18 Spinal Reflexes
NOTE: Optional
The content below about spinal reflexes will be covered during lecture and tested on the lecture exam, not the quiz section test.
Introduction
In a reflex, a stimulus to a sensor leads to a response in an effector. The neural pathway controlling the reflex is called the reflex arc. The reflex arc for a spinal reflex consists of the afferent pathway, a portion of the central nervous system, and an efferent pathway. In a spinal reflex, the integration for the behavior occurs entirely in the spinal cord, thus the behavior occurs automatically and doesn’t require input from the brain (although the reflex may be modulated by brain input). Spinal reflexes are often used in neurological testing because they are simple, reproducible behaviors.
The Stretch Reflex
The stretch reflex is a commonly tested reflex in medical practice. People are most familiar with this reflex at the knee. The physician uses a reflex hammer to rap on the patellar tendon. As a result of activation of the reflex arc, the lower leg kicks forward. Technically speaking, the behavior that occurs is extension of the leg at the knee. The figure below shows the circuitry underlying the stretch reflex.
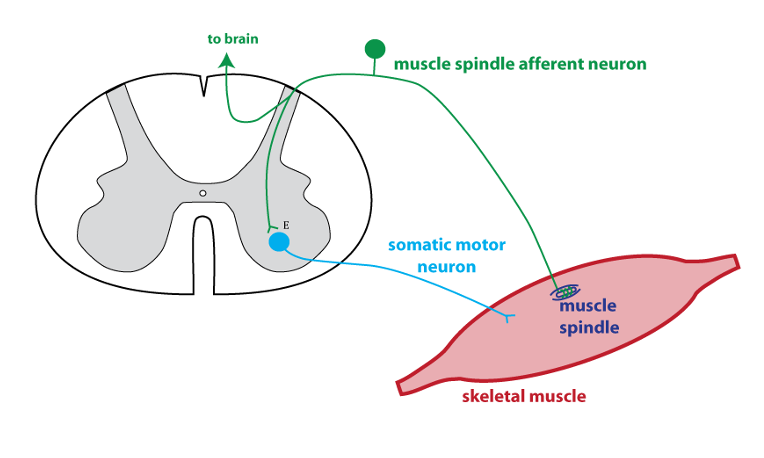
The rap of the tendon acts to stretch the muscle. This activates sensors called muscle spindles. Muscle spindles are proprioceptors (see below) that monitor muscle length. The stretch of the muscle causes increased action potentials in the muscle spindle afferent (green). The muscle spindle afferent makes a direct synaptic connection to a somatic motor neuron that innervates the same muscle. Thus when the muscle spindle afferent is activated by stretch, it excites the somatic motor neuron to cause contraction in the same muscle.
Returning to the test described in the first paragraph, the rap on the patellar tendon lengthens muscles in the quadriceps group (located on top of the thigh). The reflex response is contraction of these muscles, i.e. extension of the lower leg. The quadriceps stretch reflex is the one most often tested in a general physical exam, but all the muscles have stretch reflexes.
Proprioceptors
“Proprio-” means “self”, and proprioceptors such as the muscle spindle provide information that is intergrated in the brain to provide information about the position of the limbs in space (note that the muscle spindle afferent sends an axon branch to the brain). Muscle spindles are small sensory organs that are scattered throughout the body of the muscle, in parallel to the muscle fibers.
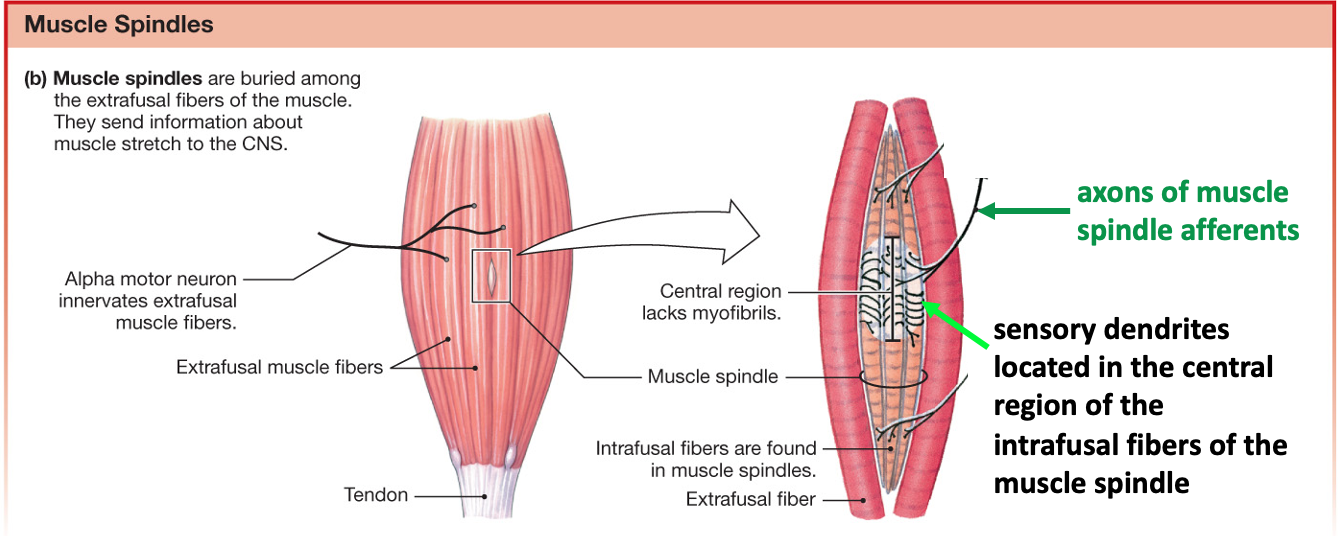
Muscle spindles provide information about muscle length. Another type of proprioceptor is the Golgi tendon organ. Golgi tendon organs are located in the tendons and are best stimulated when the muscle pulls on the tendon. Thus, the Golgi tendon organ provides information about muscle tension.
Reflexes in Neurological Testing
The test of the stretch reflex is used to evaluate the elements in the reflex arc, but also higher motor control centers in the central nervous system. If the stretch reflex is weak or nonexistent, that indicates that there is damage to the neurons in the reflex arc.
Spinal neurons involved in the stretch reflex receive input from the brain, so brain and spinal cord damage can affect the strength of the stretch reflex. Recall that the upper motor neurons are neurons whose cell bodies are located in the primary motor cortex, and whose axons descend to the spinal cord via the corticospinal tract. Upper motor neuron input has a largely inhibitory effect on the stretch reflex. Thus, upper motor neuron disorders are characterized by hyperreflexia (exaggerated reflexes) and hypertonia (increased muscle tone).
Another abnormal behavior associated with an increased stretch reflex is called clonus. Clonus is an oscillatory movement, usually observed at the ankle joint. A muscle stretch causes a beating motion of the foot due to alternating contractions of antagonist muscle groups. The video clip in this article shows sustained clonus in a patient who had suffered a stroke (“Clonus after a Stroke” (2013) New England Journal of Medicine 368:e2). Clonus, hyperreflexia, and hypertonia are considered positive signs associated with upper motor neuron disorders (see the section on Motor Pathways in the chapter on Brain Anatomy).
Another reflex that can reveal damage to the upper motor neurons is the Babinski reflex (also called the plantar reflex). To test this reflex, a blunt object, such as the handle of the reflex hammer, is run along the lateral sole of the foot, moving from the heel in the direction of the toes. If there is no damage to the corticospinal tract, the patient will curl the toes. If there is damage to the corticospinal tract, the response is extension of the big toe and fanning of the other toes. This is known as a positive Babinski sign. Infants also have a positive Babinski sign due to the fact that the corticospinal tract is not yet fully myelinated.
To summarize, the stretch reflex is a simple, stereotyped behavior that can be tested as a means of assessing neurological damage.
- Damage to the reflex arc causes a weak or absent stretch reflex.
- Upper motor neuron disorders increase the stretch reflex, causing hyperreflexia and hypertonia.
