3 Lab Week 3: Spinal Cord and Brainstem
Learning Objectives
Spinal Cord and Spinal Nerves
1. Describe the gross anatomy of the spinal cord and the spinal nerve.
Identify the dorsal and ventral roots, dorsal root ganglion, cervical and lumbar enlargements, central canal, conus medullaris, cauda equina, ventral (anterior) median fissure, meningeal layers and their specializations (filum terminale and denticulate ligament).
Define the lower limit of the spinal cord, and explain why a spinal tap (lumbar puncture) is usually done below the vertebral level of L3.
Distinguish between spinal and epidural anesthesia.
2. Describe the internal structure of the spinal cord.
Draw a cross-sectional view of a typical spinal cord segment and nerve, and include in the diagram a motor neuron and a sensory neuron.
Identify the pattern of white and gray matter in each region of the cord, noting which nuclei are found only in restricted parts of the cord.
Brainstem and Cranial Nerves
1. Describe the morphology of the brainstem
Describe the major external features of the ventral, dorsal and lateral surfaces of the medulla, pons and midbrain.
Correlate the external features with the appearance of transverse sections at these levels: caudal and rostral medulla, pons, midbrain.
Define the regions comprising the tectum, tegmentum and base in brainstem cross-sections, and list the major contents of each.
Identify the major vessels that supply each of the three main brainstem levels, the midbrain, pons, and medulla.
Summarize the functions of the brainstem and correlate with the 4 D mnemonic (diplopia, dysphagia, dysarthria, dysmetria) for dysfunction due to brainstem damage.
2. Describe the 12 cranial nerves.
List the name, number, attachment site, and basic functions of each of the cranial nerves.
Identify on specimens the cranial nerves that arise from the forebrain, midbrain and hindbrain.
Distinguish between sensory and motor cranial nerve nuclei.
Predict the deficit associated with damage to each cranial nerve or its associated nucleus/nuclei.
Spinal Cord and Spinal Nerves
Dr. Claudia Krebs introduces the gross morphology of the human spinal cord. Use full screen mode where available.
(click here if you would like to watch the entire presentation with closed captioning.)
Dr. Suzanne Stensaas surveys regional variations in the gray and white matter of the spinal cord and describes a simple monosynaptic reflex.
(click here if you would like to watch the entire presentation with closed captioning.)
Be sure you can distinguish dorsal (posterior) from ventral (anterior) cord and rootlets. These images will help.
Check your learning! Enlarge the image and look for the faint shaded boxes to drag the labels into (they are subtle, sorry!)
Clinical Considerations
Terminology
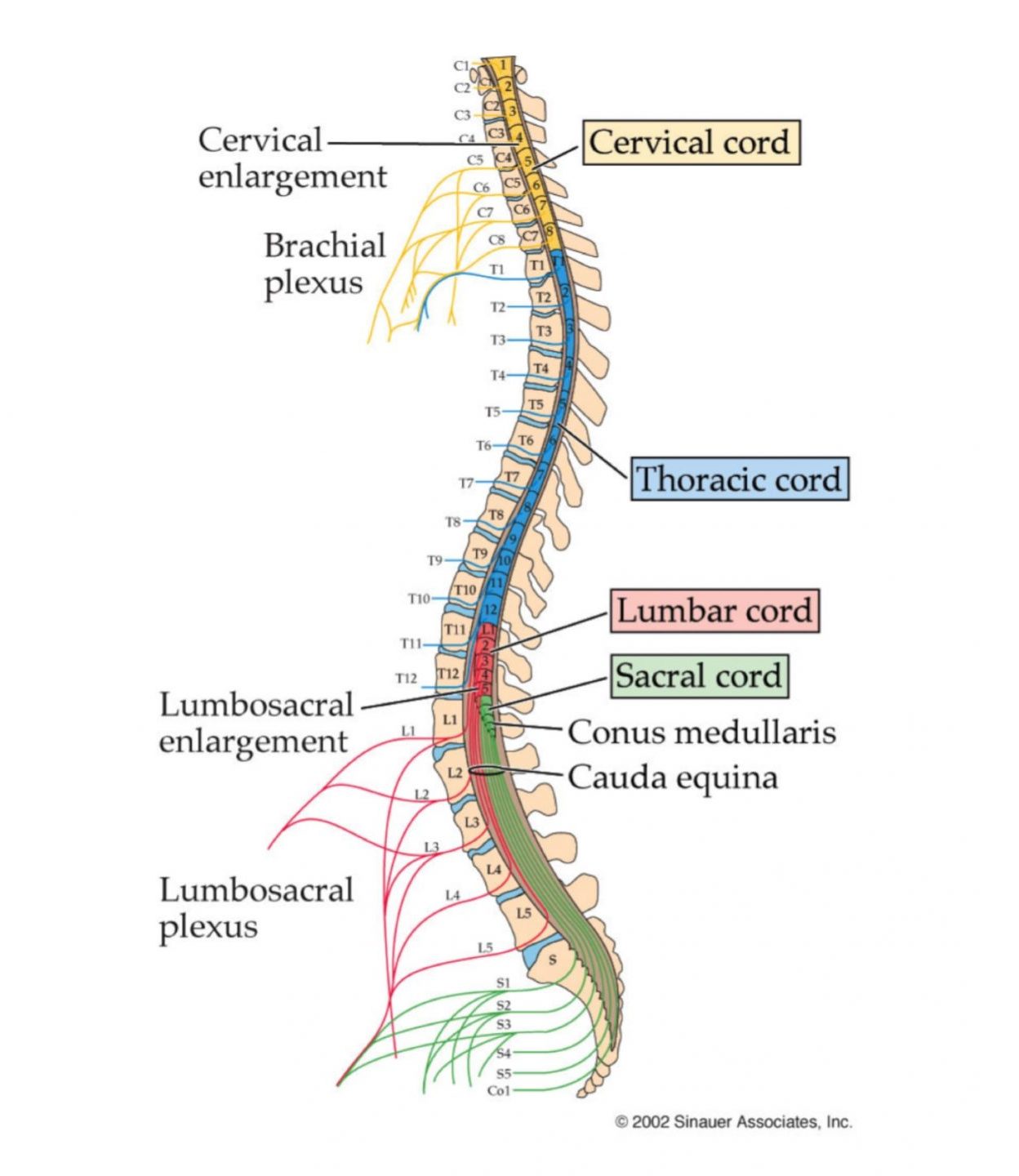
It is important to be clear in communicating about the spinal cord in clinical situations. For example, when someone refers to “C5” be sure you know whether they are referring to a vertebra, a vertebral level, a spinal nerve, a spinal cord segment, or a dermatome! Note that this might be especially important when referring to the spinal cord, because of the discrepancy between a spinal cord segment and the vertebra of the same number. Recall that the cord itself has 8 cervical segments, but there are only 7 cervical vertebrae, and that the cord ends at the intervertebral disk between L1 and L2 vertebra. Thus, the sacral cord segments are all above the L2 vertebra. The image below reminds you of the discrepancy between spinal cord segment and vertebral level.
Lumbar puncture
Lumbar puncture (spinal tap) can be useful in gaining access to CSF in the subarachnoid space of the lumbar cistern. To avoid damaging the cord, the needle needs to be placed well below the intervertebral disk between L1 and L2 (where the conus medullaris is typically found), usually between L4 and L5 vertebrae. In lumbar punctures, CSF pressure can be assessed, CSF can be sampled for diagnostic purposes (eg to check for bleeding or infection), CSF can be withdrawn to decrease intracranial pressure, or therapeutic agents can be introduced (eg intrathecal chemotherapy).
Anesthesia
The spinal cord and spinal nerves serve as convenient locations for introducing anesthetic agents for analgesia that act without changing levels of consciousness.
In epidural anesthesia, a catheter is introduced into the epidural space in the vertebral canal surrounding the cord. This space contains fat, connective tissue and venous plexuses. The catheter can be advanced to the level of the spinal nerves that serve the region to be anesthetized, for example, during parturition, the catheter can be positioned alongside sacral spinal cord segments to block pain from the perineum.
In spinal anesthesia, anesthetic is deposited (usually as a single injection) directly into the subarachnoid space, and thus into the CSF near the roots and spinal cord segments to be blocked. In this kind of anesthesia, care must be taken to avoid damage to the spinal cord itself, and precautions are taken to reduce the diffusion of agent widely through the CSF. It is useful for blocking the lower cord.
Cross-sections of spinal cord
Throughout the cord, gray matter of the dorsal and ventral horns forms a recognizable H-shape surrounded by columns of white matter dorsally, laterally and ventrally.
The ventral horn is significantly larger in the cervical and lumbar enlargements, to accommodate the “extra” neurons needed for control of limb muscles.
In the T1-L2 segments, there is a lateral horn formed by the cell bodies of sympathetic preganglionic neurons, and in the same segments, an additional nucleus at the base of the dorsal horn – Clark’s nucleus – serves as a relay nucleus for somatosensory information to the cerebellum.
White matter consists of interconnections between spinal cord segments and long tracts ascending (sensory) to and descending (motor) from the brain. The upper cervical region contains the most white matter of any cord region as all the sensory information has accumulated from the body, while the motor tracts have not yet begun terminating on their target motor neurons in the ventral horn.
Use the following exercises to review cross-sectional anatomy of the cord. Remember in this course, we use images of myelin-stained histological sections, so white matter appears dark and gray matter appears pale.
(in the following exercises, remember to click on the “i” symbol for tips and hints)
Brainstem
Dr. Krebs provides an overview of the parts of the brainstem in anterior, posterior and midsagittal views.
(click here if you would like to watch the entire presentation with closed captioning.)
Check your learning!
Brainstem Contours
 Study the surface morphology of the brainstem using the images above. Recall that it is not a uniform cylinder of tissue (as the spinal cord is), but has bumps and fissures and fossae. Its internal morphology is also more complicated than the relatively simple gray/white matter pattern seen in the cord. We will be studying the brainstem in detail in upcoming labs, but here we introduce you to sections through 4 key levels. Before even considering the internal morphology, it is possible to distinguish levels of brainstem in section by characteristic surface profiles. Use the sliders in the exercises below to confirm that:
Study the surface morphology of the brainstem using the images above. Recall that it is not a uniform cylinder of tissue (as the spinal cord is), but has bumps and fissures and fossae. Its internal morphology is also more complicated than the relatively simple gray/white matter pattern seen in the cord. We will be studying the brainstem in detail in upcoming labs, but here we introduce you to sections through 4 key levels. Before even considering the internal morphology, it is possible to distinguish levels of brainstem in section by characteristic surface profiles. Use the sliders in the exercises below to confirm that:
- sections through the midbrain have bumps posteriorly, and two large cerebral peduncles separated by the interpeduncular fossa anteriorly. The cerebral aqueduct is a small circular profile within the posterior third of the midbrain.
- sections through the pons have a smooth anterior profile and the white matter of the cerebellar peduncles is continuous laterally with the white matter of the cerebellum, or the profile will have straight cut edges laterally that allowed for the removal of the cerebellum.
- sections through the rostral medulla have an anterior median fissure, and the olive shows up prominently anterolaterally. The posterior edge of the section is part of the floor of the 4th ventricle.
- sections through the caudal medulla resemble the spinal cord in having a circular profile, an anterior median fissure, and a central canal with the section.
Remember that in clinical imaging, anterior is at the top of the page and the image is viewed from below, as if you were standing at the foot of a bed on which the patient is lying on their back. However, in histological preparations, anterior is most often at the bottom of the page and there is no convention about right and left sides of the specimen, so there is no way to distinguish left from right unless indicated with a label.
In each of the following use the slider to compare section plane, myelin-stained section and MRI appearance at each level.
Try this quick flash card deck to check whether you can distinguish different levels of the brainstem in different imaging modalities.
Dr. Stensaas provides a summary of sectional anatomy of the brainstem. View in full screen mode to consolidate your understanding.
(click here if you would like to watch the entire presentation with closed captioning).
Tectum, Tegmentum and Base
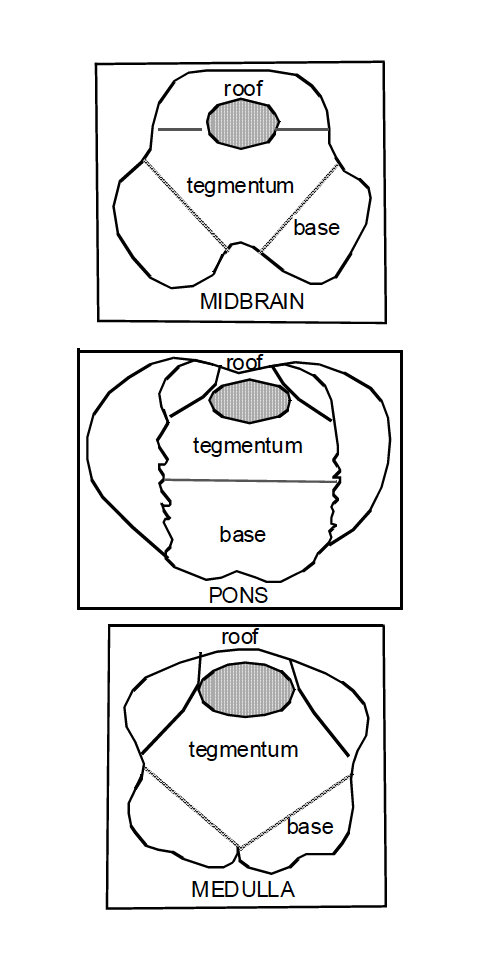
The internal organization of the brainstem is complicated and we use some “geographical” terms for describing the locations of specific nuclei and tracts in brainstem cross-sections.
The part of the brainstem dorsal to the ventricular profile is the tectum or roof. This is only seen in the midbrain and is the colliculi.
The most ventral (anterior) third to half of a brainstem cross-section is the base. The base contains the important descending tract for voluntary motor control and related nuclei (eg inferior olivary nuclei, substantia nigra, pontine nuclei)
The remaining part of any cross section is the tegmentum (‘shelter’) where you will find the ascending (sensory) pathways, pathways interconnecting parts of the brainstem, cranial nerve nuclei, and nuclei and circuitry for autonomic control and consciousness.
Cranial Nerves
In this video, Dr. Krebs demonstrates the attachment points of the cranial nerves. View in full screen mode for best resolution.
(click here if you would like to view the entire presentation with closed captioning).
Dr. Stensass provides a review on brainstem and cranial nerves. It is helpful to know attachment points of cranial nerves, because in most cases, the cranial nerve nuclei associated with a cranial nerve are located in the plane at the point of attachment of the nerve. Skip this if you feel confident about the external morphology from earlier labs.
(click here if you would like to view the entire presentation with closed captioning).
Cranial nerve attachment points: Check your learning!
Here is a summary of cranial nerves for reference. As the course progresses, we will cover cranial nerves and their nuclei in the context of systems, and you can refer back to this table as needed.
Sensory function of cranial nerves: check your learning by dragging and dropping the correct cranial nerve to the description of its function, referring to the image immediately below.
Motor and parasympathetic function of cranial nerves: check your learning by dragging and dropping the correct cranial nerve to the description of its function, referring to the image immediately below.
Cranial Nerve Nuclei
Cranial nerve nuclei are collections of neuron cell bodies whose axons either
- innervate striated, voluntary muscles of the head and neck or parasympathetic targets such as smooth muscle and glands (cranial nerve motor nuclei), or
- process sensory input from the head, neck and viscera conveyed via sensory components of cranial nerves (cranial nerve sensory nuclei).
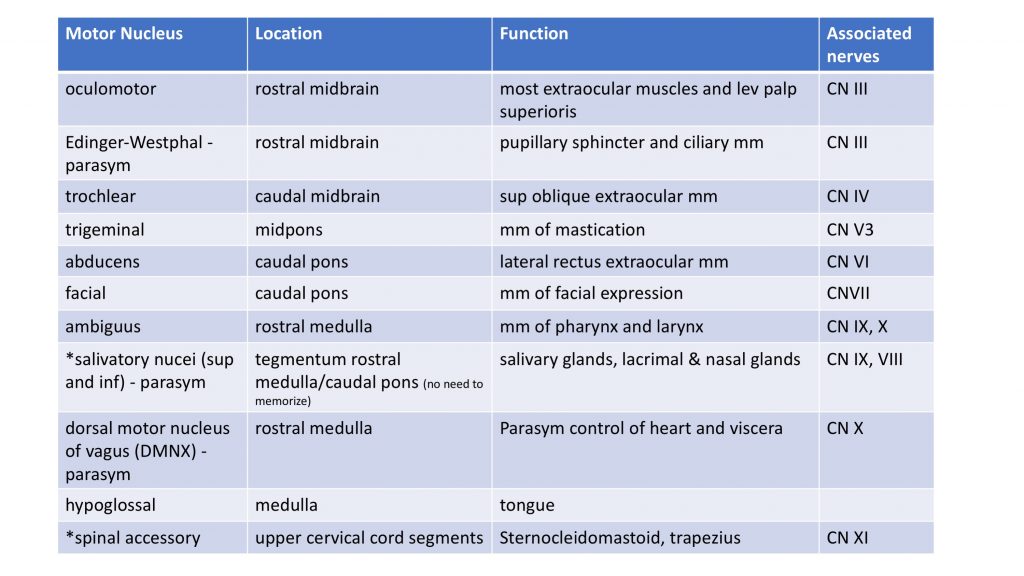
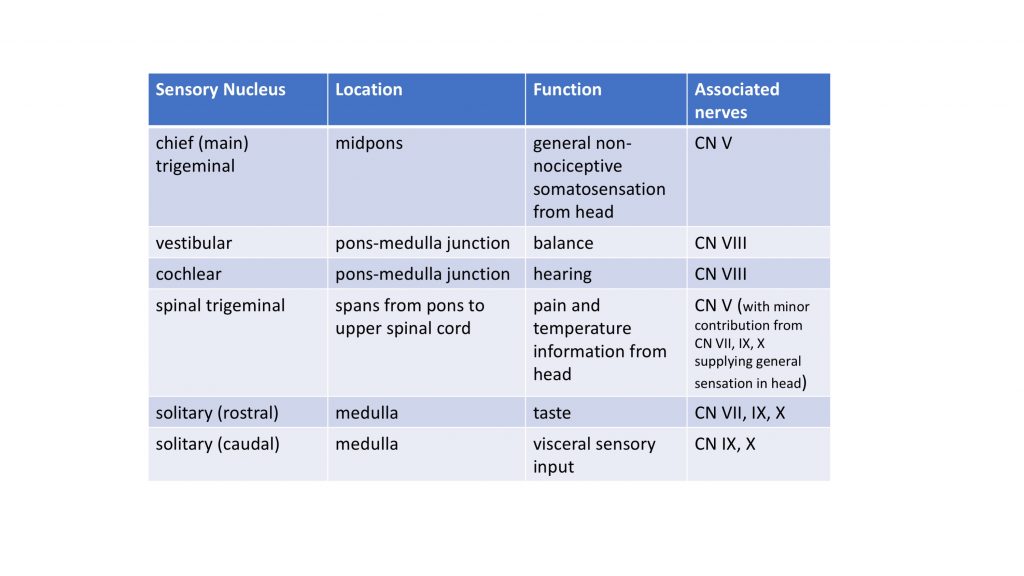
Review this diagram from Dr. Pradhan’s lecture showing the rostrocaudal extent of the nuclei. Note that each cranial nerve is associated with at least one and sometimes several nuclei (indicated in parentheses) and vice versa. Blessedly, many nuclei are named the same as their related cranial nerve! In the image, for simplicity’s sake, nuclei are shown on one side, but of course, they are present bilaterally. Motor nuclei are brown, sensory nuclei are blue, and nuclei associated with viscera (parasympathetic motor nuclei on left of image, visceral afferent nuclei on right) are green.
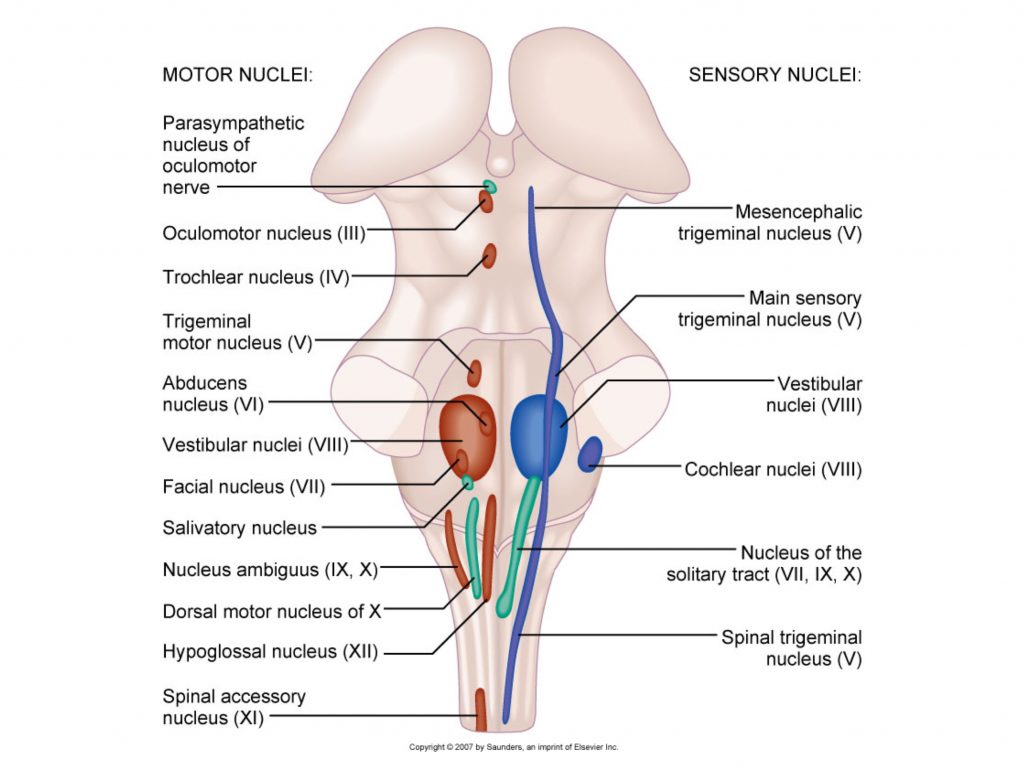
Tips for localizing nuclei:
- they are generally located close to the point of attachment of the associated cranial nerve(s). For example: the oculomotor nuclei and trochlear nuclei are in the midbrain.
- you will always find the nuclei in the tegmentum of the brainstem.
- sensory nuclei will be located more laterally, while motor nuclei are located more medially.
The following tables, which organize the nuclei by function, should help you become familiar with cranial nerve nuclei in myelin-stained sections.
Please rest assured that we will be re-visiting this material in the context of systems as we progress through the course.
 Blood Supply
Blood Supply
If you know the surface of the brainstem and the relationship of overlying arteries, you can predict the blood supply for any part of the brainstem because arteries supply branches to the tissue deep to their paths.
See what you remember from Lab 1!
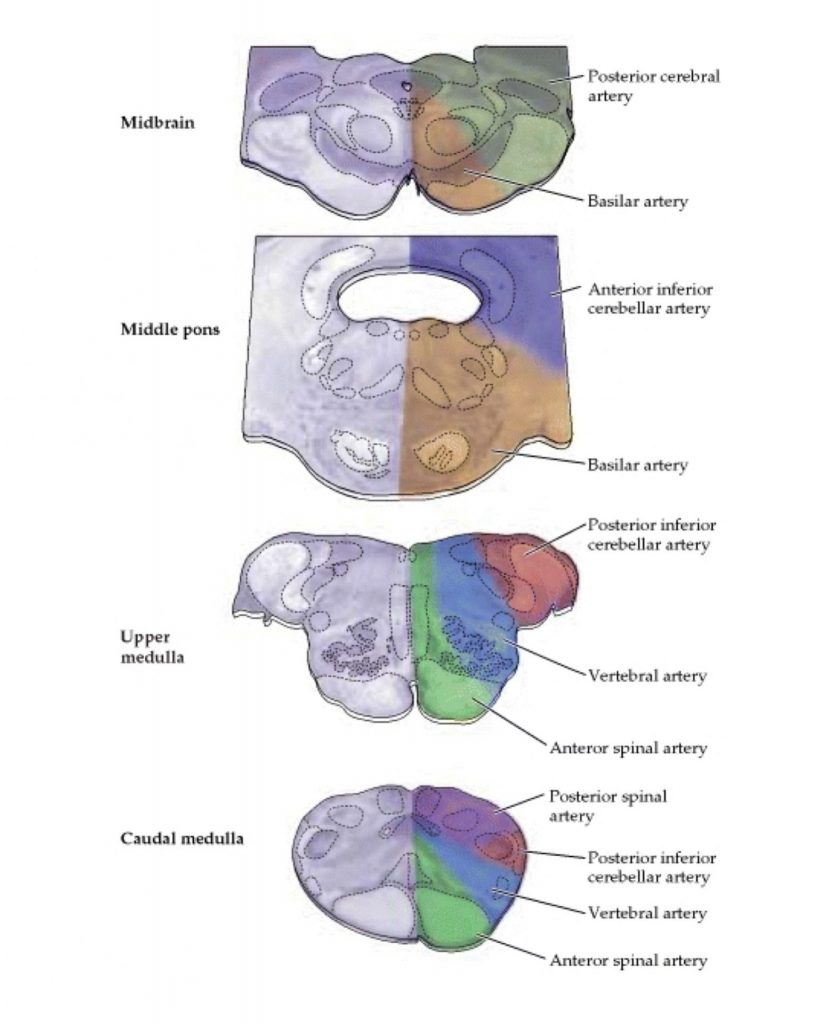
Here is the image from lecture to remind you of arterial territories in the brainstem. Now would be a good time to review drawing the vertebro-basilar system superimposed on the ventral surface of the brainstem!
Clinical considerations
The brainstem is a remarkable piece of CNS “real estate” essential for life. Brainstem reflexes are used as part of the diagnosis of brain death. Testing brainstem reflexes, just like testing limb reflexes, is a convenient way to do a quick assessment of function. Here are some key reflexes involving cranial nerves and their interconnection in the brainstem.
- pupillary light reflex: light shone in one eye results in constriction of pupils of both eyes. Tests, CN 2 (input), CN 3 on both sides (output), and the midbrain connections between them.
- corneal reflex: lightly touch of one cornea with a piece of sterile cotton results in eye closure on both sides. Tests CN 5 (input), CN 7 on both sides (output) and their interconnections through the pons.
- gag reflex: light stimulation of the posterior tongue/pharynx with a tongue depressor results in a contraction of pharynx and larynx. Tests CN 9 (input) and CN 10 (output)
- vestibulo-ocular reflex: head rotation to one side results in equal and opposite rotation of both eyes to other side to compensate. Tests CN 8 (input), and CN 6 and CN 3 (outputs) as well as the brainstem connections among them from rostral medulla to midbrain.
Brainstem Strokes
Combining knowledge of brainstem anatomy and blood supply allows one to predict the clinical presentation of various vascular and other insults. in upcoming labs we will be integrating and adding to our understanding of the brainstem, so do what you can to get familiar with this material and things will get easier as we go! (You have already had a taste of this integration in lecture).
Brainstem “Rule of 4”
Clever people have encapsulated the structure and function of the brainstem in a “rule of 4” mnemonic. At this point, we have not covered everything in the rules, but it may be helpful to know about this mnemonic. Like all simplifications, there are inconvenient truths that are ignored (eg motor nuclei for muscles derived from branchial arches are omitted), but if it helps you, use it (with caution!)
There are 4 medial (‘M’) structures:
- Motor pathway (corticospinal tract)
- Medial lemniscus (a sensory pathway)
- Motor nuclei and nerves that divide equally into 12 (that is CN III, IV, VI and XII)
- Medial longitudinal fasciculus (tract interconnecting extraocular and vestibular nuclei)
There are 4 ‘side’ (‘S’) i.e. lateral, structures:
- Spinothalamic pathway (a sensory pathway)
- Sensory nuclei of the trigeminal nerve
- Spinocerebellar pathway (sensory pathway to cerebellum)
- Sympathetic pathway (from hypothalamus to lateral horn of spinal cord T1-L2 levels)
There are 4 cranial nerves attached at the medulla:
CN IX, X, XI, XII (strictly speaking XI is attached at the cervical spinal cord but it exits the skull with CN X)
There are 4 cranial nerves attached at the pons:
CN V, VI, VII, VIII
There are 4 cranial nerves above the pons:
CN I, II, III, IV (CN I and II are in the forebrain not brainstem)
There are 4 deficits (‘D’) associated with damage to the brainstem:
- Dizziness (usually signals something wring with the vestibular system)
- Diplopia (often due to misalignment of the eyes due to imbalance between actions of extraocular muscles)
- Dysarthria (difficulty controlling muscles involved in speech)
- Dysphagia (difficulty controlling muscles involved in eating/swallowing)
Here’s a short quiz
Phew! that’s a lot of information. Do your best and we promise things will all fall into place over the next few weeks as we explore this material in the context of specific systems.
Structures to Identify
