3 Synaptic Transmission
Learning Objective 4: Describe the mechanism by which neurotransmitter is cleared at chemical synapses
Synaptic potentials vary widely in time course. The speed of synaptic transmission is influenced by: (1) the time required for transmitter to be released and diffuse across the synaptic cleft— which is typically extremely short, and (2) the time required to generate the postsynaptic conductance change—which is quite variable. As described above, rapid release of transmitter relies on the close proximity of the vesicle release sites and the Ca2+ channels that permit Ca2+ to enter the nerve terminal and trigger exocytosis. The time for diffusion across the synaptic cleft is minimized by the close proximity of pre and post-synaptic membranes.
Postsynaptic events substantially shape the time course of the synaptic potentials and in doing so introduce diversity in the time course of synaptic potentials. An important division is into fast versus slow chemical synaptic transmission:
1. Fast synaptic transmission: Neurotransmitter binds to and activates receptors that are ligand-gated ion channels – these are referred to as ionotropic receptors (Learning Objective 3). The lack of intermediate steps between transmitter binding and the conductance change leads to a brief synaptic potential (1–20 ms in duration typically).
Recovery of the synaptic potential is mediated by receptor desensitization and by clearance of released transmitter. Receptor desensitization occurs when the channel associated with the receptor closes even though transmitter is still bound to the receptor – a situation a bit like inactivation of voltage-gated Na+ channels. Transmitter clearance at neuromuscular junctions is achieved via degradation of ACh by acetylcholinesterase; this is atypical, however, and other types of released neurotransmitter are cleared by transporters. Transporters located on glial cells near the synapse play a central role in “reuptake” or clearance of released transmitter (Learning Objective 4). These transport proteins do not use ATP but instead obtain the energy they need to move neurotransmitter out of the synaptic cleft by allowing ions such as Na+ to flow down their electrochemical gradient; as a result, they are Na+-coupled cotransporters (see also membrane transporter class). Several therapeutic drugs target these transporters (see below).
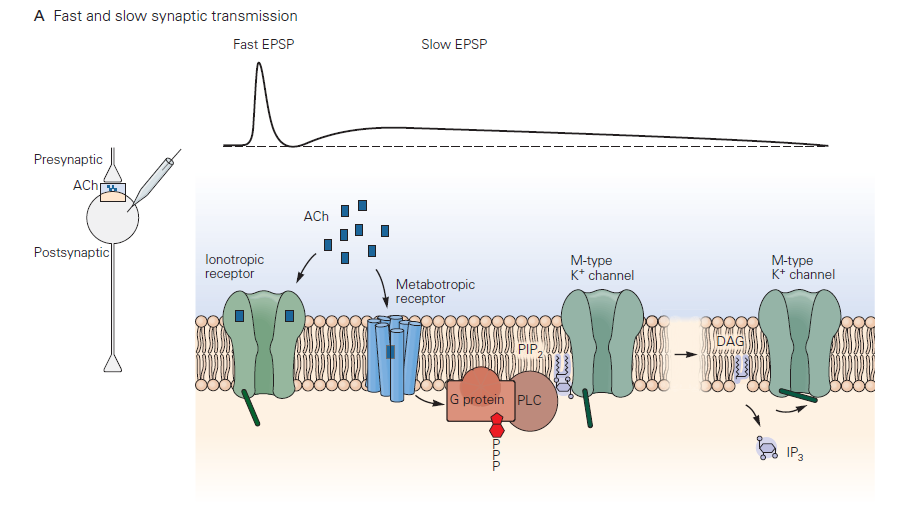
- Slow synaptic transmission: This type of postsynaptic response mechanism differs radically from that in fast chemical transmission. Neurotransmitter binds to and activates a G-protein- coupled receptor (GPCR) – referred to by neurobiologists as a metabotropic receptor (Learning Objective 3). This leads to G-protein signaling and a cascade of biochemical events that may include opening or closing of ion channels, producing a slow synaptic potentials. The electrical response, as you would guess, takes longer to initiate and terminate than fast synaptic potentials due to the delays introduced by the chemical reactions comprising the G-protein cascade. Typical durations can be several to many seconds. A reason for the longer lasting synaptic potentials is that the biochemical events leading to conductance change can persist well after the transmitter has been removed from the synaptic cleft. The duration of slow synaptic potentials is determined by the time to shut off the activated G-protein signaling components. The G-protein needs to hydrolyze GTP to GDP, and downstream biochemical processes and second messengers need to return to the resting state.
Aside: Drugs acting on synaptic transmission
Many therapeutic and recreational drugs act on synaptic transmission. These have also been key tools in furthering our understanding of how synaptic transmission works. Essentially every component of the synapse is a target:
- Receptor enhancement: Benzodiazepines enhance effects of GABA. These drugs strengthen GABA synapses by causing the postsynaptic receptors to be more sensitive to GABA released by the presynaptic cell. These drugs are tranquilizers and may induce sleep.
- Receptor agonists: LSD mimics serotonin at serotonin receptors. The result may be hallucinations. Receptor agonists severely alter synaptic transmission by directly binding to and activating neurotransmitter receptors and bypassing transmitter release from the presynaptic cell.
- Receptor antagonists: Antipsychotics block dopamine receptors (e.g. haloperidol). Curare blocks nicotinic ACh receptor leading to muscle paralysis. These drugs suppress synaptic transmission by partially or completely blocking neurotransmitter receptors.
- Reuptake blockers: Most antidepressants inhibit serotonin uptake (e.g. Prozac); cocaine blocks norepinephrine, serotonin and dopamine uptake. These drugs permit released transmitter to remain in the synaptic cleft for a longer period of time and thus to elicit a stronger postsynaptic response. Unlike for receptor agonists, here the generation of a signal in the postsynaptic cell still relies on release of a chemical neurotransmitter.
- Block enzymatic degradation: Nerve gases, some insecticides, and research and clinical anticholinesterases inhibit degradation of ACh by acetylcholinesterase at the cholinergic junction. Like reuptake blockers, these drugs permit transmitter to remain in the synaptic cleft for a longer period of time. Low doses of such drugs may have therapeutic effects by enhancing the response to released transmitter (much like drugs that block reuptake mechanisms at other synapses). Nerve gases typically work by asphyxia as the muscles controlling breathing cease to be controlled.
