engaged when jumping out of a plane, and the parasympathetic response engaging after opening a parachute. In the nervous system, a collection of cell bodies performing the same function (or similar functions) is called a nucleus or ganglion. Both the SNS and PSNS originate from collections of cell bodies called the autonomic ganglia.
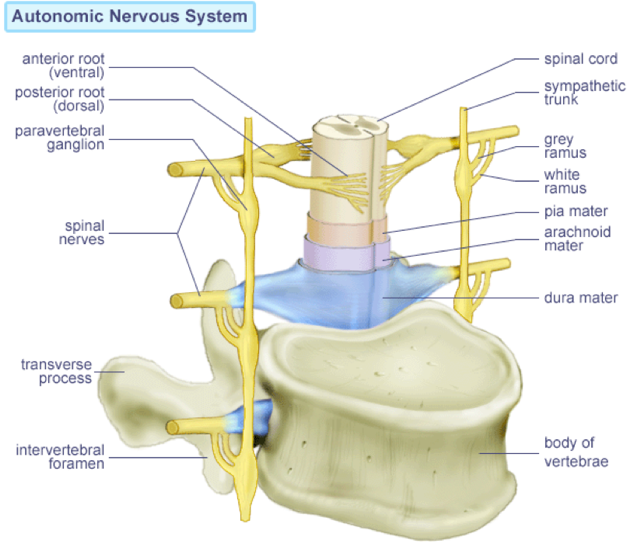
Within the PNS, individual neurons project between the spine and their targets. As the body grows, the axons grow in length to accommodate the longer distance information must be carried. The PNS carries sensory information back towards the CNS so that it can be processed, and an appropriate response can be generated. The most basic pathway, then, starts with a peripheral process from a sensory neuron, which carries an afferent transmission from sensory dendrites towards the spinal cord. The cell body of a sensory neuron is located in a dorsal root ganglion (i.e., in a dorsal root of the spinal cord). From the dorsal root ganglion, the central process axon projects to interneurons (association neurons) in the CNS, which processes the sensory signal before contacting a motor neuron, leading to an efferent transmission. The efferent transmission can be mediated by either the SNS or the ANS. In the SNS, the motor neuron has a cell body in the ventral root of the spinal cord (within the CNS), and projects out of the CNS towards effector muscles and/or glands. This pathway, in which a sensory signal leads to a motor response, is a circuit.
Unlike somatic nervous system cell bodies, the autonomic ganglia reside outside of the CNS. Thus, there is a disynaptic pathway between the CNS and target structures of the ANS. This is in contrast to the somatic nervous system, in which neurons from within the CNS can communicate with their targets through a single synapse, the neuromuscular junction. In the ANS, pre-ganglionic fibers carry information from the brain to the autonomic ganglia. These neurons in the autonomic ganglia project post-ganglionic fibers to three types of targets throughout the body. Firstly, post-ganglionic fibers innervate numerous glands, including saliva-, sweat-, tear-, and mucous-producing glands. They also regulate the metabolic functions of the liver, gastrointestinal tract, pancreas, kidneys, and reproductive organs. While the pancreas and kidneys have traditionally been regarded as functioning autonomously, it is now understood that both are innervated, and their operation is subject to modulation. Secondly, post-ganglionic fibers innervate smooth muscles, endowing their abilities to regulate blood flow via dilation/constriction of blood vessels, to modulate air passage into the lungs via control of smooth muscle-lined bronchi, to adjust gastrointestinal motility, and to initiate expulsion of urine from the bladder and feces from the rectum. Lastly, post-ganglionic fibers also regulate the cardiovascular system through innervation of cardiac muscles and blood vessels.
 The SNS and PSNS are largely independent from one another. Though they do not directly affect each other’s functioning, they will respond to the internal conditions caused by each other.
The SNS and PSNS are largely independent from one another. Though they do not directly affect each other’s functioning, they will respond to the internal conditions caused by each other.
The SNS is activated by any of the four F’s: fight, flight, fright, or floozying (sex). Sympathetic activation, the so-called fight-or-flight response, generates short-term emergency responses at the expense of long-term health, such as increased cardiac output, the shunting of blood towards skeletal muscles, increased pulmonary respiration, mobilization of glucose reserves, as well as suppression of digestion, suppression of reproductive physiological systems, and suppression of immune functioning. Pre-ganglionic neurons in the SNS are cholinergic (ACh-producing) and are located in the intermediolateral gray matter of the spinal cord. They project from thoracic and lumbar regions to the sympathetic ganglia. The sympathetic ganglia on each side of the body are organized into a chain running parallel the length of the spinal cord and fusing together at the coccyx. These post-ganglionic neurons have nicotinic ACh receptors (ionophores), permitting rapid excitation by cholinergic pre-ganglionic fibers. Other sympathetic ganglia, called collateral ganglia, are not part of the sympathetic chain, but rather are located in the abdominal cavity. The post-ganglionic fibers in the sympathetic chain control tissues in the chest and head (e.g., pupil dilation, salivation, pulmonary respiration, vasodilation/constriction, cardiac output), whereas those in the collateral ganglia target organs in the abdominal cavity. One exception to these trends is the adrenal gland, which receives direct innervation from pre-ganglionic neurons, meaning that the release of NE and epinephrine from the adrenal medulla is actually initiated by ACh. Nevertheless, post-ganglionic sympathetic fibers are almost exclusively noradrenergic, using norepinephrine as their signal molecule. Aside from the unique monosynaptic cholinergic innervation of the adrenal gland, post-ganglionic neurons targeting sweat glands and blood vessels in skeletal muscles violate the general rules and use ACh as their signal molecule.
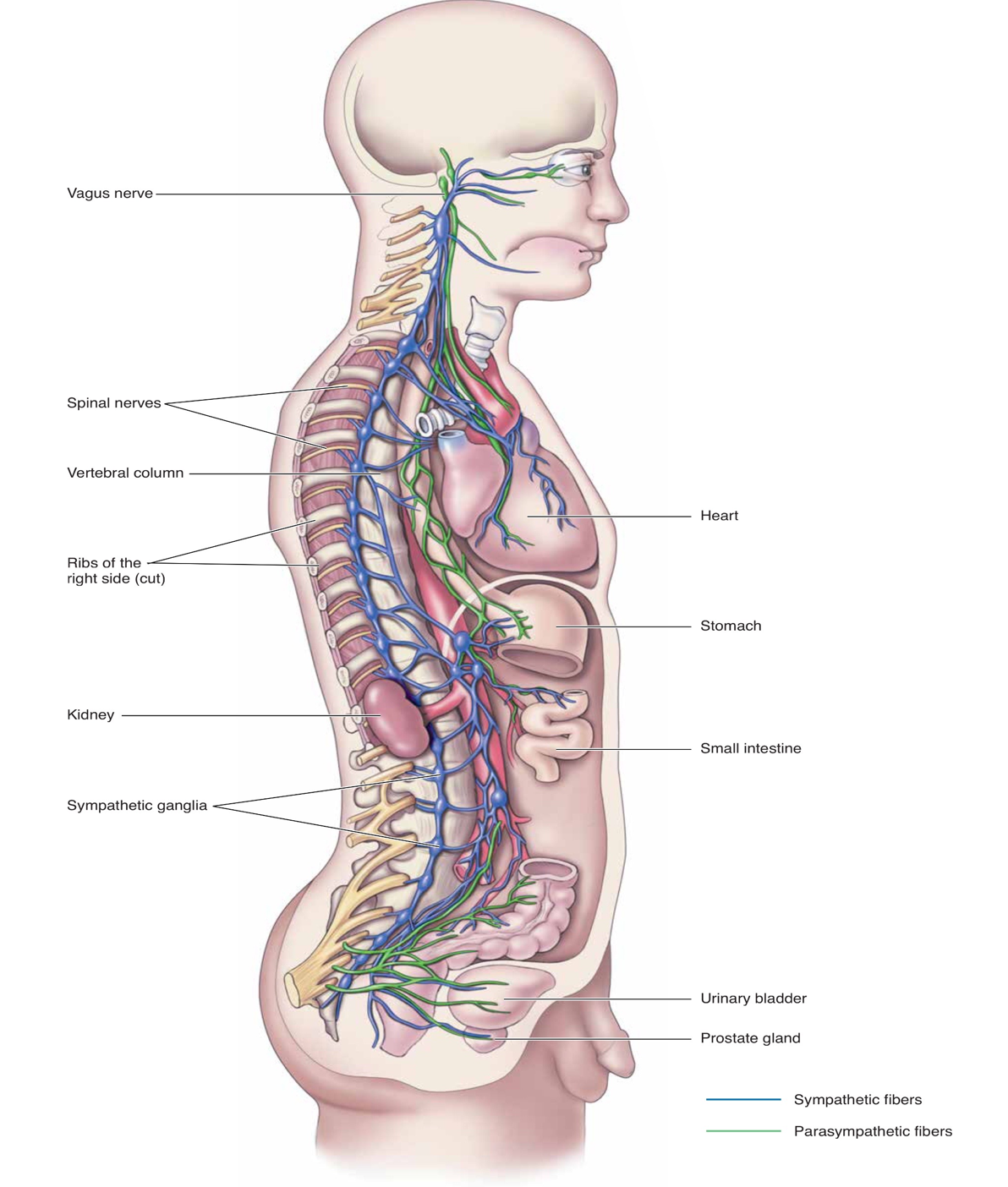 Vagus NerveSpinal NervesVertebral ColumnRibs of the Right SideKidneySympathetic GangliaHeartStomachSmall IntestineProstate GlandBladderSympathetic Parasympathetic
Vagus NerveSpinal NervesVertebral ColumnRibs of the Right SideKidneySympathetic GangliaHeartStomachSmall IntestineProstate GlandBladderSympathetic Parasympathetic
The PSNS facilitates the four non-F’s: digestion, growth, immune response, and energy storage. Thus, activation of the PSNS is often simply denoted as a rest-and-digest response, in which blood pressure and heart rate are low, and the body has time to recover and repair. These actions of the PSNS support long-term health. Like the SNS, pre-ganglionic neurons of the PSNS are cholinergic (i.e., all pre-ganglionic ANS neurons are cholinergic). However, unlike the SNS, PSNS pre-ganglionic neurons reside in the brain stem and the sacral portion of the spinal cord. In contrast to the organized ganglia of the SNS in the sympathetic chain, the parasympathetic ganglia are located adjacent to their target tissues. Furthermore, all PSNS post-ganglionic fibers are cholinergic.
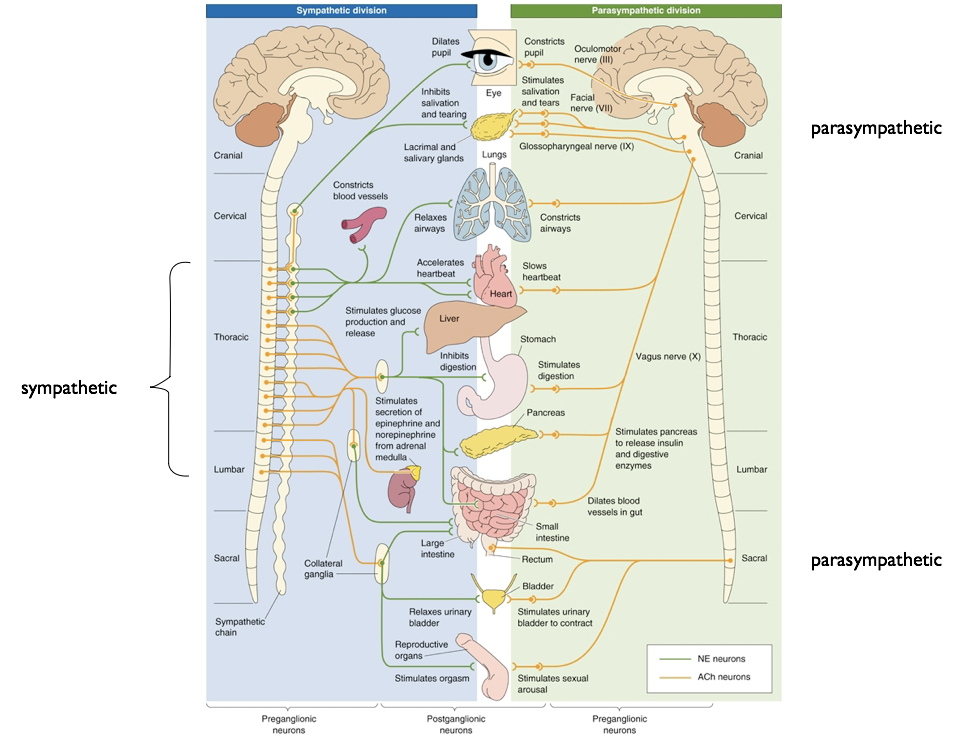
In general, the SNS and PSNS have antagonistic actions, and relative levels of activity tend to be somewhat inversely correlated such that high activity in one system necessarily entails low activity of the other. However, the SNS and PSNS are not perfectly symmetrical. Blood vessels in the skin, sweat glands, adrenal glands, and certain cardiac functions are regulated exclusively by the SNS. This asymmetry in adrenal innervation is of particular importance because the PSNS has no way of directly reversing the secretion of epinephrine and adrenaline. In contrast, tear-producing glands only receive PSNS innervation. Furthermore, the two systems are not always antagonistic. For example, a successful male sexual response requires sustained parasympathetic activity to enable erection, but necessitates SNS activity for orgasm and ejaculation.
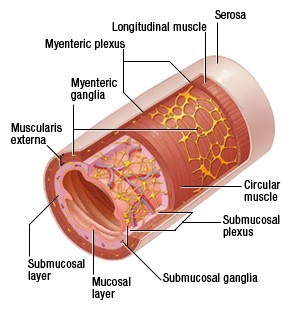
The last division of the PNS, and arguably a component of the ANS, is the enteric nervous system (ENS). It is composed of neurons contacting the entire gastrointestinal (GI) tract, from esophagus to anus, as well as the pancreas and gallbladder. While it receives indirect input from the SNS and PSNS, it operates with relative autonomy in its control of various digestive processes. The ENS is composed of two neural networks with sensory, inter-, and motor neurons, the ganglia of which lie in distinct layers around the length of the digestive tract. Ganglia of the submucosal (Meissner’s) plexus reside close to the intestinal lumen within the submucosal. Myenteric (Aurback’s) plexus ganglia reside in the muscularis externa, further from the lumen of the gastrointestinal tract. Sensory cells in the submucosal plexus regulate excretion into the lumen and communicate with the myenteric plexus, which in turn is capable of regulating secretion and excretion by adjacent endocrine organs.
Together, these plexes regulate numerous aspects of digestion. The ENS monitors tension and stretch of intestinal walls, chemicals in the gastrointestinal tract, as well as the presence of blood-borne hormones. Independent of control by the CNS, SNS, or PSNS, the ENS is able to integrate these chemical and mechanical signals to appropriately regulate peristalsis, production of mucous, excretio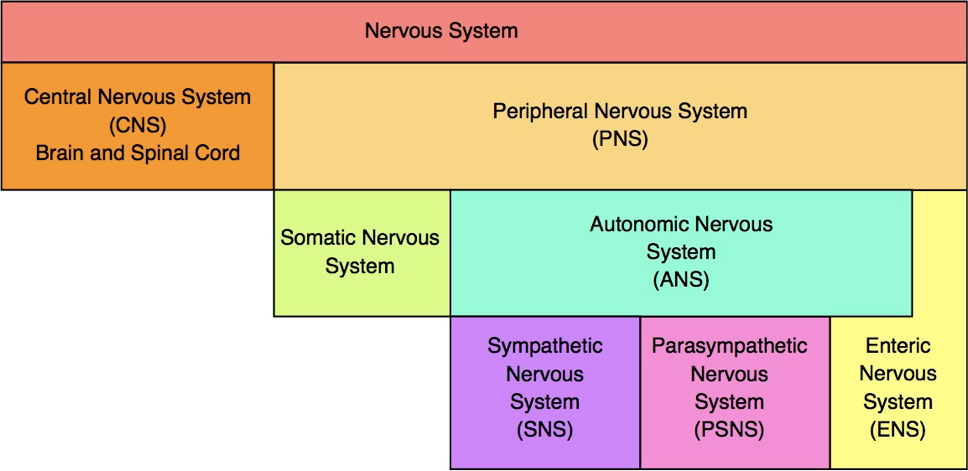 n of digestive enzymes into the gastrointestinal tract, and the dilation of local blood vessels. Most interestingly, the ENS has bidirectional communication with the intestinal flora, and alters gut motility and secretion in response. The ENS also provides a substrate by which microbiota of the gut can influence CNS functioning, including higher-order cognition and emotion. Despite the fact that the ENS contains as many neurons as the entire spinal cord (about 500 million), research has only recently begun to examine its diverse roles.
n of digestive enzymes into the gastrointestinal tract, and the dilation of local blood vessels. Most interestingly, the ENS has bidirectional communication with the intestinal flora, and alters gut motility and secretion in response. The ENS also provides a substrate by which microbiota of the gut can influence CNS functioning, including higher-order cognition and emotion. Despite the fact that the ENS contains as many neurons as the entire spinal cord (about 500 million), research has only recently begun to examine its diverse roles.

Feedback/Errata