7 Brain Anatomy
Surface Features of the Brain
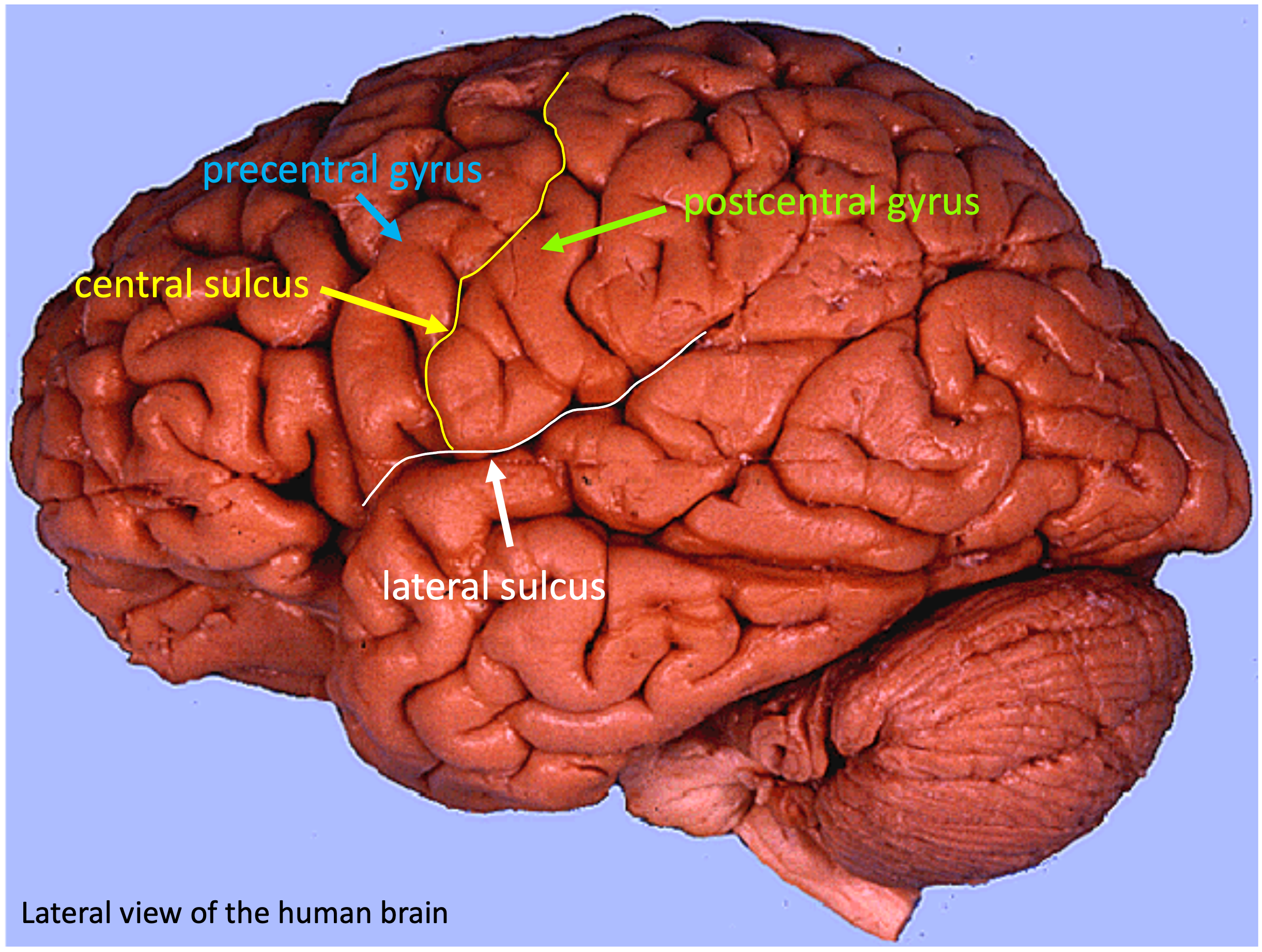
The rostral part of the neural tube expands much more extensively than the more caudal portions to form the cerebrum or cerebral hemispheres. The rapid growth of the cerebrum within the rigid confines of the skull results in the tissue being thrown into convoluted folds. A fold of cerebral tissue is called a gyrus (plural: gyri) and a groove (between folds) is called a sulcus (plural: sulci). The entire surface of the cerebrum is called the cerebral cortex. It contains layers of neuronal cell bodies.
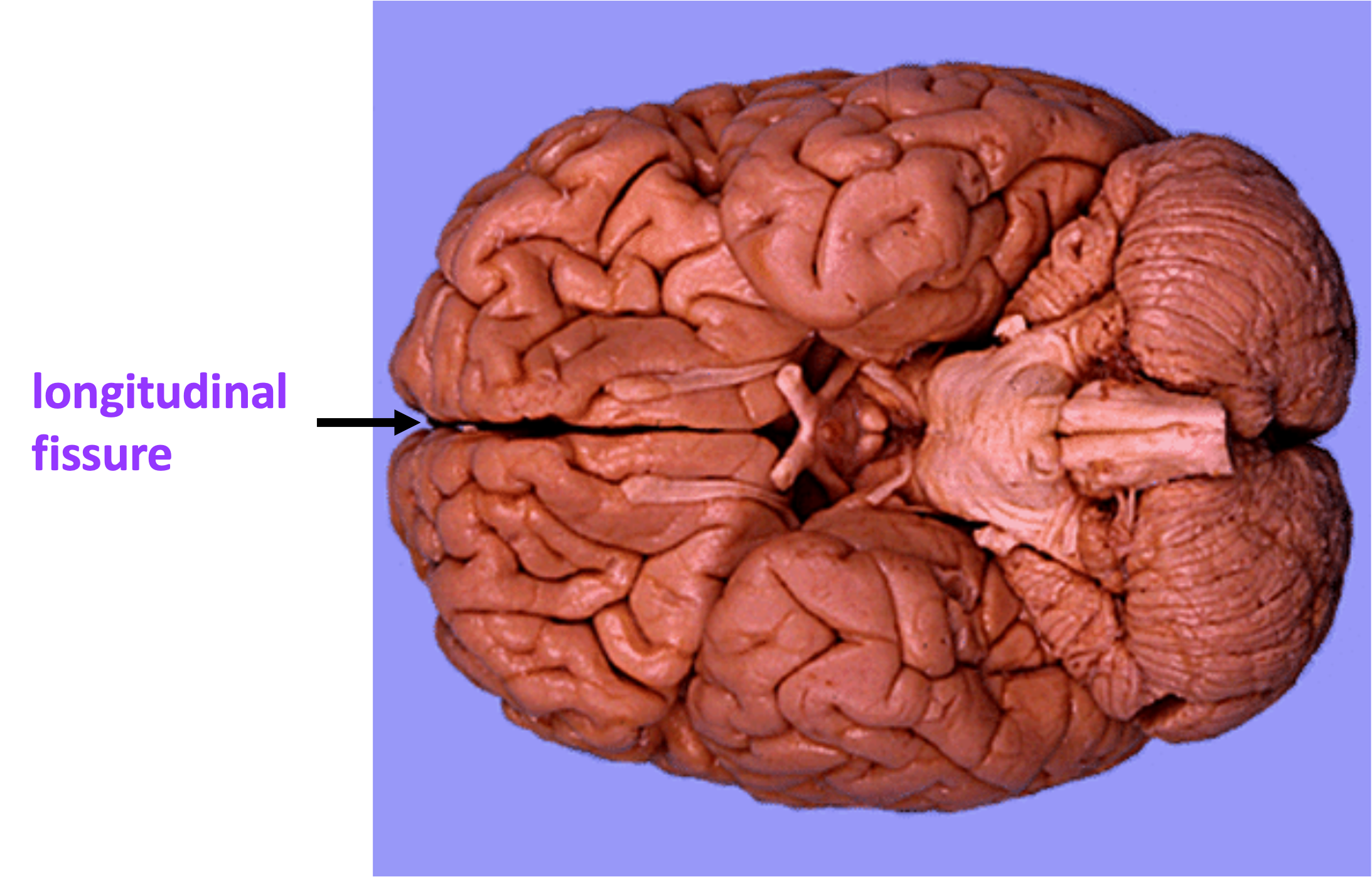
The different lobes of the cerebrum (frontal lobe, parietal lobe, occipital lobe, temporal lobe) are named for the overlying skull bones. The large groove that divides the two cerebral hemispheres is called the longitudinal fissure. The longitudinal fissure can be seen in an inferior view of the brain.
The large groove between the temporal lobe and the frontal and parietal lobes is called the lateral sulcus (also called lateral fissure or Sylvian fissure). The central sulcus extends from the lateral sulcus to the longitudinal fissure, and is bordered by two fairly continuous gyri on either side of it. The central sulcus is the landmark that separates the frontal lobe from the parietal lobe. Anterior to the central sulcus is the precentral gyrus, which is the location of the primary motor cortex. The gyrus just posterior to the central sulcus is called the postcentral gyrus. This is the location of the primary somatosensory cortex, which is highly interconnected with motor cortex.
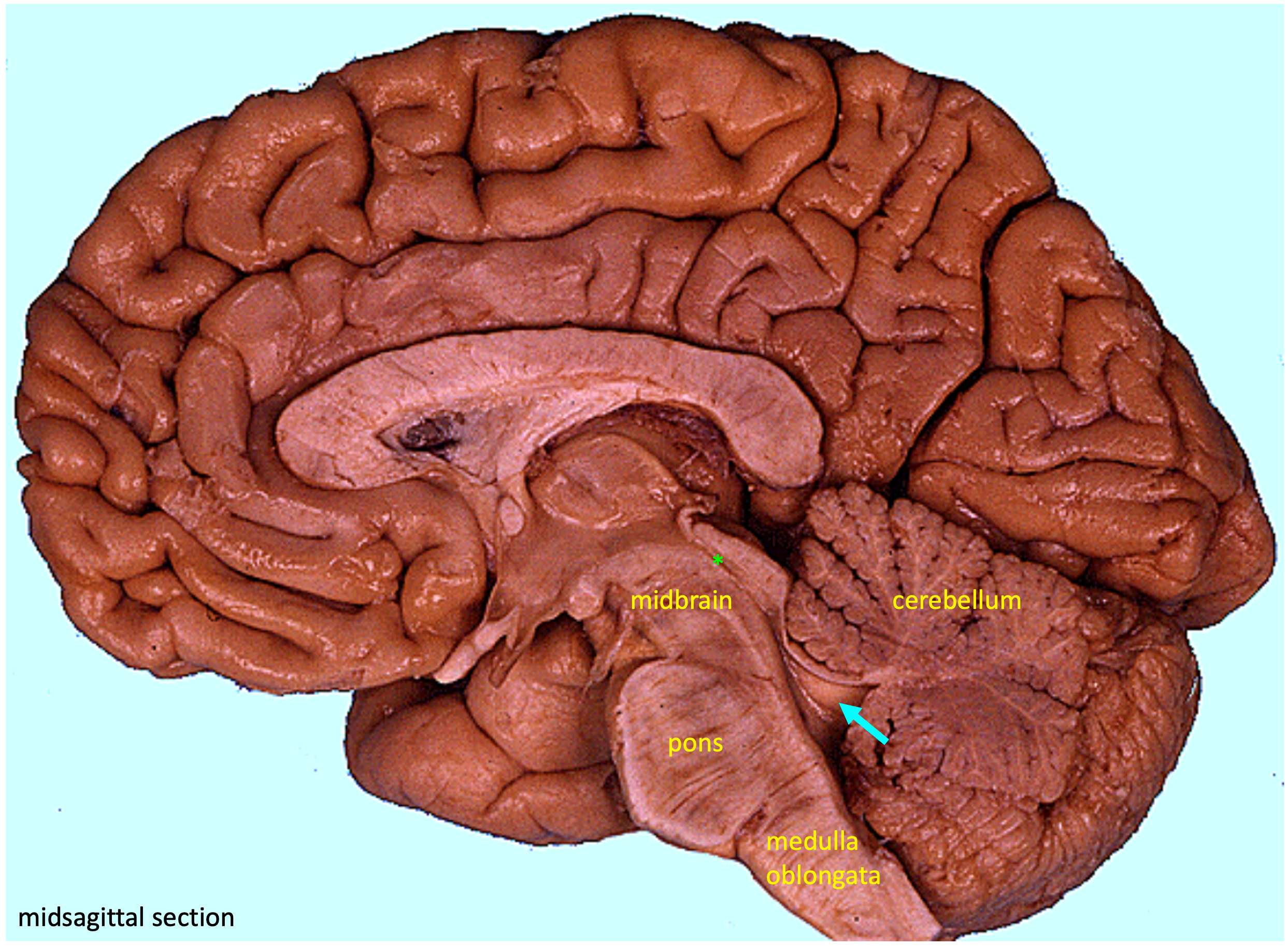
Midsagittal View of the Brain
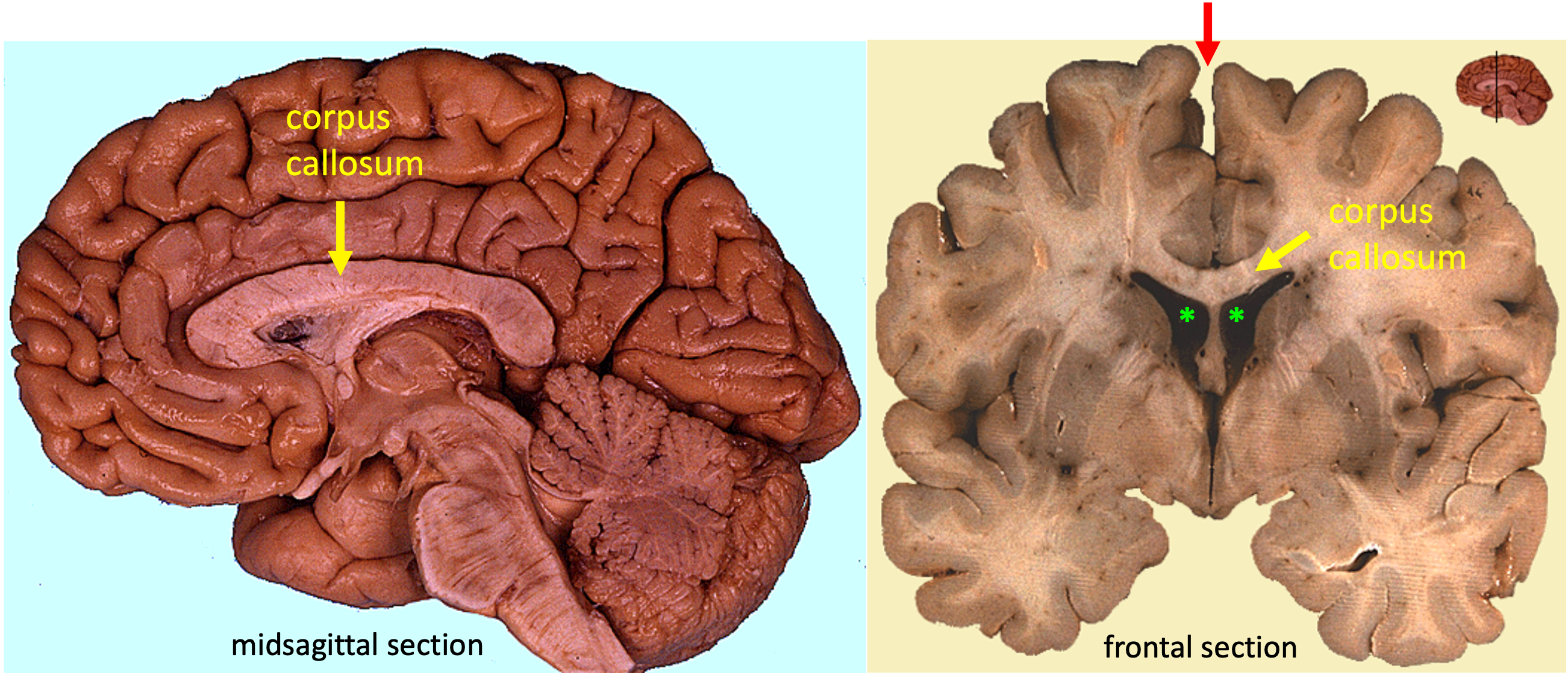
In the midsagittal view of the brain, an obvious feature is the corpus callosum. The corpus callosum is made up of axons and it connects the two cerebral hemispheres. That the corpus callous connects the two cerebral hemispheres is more obvious when looking at a frontal (coronal) section of the brain.
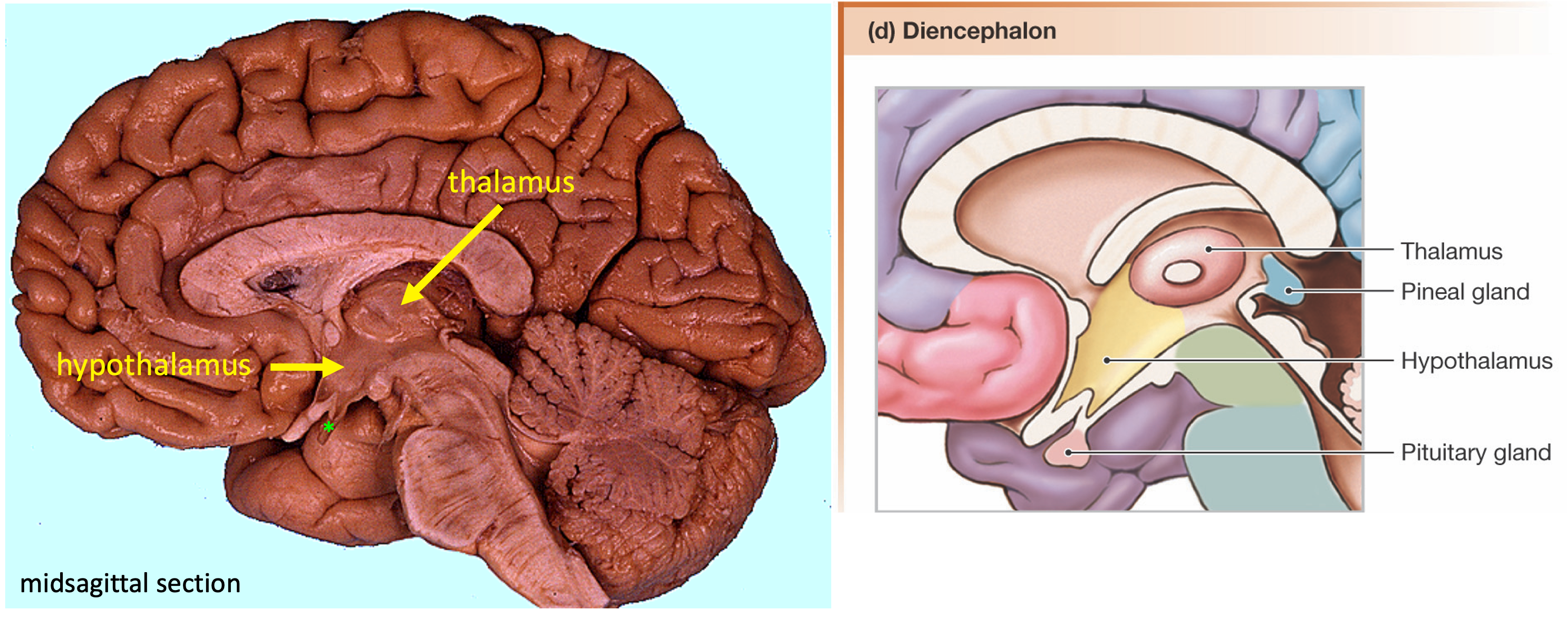
The diencephalon is the region of the brain that lies between the cerebrum and the brainstem. Recall that the diencephalon forms the walls of the third ventricle. This diencephalon contains the thalamus, an oval structure situated just inferior to the corpus callosum. The thalamus acts as a relay station, receiving inputs from almost all sensory systems and relaying that information to the cerebrum. The thalamus is also involved in motor control.
Anterior and inferior to the thalamus is the hypothalamus. The hypothalamus is important for homeostasis, the maintenance of a steady conditions in order to create an ideal internal environment of the body. It contains centers that regulate hunger, thirst, sleep, and other drives. The hypothalamus is also important in endocrine control, regulating hormone release by the pituitary gland, which sits below and anterior to the hypothalamus.
Caudal to the diencephalon is the brainstem, which contains the midbrain, pons, and medulla oblongata. The brainstem is considered the most primitive region of the brain and is concerned with the control of basic processes such as the regulation of breathing, heart rate, and blood pressure. The midbrain tissue surrounds the cerebral aqueduct, the passageway connecting the third ventricle to the fourth ventricle. The cerebellum is the highly folded structure that sits below the cerebrum and posterior to the brainstem. The cerebellum integrates sensory and motor information to provide coordination in movement.
Sectional Views of the Brain
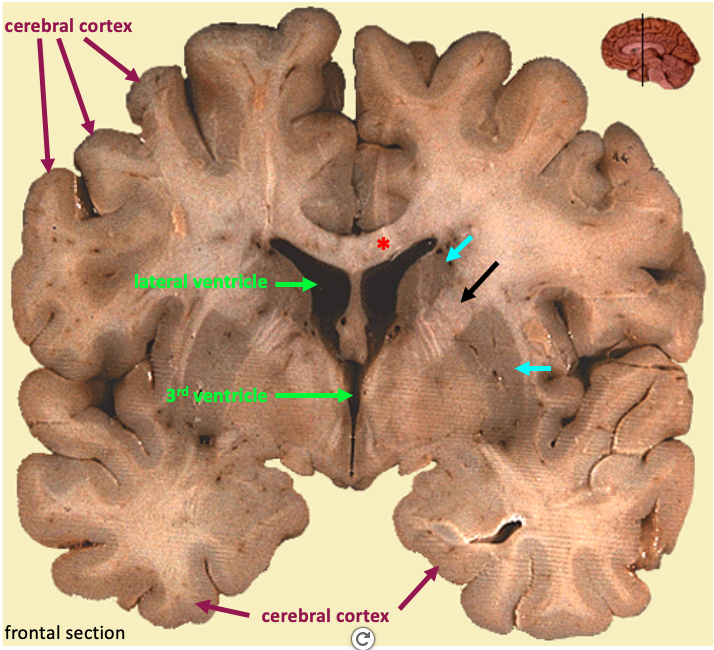
Sections of the brain show the division of the tissue into gray matter and white matter. Gray matter is where neuronal cell bodies are found, while white matter regions mainly contain axons. White matter appears lighter due to the fact that many axons are myelinated.
In the cerebral hemispheres, much of the gray matter is located in the outermost tissue layer called the cerebral cortex. A cluster of neuronal cell bodies within the CNS is called a nucleus. Bundles of axons within the CNS white matter are called tracts. The corresponding term for a bundle of axons that extends outside the central nervous system is nerve (see the section on visual pathways below).
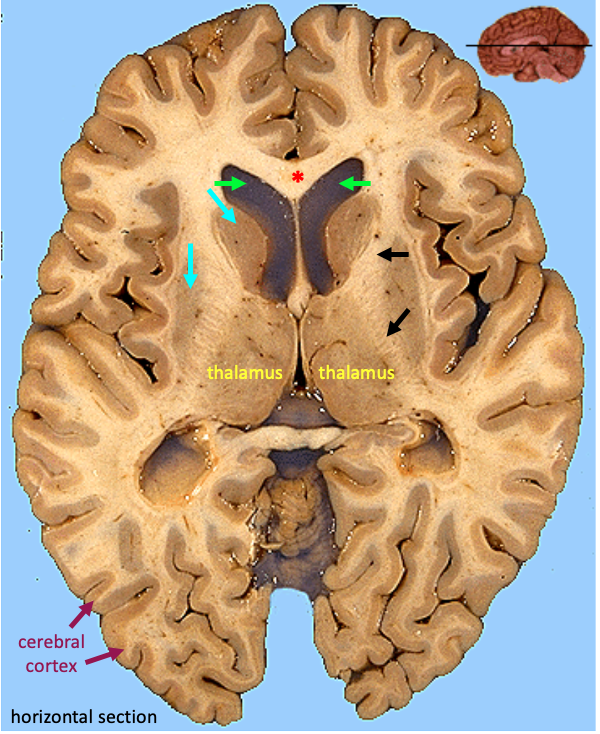
The nuclei and tracts that we will focus on identifying are involved in motor control. The basal ganglia are a group of cerebral nuclei that modulate the output of the motor cortex. (Despite the fact that “ganglion” is used to describe a peripherally located grouping of neuronal cell bodies, most anatomical sources still use the term “basal ganglia” to indicate this group of cerebral nuclei.) The corticospinal tract refers to the axons that extend from upper motor neurons in the primary motor cortex, and that innervate somatic motor neurons in the brainstem and spinal cord (the “lower motor neurons”). The corticospinal tract is a major part of the internal capsule, a white matter structure that extends through the basal ganglia. Look for the gray matter of the basal ganglia to be striped (striated) and separated by the internal capsule.
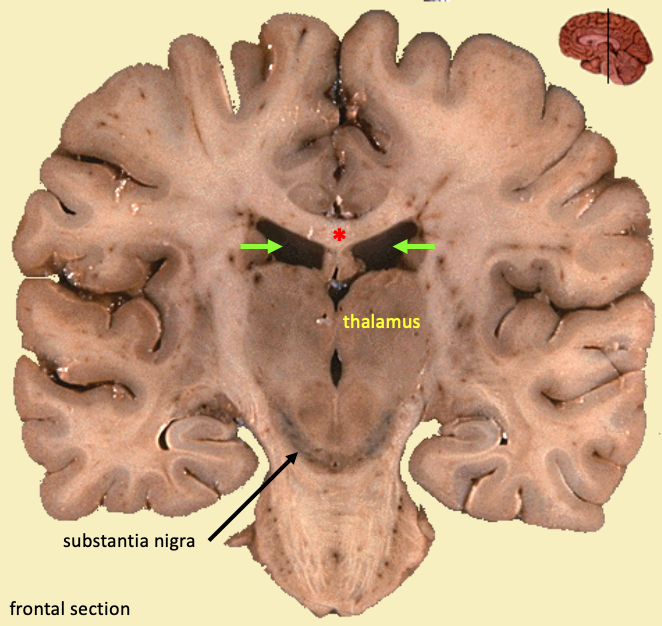
When the frontal section comes from a more caudal location, less of the basal ganglia tissue is visible. Below the lateral ventricles and adjacent to the third ventricle is a large smooth territory of gray matter: this is the thalamus. Also visible in the same section is the darkly pigmented arc of tissue in the midbrain: this is the substantia nigra (substantia nigra literally means “black substance”). The substantia nigra is interconnected with the basal ganglia, and it is often grouped with the basal ganglia because of this functional association. The substantial nigra is the nucleus that degenerates in the disorder Parkinson’s disease.
A horizontal section of the brain would split the brain into an upper and a lower half. The figure below shows the basal ganglia, internal capsule, and the thalamus in a horizontal section.
Visual Pathways
Nerve is the term for a bundle of axons that leaves the central nervous system. Nerves that leave from the brain are termed cranial nerves (spinal nerves leave from the spinal cord). Cranial nerves contain sensory and motor axons for the head and neck, as well as the axons of the special senses (smell, taste vision, hearing, vestibular sense).
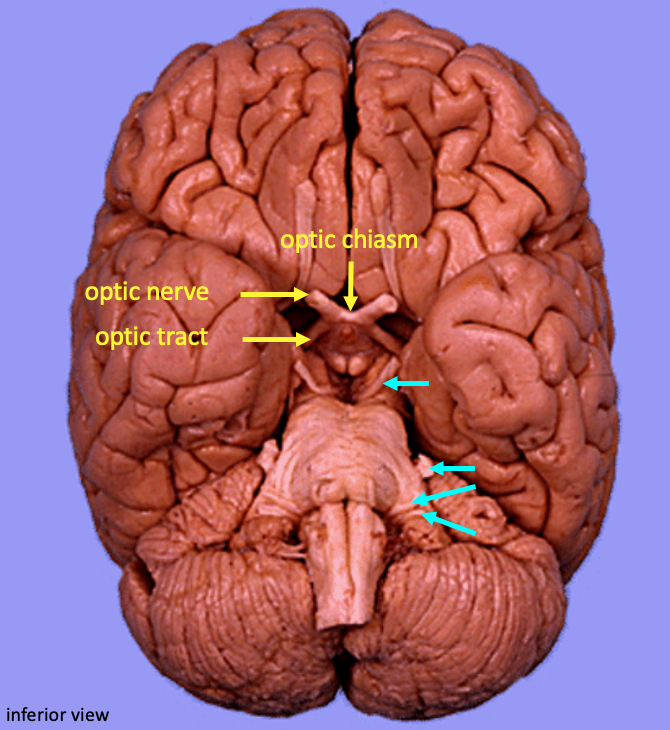
Visual information is detected and processed in the retina at the back of the eye. This information travels into the brain via the optic nerve, which contains the axons of the retinal ganglion cells. Cranial nerves are numbered with Roman numerals; the optic nerve is cranial nerve II. In a location just anterior to the pituitary gland and ventral to the hypothalamus, some of these axons cross over to the opposite side. The place where the axons cross (the center of the X) is called the optic chiasm. (The sectioned optic chiasm is visible in the midsagittal view of the brain.) The bundle of axons that extends from the optic chiasm to the thalamus is called the optic tract. These structures are labeled below in the inferior view of the brain.
This figure illustrates the pattern of axonal projections in the visual pathways.
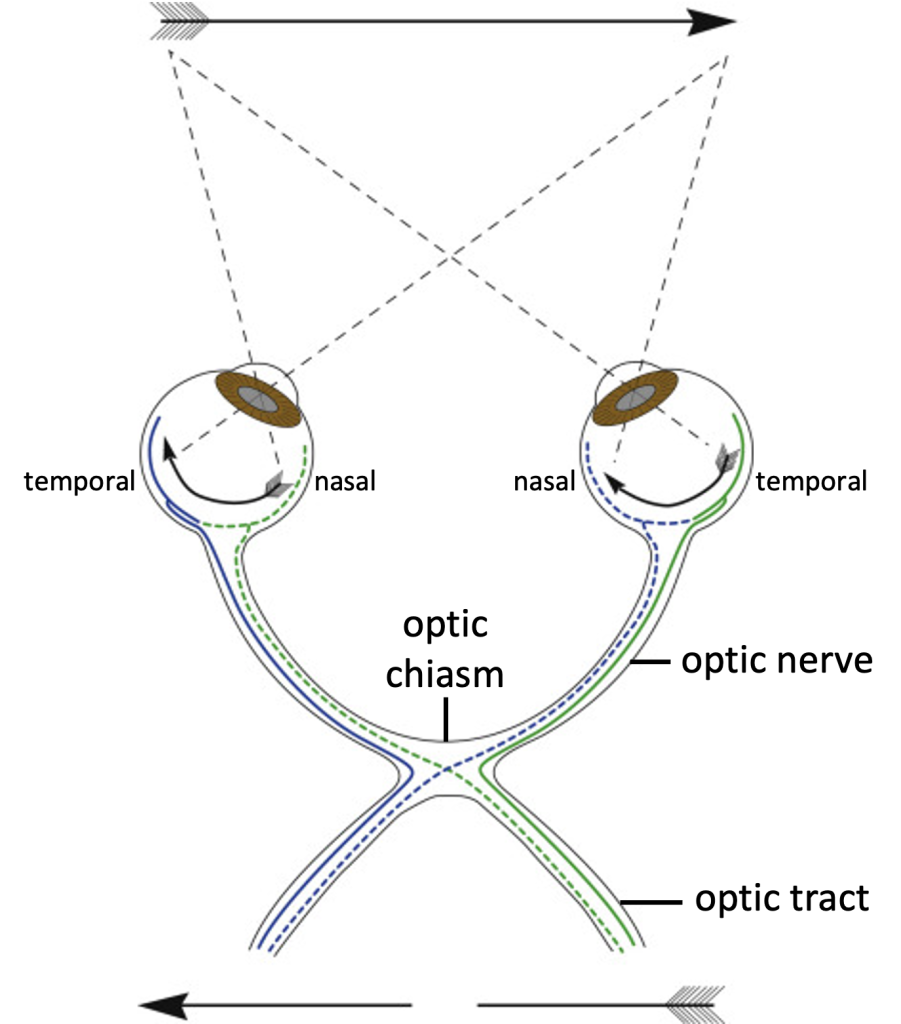
The retina can be divided into two halves: a nasal half that is on the medial side, closest to the nose, and a temporal half that is on the lateral side closest to the temporal bone. The nasal part of the retina”looks at”, in other words, encodes visual information from the outer part of the visual field, while the temporal part encodes visual information from the inner part of the visual field. The right temporal retina and the left nasal retina encode visual information from the left visual field (green lines in the drawing). Axons from each nasal retina (dotted lines) cross over at the optic chiasma. The result is that the visual information from one side of the visual field will be encoded in the contra later (opposite side) optic tract.
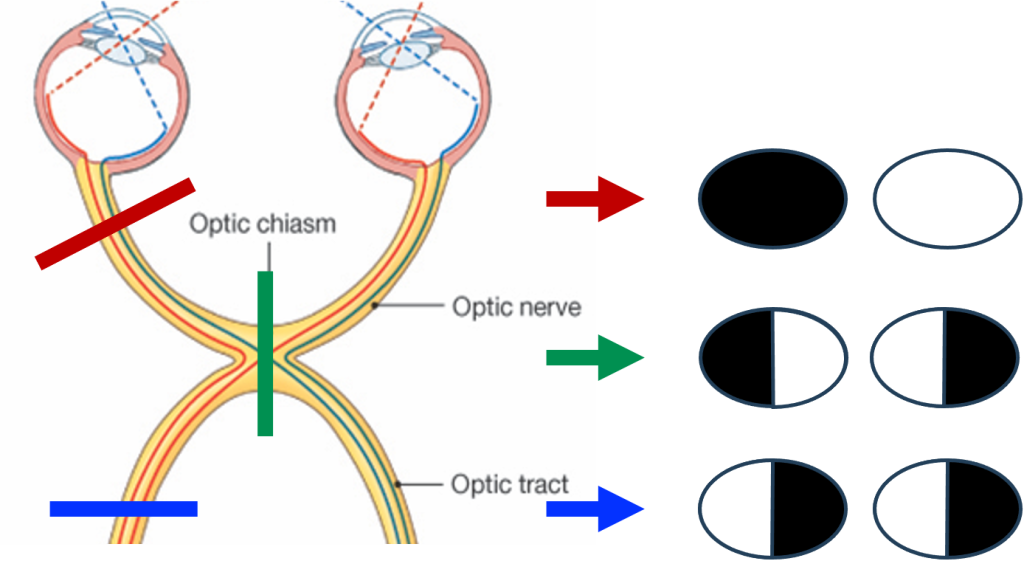
When a patient has a visual field defect, a neurologist will use their knowledge of this anatomy to determine where the lesion might be located. The figure below summarizes the visual deficits that arise from a lesion in the optic nerve, optic chiasm and optic tract.
Motor Pathways
The primary motor cortex is located in the precentral gyrus. This region of the brain contains neurons that are involved in initiating voluntary movements. A key feature about this region (and the adjacent primary somatosensory cortex in the postcentral gyrus) is that neurons are organized somatotopically. This means that neurons that control muscles in adjacent parts of the body are next to each other in the primary motor cortex. Essentially, there is a map of the body in the brain.
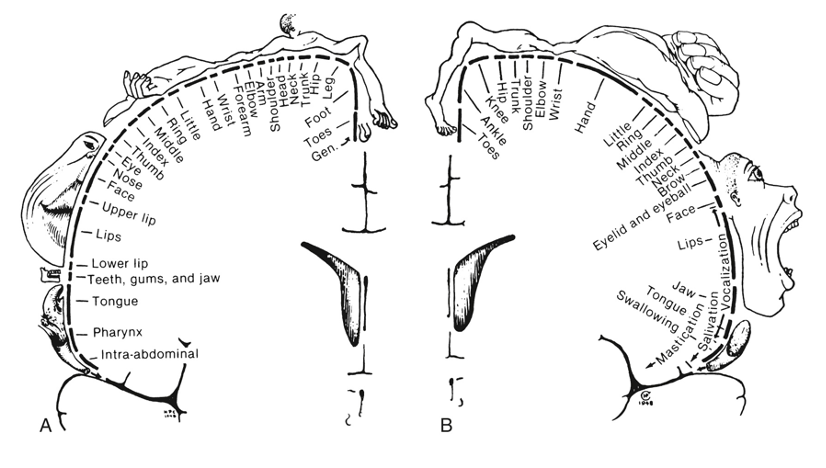
As shown in figure above, regions of the body with more fine motor control (such as the hand) have a higher degree of representation in the motor cortex.
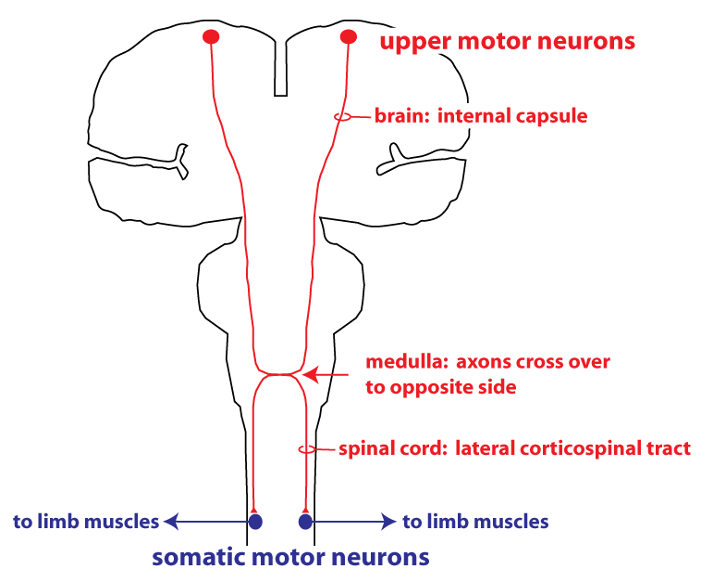
The neurons whose cell bodies are located in the primary motor cortex are some of the largest neurons in the body. The axons of these neurons extend down to the spinal cord where they make direct synaptic connections with somatic motor neurons, which are the cells that directly innervate skeletal muscles. A clinical term for these cells in the motor cortex is upper motor neurons (with the somatic motor neurons being the lower motor neurons). Another name for these cells is pyramidal neurons, because their axons cross in a structure on the ventral surface of the medulla known as the pyramids.
The axon bundle containing the axons of the upper motor neurons is termed the corticospinal tract. Axons in the first part of the corticospinal tract are found in a region of white matter called the internal capsule. Most of the axons (particularly those that project to somatic motor neurons innervating the limbs) cross over to the opposite side of the body at the medulla oblongata, and then continue in the spinal cord in the lateral corticospinal tract. The figure below is a schematic showing this pathway of connection from the motor cortex to skeletal muscle.
Upper Motor Neuron Disorders
Damage to neurons of the corticospinal tract is known clinically as an upper motor neuron disorder. An upper motor neuron disorder will affect motor control in different ways, depending on the location of the damage. A stroke that causes a lesion in the primary motor cortex or internal capsule affects motor function on the opposite (contralateral) side of the body. Damage to the lateral spinal cord (a lesion in the lateral corticospinal tract) will cause a motor defect in the limbs on the same (ipsilateral) side of the body.
Damage to the upper motor neurons causes two kinds of effects. The predominant effect initially is a loss of motor function, either paralysis or muscle weakness. These changes result from loss of excitatory input to the somatic motor neurons, and are termed negative signs. However some of the axons that descend in the corticospinal tract provide inhibitory input to neurons in the spinal cord, and loss of this input leads to abnormal increases in certain motor behaviors, or positive signs. An example of a positive sign is exaggerated reflexes (hyperreflexia). Another positive sign is an increase in stiffness, or muscle tone (hypertonia). Muscle tone is defined as the resistance of the muscle to passive stretch.
NOTE: Optional
The material in the following section will not be tested on the quiz section test. We will discuss Parkinson’s disease in the lectures about motor control later in the quarter.
Parkinson’s Disease
Parkinson’s disease is a neurodegenerative disease affecting the basal ganglia, which have a complicated role in the modulation of movement. The disease is diagnosed by observing a set of characteristic symptoms: resting tremor, bradykinesia, and hypertonia.
- Resting tremor is an oscillating movement that occurs when the patient is trying to be still. The tremor usually disappears when the patient undertakes a voluntary movement with the limb. This distinguishes it from other disorders involving tremor in which the tremor persists during movement (essential tremor) or is specifically associated with movement (intention tremor in cerebellar disorders).
- Bradykinesia means slowness of movement. The patient might initially experience bradykinesia as a weakness or stiffness in one limb.
- Hypertonia (excessive muscle tone) also occurs in Parkinson’s disease. This will manifest itself as rigidity or stiffness.
Other typical features seen as the disease progresses are a stooped posture and slow, shuffling gait. As it becomes more and more difficult to initiate movement, the patient will start to show akinesia, or a lack of movement. Lack of movement of the facial muscles gives the patient the appearance of having a mask-like, frozen look.
For many patients, the initial presentation is asymmetric, meaning only one limb or one side of the body is affected. This is what is illustrated in the video clip, from a clinical practice article in the New England Journal of Medicine (Nutt JG and Wooten GF. Diagnosis and Initial Management of Parkinson’s Disease. N Engl J Med 2005;353(10):1021-7).
The second video clip shows a patient in whom the disease is much more advanced. The patient has a strong resting tremor in the arms, and a stooped posture. Akinesia manifests as “freezing of gait”, in which the patient has great difficulty in taking a step forward. Amazingly, the second part of the video shows the patient is still able to ride a bicycle. (Snijders, A. H. and Bloem, B. R. Cycling for Freezing of Gait. N Engl J Med 2010;362: e46).
Neurodegeneration in Parkinson’s Disease
Parkinson’s disease is caused by a degeneration of neurons in the substantia nigra of the midbrain. Substantia nigra means “black substance, and it is easily reconizable as the pigmented region that stretches across the midbrain in a frontal section of the brain. These neurons form connections with nuclei in the basal ganglia and release the neurotransmitter dopamine. Parkinson’s disease is considered a disorder of the basal ganglia because the major projection from the substantia nigra is to nuclei of the basal ganglia[1].
The schematic below provides a simplified illustration of the connectivity of the basal ganglia.
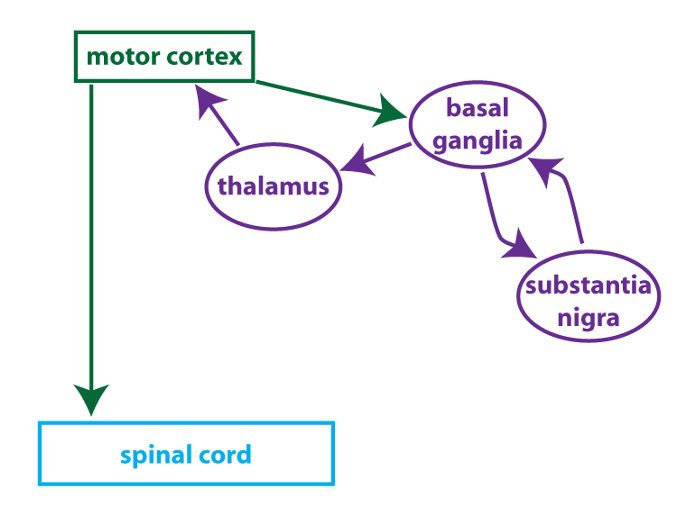
The basal ganglia receive inputs from the motor cortex (and other brain regions), and then project back to the motor cortex via the thalamus. The substantia nigra is interconnected with nuclei in the basal ganglia. The basal ganglia integrate these multiple inputs to modulate the output of the motor cortex. Some of the connections are excitatory and some are inhibitory. The loss of input from dopamine-releasing neurons in the substantia nigra alters the balance of the output from the basal ganglia to the motor cortex, and this underlies the symptoms that are seen.
Parkinson’s disease can be treated by restoring the dopamine that is lost from the basal ganglia when neurons from the substantia nigra degenerate. Dopamine itself cannot be used because it doesn’t cross the blood-brain barrier. Instead, patients are treated with L-DOPA (also known as levodopa), a dopamine precursor that can cross the blood-brain barrier.
OPTIONAL
This video shows the effectiveness of a treatment for Parkinson’s disease called deep brain stimulation (DBS). DBS changes the activity of neurons in the basal ganglia circuitry in ways that are not fully understood. The treatment doesn’t work for all Parkinson’s patients, but for some individuals, DBS can have a profound effect on symptoms.
- **Wikipedia (and perhaps some other sources) define the basal ganglia as "subcortical nuclei", a definition that allows the substantia nigra to be lumped in with the cerebral nuclei of the basal ganglia. For our purposes, the basal ganglia consist of the three nuclei (caudate, putamen, globus pallidus--you don't need to know the specific names) located deep in the cerebrum. Functionally speaking, the substantia nigra is part of the basal ganglia circuitry; but anatomically speaking, it is a distinct nucleus located in the midbrain. ↵
