Epithelia
SESSION OBJECTIVES
- Recognize and describe the histological types, structural characteristics, and functions of epithelia.
- Describe the structural features of a typical epithelium, and some specializations of epithelial cells and epithelial tissues.
- Know the types and locations of cell junctions and what they do.
- Understand how epithelia are renewed by cell division.
- Describe how epithelia can organize into glands, the types of secretion exhibited and the structural arrangements of glands.
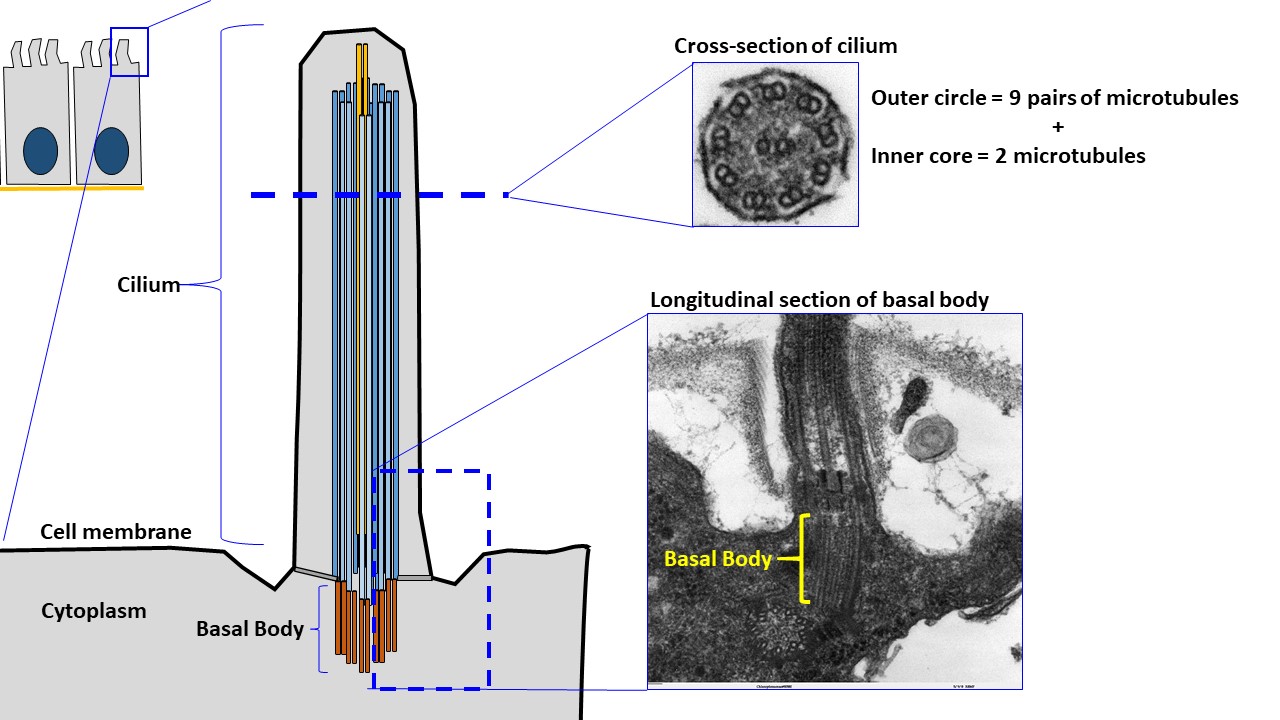
- Identify the ultrastructural components of a cilia including basal bodies and identify the motor protein that creates movement of these structures.
- Relate the importance of transcellular (vectorial) transport, distinguishing features on the apical, basal surfaces of a cell, and the necessity of tight junctions in eliminating paracellular transport in establishing gradients across an epithelial membrane.
OPTIONAL PRE-CLASS MATERIALS FOR THIS SESSION:
- Skim the section titles, bolded terms, and image captions from Junqueira’s Basic Histology, Chapter 4 (Click here for FMR library resources) to fill in any knowledge gaps you need.
OVERVIEW:
Like other tissue types, epithelia are aggregations of functionally associated cells. An epithelium is classified according to the shape of the cells at its free surface and also by the number and arrangement of layers. Epithelia display a remarkable range of applications and adaptations. An epithelium can form sheets or tubes when covering a free surface, or solid cords or a system of branching tubules. Frequently, the key to identifying a tissue or an organ is to recognize the types of epithelia present.
Before we begin, recognize the difference between terms:
Epithelia (noun, singular = epithelium) line all external and internal surfaces of the body.
Epithelial (adjective) cells are the specialized, individual cells tightly attached to their epithelial cell neighbors and basement membrane to form a continuous sheet of epithelium.
Tip: ALWAYS base your identification of epithelia on the layer of cells closet to the surface (luminal aspect) of the epithelium.
GENERAL CHARACTERISTICS (Session Objectives #1, #2, #6)
- FUNCTIONS OF EPITHELIA
Epithelia serve numerous functions
- PROTECTION: Tough, flexible, mechanical and microbial barriers (epidermis, oral epithelium, vagina), chemical barriers (urinary tract), and vapor barriers (epidermis).
- TRANSPORT: Mucus and particulate materials are removed (e.g., the respiratory tract) and cells are propelled through tracts (e.g., sperm or eggs in the uterine tube, uterus, efferent ductules) by ciliary action.
- SECRETION: Ions are actively moved (pumping); synthesized materials are released by merocrine (granule exocytosis), apocrine (apical cytoplasm loss), and holocrine (whole cell) secretion. Many of the cells thought to secrete via an apocrine mechanism are now considered to be merocrine.
- Pumping is energy-dependent (requires mitochondrial ATP), is directional (maintains ionic gradients), and requires a tightly sealed epithelium. It may be involved in either secretion (e.g., sweat glands) or absorption (e.g., gall bladder).
- Exocytosis occurs in both exocrine and endocrine cells and is the method most often used by cells to secrete stored materials. Local hormone release or nerve stimuli may trigger exocytosis.
- ABSORPTION: Cells take up materials such as gases (alveolar epithelium in lungs), nutrients (gut epithelium), and sugars (proximal convoluted tubules in the kidney) through endocytosis.
- LUBRICATION: Fluid or mucus is secreted onto the surface of the epithelium to minimize friction (e.g., the mesothelium lining body cavities) or to prevent abrasion (the lining of the gut).
- SENSORY RECEPTION: Epithelial cells can develop into sensory receptors (e.g., taste buds, olfactory epithelium, vestibular cells).
- STRUCTURAL FEATURES OF EPITHELIA
- Epithelia are derived from all three layers of the embryo (ectoderm, mesoderm and endoderm).
- Epithelial cells possess a cytoskeleton comprised of microfilaments, intermediate filaments and microtubules.
- Epithelial cells are anchored to a sheet of extracellular matrix components (basal lamina) to form sheets of cells.
- Specialized junctions attach epithelial cells to each other. Collectively, these different types of junctions form a junctional complex between epithelial cells. Because of these junctions and attachment to basal lamina, epithelial cells can form tissue compartments and the cells themselves can be polarized (luminal/apical vs baso/lateral).
- Epithelial cells often display luminal features that relate to specific functions (microvilli and stereocilia, motile cilia,).
- Epithelial cells are separated from the blood supply by this basal lamina and are dependent on the connective tissue for metabolic exchange (diffusion).
- Basal lamina is composed of collagens (types IV and VII), proteoglycans and other extracellular proteins produced by epithelial cells and underlying connective tissue.
- Polarity of Epithelial Cells:
- Epithelial cells have polarity so that their basal surface is anchored to the basement membrane (an extracellular structure composed of specialized proteins, including Type IV, Type III, and Type VII collagen proteins and laminin) that anchors cells to the underlying connective tissue of the epithelium.
- Ultrastructure of the basement membrane using TEM reveals two layers:
- Basal lamina (collagen Type IV and laminin)
- Reticular lamina (collagen Type III and VII)
- Ultrastructure of the basement membrane using TEM reveals two layers:
- Epithelial cells have polarity so that their basal surface is anchored to the basement membrane (an extracellular structure composed of specialized proteins, including Type IV, Type III, and Type VII collagen proteins and laminin) that anchors cells to the underlying connective tissue of the epithelium.
-
-
-
- Functions of the basement membrane include:
- Provide an attachment for epithelial cells to underlying connective tissue;
- Regulate and filter substances passing from connective tissue into epithelial cells and vice versa;
- Provide a basic structure of the epithelia during tissue regeneration following injury to build on;
- Separate epithelia from other tissues.
- Functions of the basement membrane include:
- Epithelial cells also have an apical surface facing a free surface (e.g. the surface of the skin or the lumen of the gut tube).
- Specializations include:
- Microvili:
- Structure: Cell membrane processes with an actin filament at its core, non-motile.
- Function: Increase the cell’s surface area for absorption of luminal contents (e.g. gut tube luminal contents).
- Stereocilia:
- Structure: Resemble long microvili with actin core, non-motile
- Function: A mechanosensory function in certain cells (e.g. hair cells of the ear); absorption function in the epididymis.
- Cilia (singular = cilium):
- Structure: Cell membrane processes with a core of 9+2 arrangement of microtubules (called an axoneme) anchored to the apical cytoskeleton in the cytoplasm of the cell by a basal body (see image below). Axonemal dynein binds one doublet microtubule in each pair to bend the axoneme and produce a beating motion of the whole cilium.
- Function: Propel substances (e.g. mucus) along an epithelial surface.
- Microvili:
- Specializations include:
-
-
-
-
-
- Destruction of apical specializations can have serious consequences and cause disease:
- Celiac disease: Loss of microvilli (destruction of the brush/striated border) results in decreased absorption in the small intestine.
- Cystic fibrosis: Increased mucus production results in cilia dysfunctions and decreased muco-ciliary clearance in the respiratory tract.
- Destruction of apical specializations can have serious consequences and cause disease:
-
-
- MORPHOLOGY OF EPITHELIA
There are several different types of epithelium based on morphology:
-
- Simple squamous (Click this link for an example)
- Simple cuboidal (Click this link for an example)
- Simple columnar (Click this link for an example)
- Pseudostratified (Click this link for an example)
- Stratified cuboidal (Click this link for an example)
- Stratified columnar
- Transitional (aka Urothelium) (RELAXED=Bladder empty: Click this link for an example); (STRETCHED = Bladder full: Click this link for an example);
- Stratified squamous cornified or non-cornified (Click this link for an example)
Knowledge check: Drag the text box and drop it over the correct micrograph of that type of epithelia in the activity below.
A note on terminology: Sometimes “keratinized/non-keratinized” are terms used to describe cornified and non-cornified epithelium. The term refers to the presence or absence of a layer of non-nucleated remains of terminally differentiated epithelial cells (stratum corneum). Since all epithelial cells use keratins as intermediate filaments, the term non-keratinized epithelium is inaccurate. We will practice recognizing cornified and non-cornified epithelia again in the skin histology session in the Invaders and Defenders Block.
There is a close relationship between the structure of an epithelium and its function. Different epithelia may therefore display unique features related to their specialized function:
- Simple epithelia may secrete, absorb, resorb, dialyze, and/or filter.
- Pseudostratified epithelia engage in secretion, ciliary transport and sensory reception.
- Stratified epithelia serve primarily protective functions.
Epithelial cells have unique specializations to support these different functions, typically on their apical cell surface.
EPITHELIAL CELL JUNCTIONS (Session Objective #3)
-
- Cell-Cell junctions include:
- Tight (aka occluding) junctions:
- Location: Apical cell membrane.
- Structure: Formed by claudin and occludin transmembrane proteins and actin filaments.
- Function: Separate apical from basal cell membrane regions; Prevent passage of substances between cells (paracellular transport).
- Adherens (aka belt) junctions:
- Location: Lateral cell membrane
- Structure: Formed by E-cadherin and β-catenin complexes and actin filaments.
- Function: Links cytoskeletons of adjacent cells; strengthens and stabilizes adjacent tight junctions.
- Location: Lateral cell membrane
- Tight (aka occluding) junctions:
-
- Gap junctions:
- Location: Lateral cell membrane
- Structure: Formed by connexins, no cytoskeletal filaments.
- Function: Allows for direct transfer of ions/small molecules between cells.
- Gap junctions:
-
- Desmosome (aka macula adherens):
- Location: Lateral cell membrane
- Structure: Formed by cadherins, desmogleins and intermediate filaments (specifically, keratins!)
- Function: Connects cells’ cytoskeletal elements together via strong attachments to strengthen the cohesion of a tissue.
- Desmosome (aka macula adherens):
- Cell-Matrix junctions include:
- Hemidesmosome
- Location: Basal cell membrane
- Structure: Formed by integrins and intermediate filaments.
- Function: Anchors cell cytoskeleton to basal lamina.
- Hemidesmosome
-
- Focal Adhesions (aka focal contact)
- Location: Basal cell membrane
- Structure: Formed by integrins and actin filaments.
- Function: Anchors cell to basement membrane during moving (e.g. epithelial repair) and in cell mobility.
- Focal Adhesions (aka focal contact)
Knowledge check: Match each type of cell junction to its respective location on the cell by dragging the term on the right and dropping the term on the structure indicated by the arrows on the image:
Case 1:
TRANSPORT ACROSS EPITHELIA (Session Objective #7)
Epithelial cell junctions regulate what and how certain molecules/ions/etc. can cross epithelia via:
- Paracellular transport, mentioned above and regulated by tight junctions, is the (often prevention of) movement of substances between cells. This type of transport allows for a gradient to be maintained within a tissue and a lumen. It also allows for strict maintenance of setting up barriers to certain substances from crossing epithelia (e.g. the blood-brain barrier).
- Transcellular transport is the transfer of molecules, ions, and water across the cell membrane (so through the cell itself).
The directional movement of substances across epithelia can be described in two ways:
- Absorption is the transport of substances from the epithelial cell’s apical surface toward the basolateral cell surface and across the basement membrane into the tissues (often blood) deep to the epithelium.
- Secretion is the transport of substances from a tissue/organ/or the epithelium itself from the basolateral surface of the cell to the apical surface of the epithelium.
Knowledge check:
EPITHELIAL REPLACEMENT AND REPAIR (Session Objective #4)
Epithelia are subject to wear and require cell renewal. The replacement of lost cells occurs by division of remaining cells, i.e. stem cells and transit amplifying cells and is dependent on contact with the basal lamina. Replacement may be rapid (e.g., the intestinal lining is replaced about every five to six days) or very slow (e.g., the respiratory epithelium, mesothelium, and most glands show little cell division). Alteration of normal proliferative activity may lead to changes such as regression (thinning or loss of continuity), metaplasia (transformation of one type of tissue into another), or neoplasia (formation of a new cell type with loss of normal control mechanisms that regulate proliferation).
Proliferation of epithelial cells is usually restricted to distinct tissue compartments. Simple epithelial cells are renewed by cell divisions of stem cells, which are scattered throughout the sheet of cells. Stratified epithelial cells are continually lost from the free surface and are renewed by proliferation of stem cells and transit amplifying cells in the basal layer. As the cells move upward from the basal layer, they become more mature and specialized to provide specific protective functions.
GLANDS (Session Objective #5)
- Glands are formed during development by epithelium that invade the underlying connective tissue. Exocrine glands retain a connection to the surface. Endocrine glands eventually lose their connection to the surface epithelium.
EXOCRINE GLANDS
-
- Exocrine glands are classified by their mechanism of secretion onto the surface epithelium:
- Merocrine (exocytosis of granules into a lumen),
- Apocrine (pinching off of apical cytoplasm that contains product), or
- Holocrine (shedding of the whole cell).
- Exocrine glands are also classified by the nature of their secretion:
- mucous (viscous),
- serous (protein-rich fluid), or
- mixed (both mucous- and serous-type cells are present)
- Exocrine glands can also be classified according to the morphology of their secretory portions and duct system:
- tubular
- tubulo-alveolar (alveolar=round)
- one single duct (aka simple) or
- branching ducts (aka compound) to drain the glandular tissue.
- Exocrine glands are classified by their mechanism of secretion onto the surface epithelium:
ENDOCRINE GLANDS
-
- Endocrine glands have lost their connection to their original epithelium and so don’t have ducts.

Knowledge check:
HISTOLOGY ATLAS AND PRACTICE EXERCISES
SIMPLE SQUAMOUS & SIMPLE CUBOIDAL EPITHELIUM
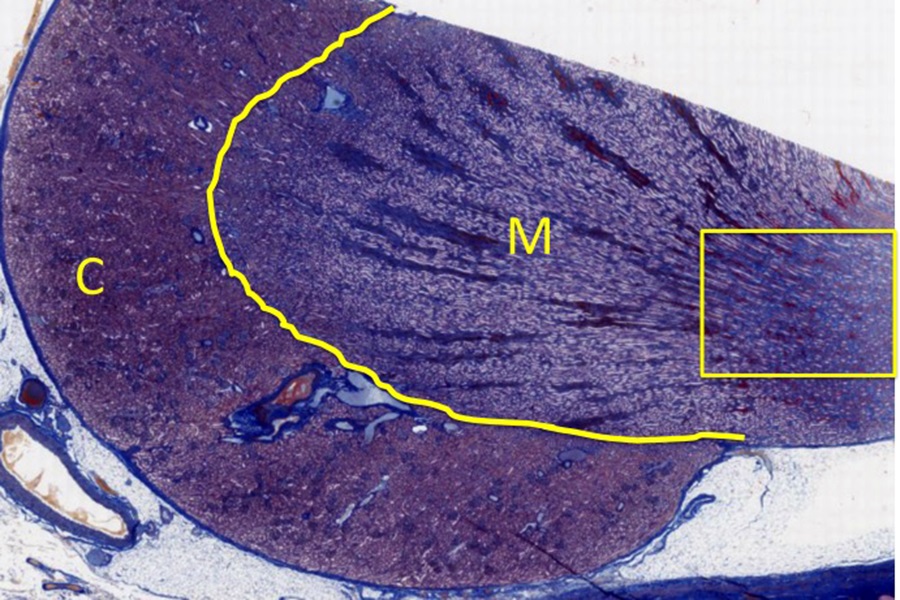
Slide 1: Kidney : Below is a low-magnification Trichrome-stained micrograph of a kidney section. The kidney has an outer cortex (C) and inner medulla (M).
In the region indicated by the yellow box on the image below we will examine samples of simple squamous epithelium and simple cuboidal/columnar epithelium.
- Stain Information: Trichrome:
- Blue = Collagen& extracellular matrix
- Red = Nuclei
- Light Purple = cell cytoplasm
- Orange/Red = erythrocytes
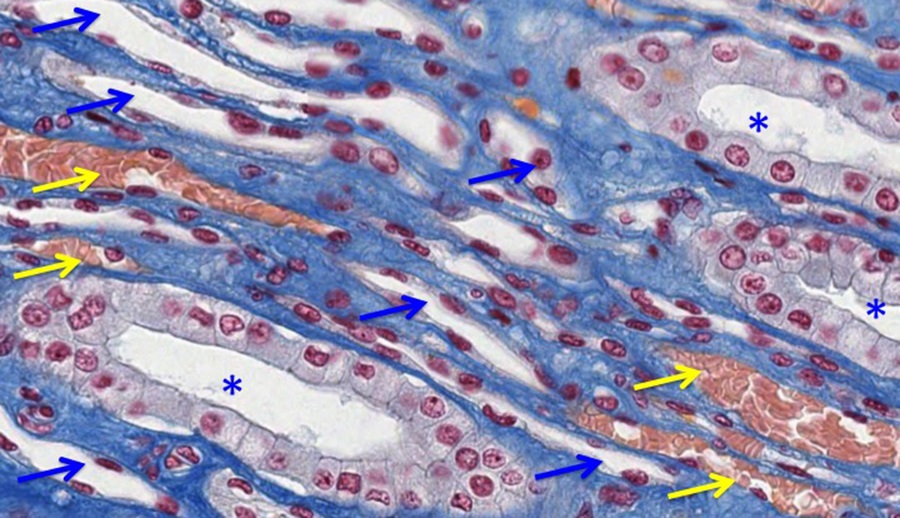
In this portion of the kidney there are many collecting ducts (CD, blue asterisks in image above) that are lined with simple cuboidal/columnar epithelium. The epithelium of the CD’s are actively transporting ions and water. There are also portions of the nephrons that are delicate tubes lined by simple squamous epithelium (blue arrow) and blood vessels (containing eosinophilic erythrocytes; yellow arrows) The squamous epithelium lining portions of the nephrons and blood vessels effectively let molecules diffuse through their thin cytoplasmic processes.
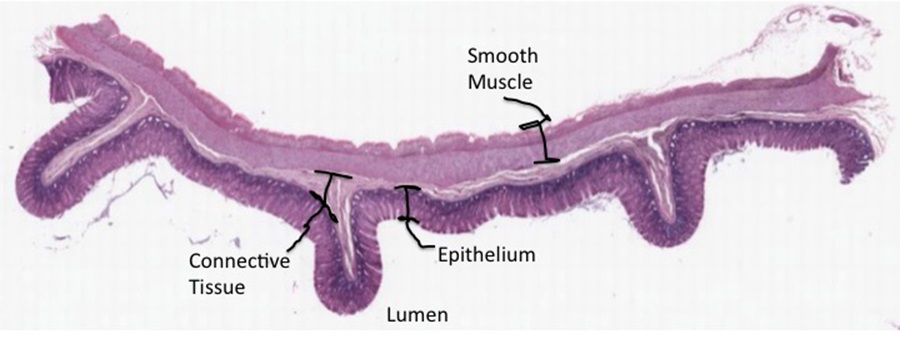
SIMPLE COLUMNAR EPITHELIUM
Slide 2: Colon: At low magnification, the density of the epithelial nuclei in the section of the gut tube below renders the epithelial layer dark (recall this is called basophilia because the nucleic acids have an affinity for basic dyes like hematoxylin).
- Stain Information: Hematoxylin & Eosin:
- Pink/light purple = Cellular and extracellular proteins
- Dark purple/blue = Nuclei
- Very pale blue = Mucus
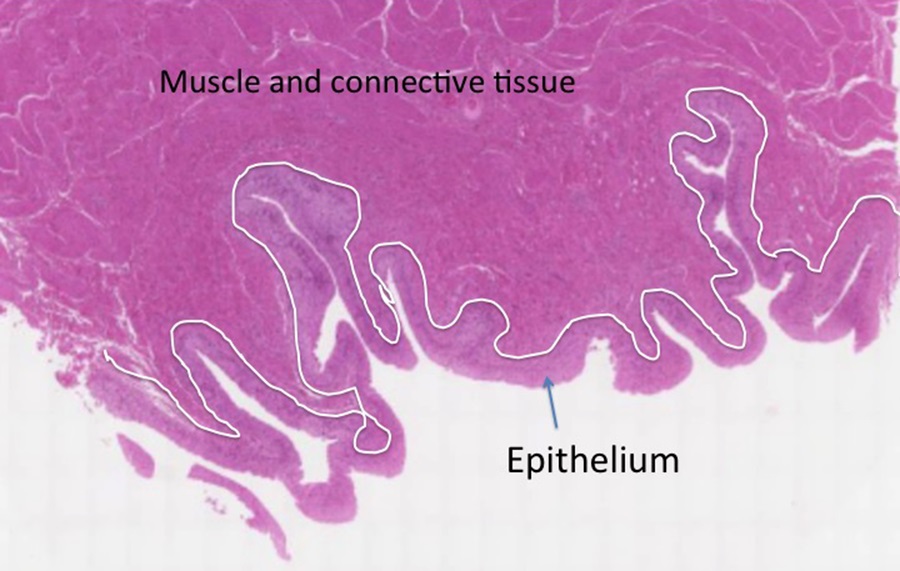
The boundary epithelium of the gut tube is simple columnar epithelium that lines the lumen of the tube, with concentric layers of connective tissue and smooth muscle forming the wall of the gut tube.

With intermediate magnification, the organization of the epithelium as a series of invaginations is evident. Some of the individual tubes of epithelium that open onto the gut lumen (L) are outlined in yellow. There is a thin layer of connective tissue that surrounds each tube. This image also illustrates the complexity of interpreting three- dimensional structures from two-dimensional images. Due to the orientation of the section relative to the position of the epithelial tube, many different profiles can be observed.
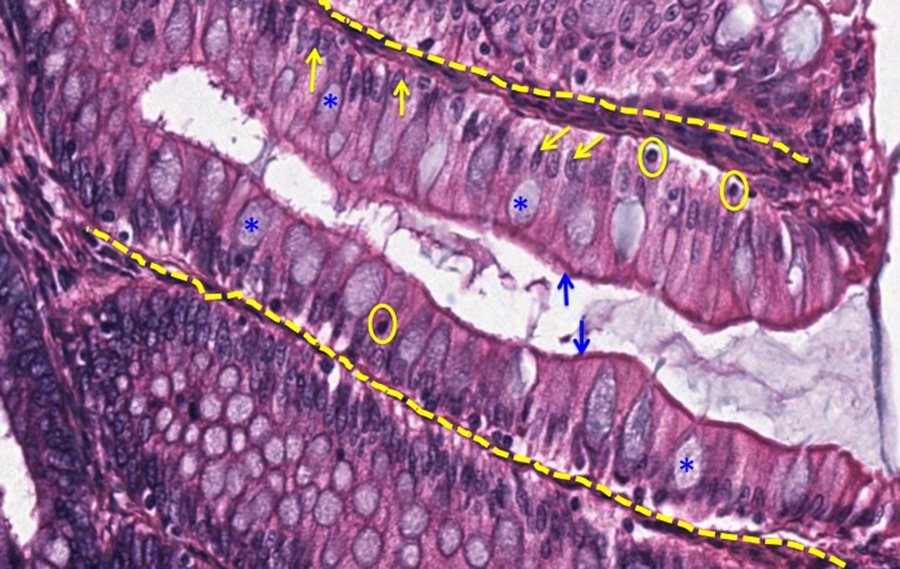
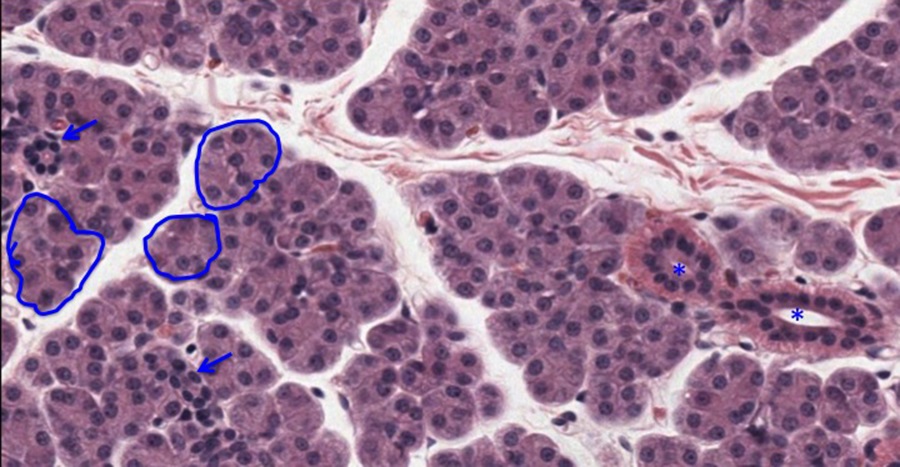
At high magnification, the simple columnar epithelial cells are visible as a single layer of epithelial cells that are taller than they are wide. They have a luminal specialization, microvilli. These small projections can sometimes be seen at the light microscopic level as a band of more intense staining along the luminal aspect of the epithelial cells (referred to as the terminal web)
indicated here by blue arrows. The basal location of epithelial nuclei is indicated by yellow arrows. There are also scattered round nuclei that are stained very intensely (a few are enclosed by yellow circles). They are lymphocytes (white blood cells) that have infiltrated the epithelium. More on these cells later. Within the epithelial layer are scattered cells that produce
mucus. These mucus-producing epithelial cells are called goblet cells and several are indicated by blue asterisks. Mucus produced by these cells accumulates in the gut lumen and can sometimes be seen in histological specimens. In this preparation, the mucus in the goblet cells and in the gut lumen is faintly basophilic. In many preparations, the mucus is not stained. More on this later. The invaginations of epithelium seen above are called crypts. The crypts are embedded in connective tissue (indicated by dashed yellow lines), which will be considered later. The crypts of epithelium in the colon can be considered as simple straight exocrine glands that secrete mucus.
NON-CORNIFIED STRATIFIED SQUAMOUS AND CILIATED PSEUDOSTRATIFIED COLUMNAR
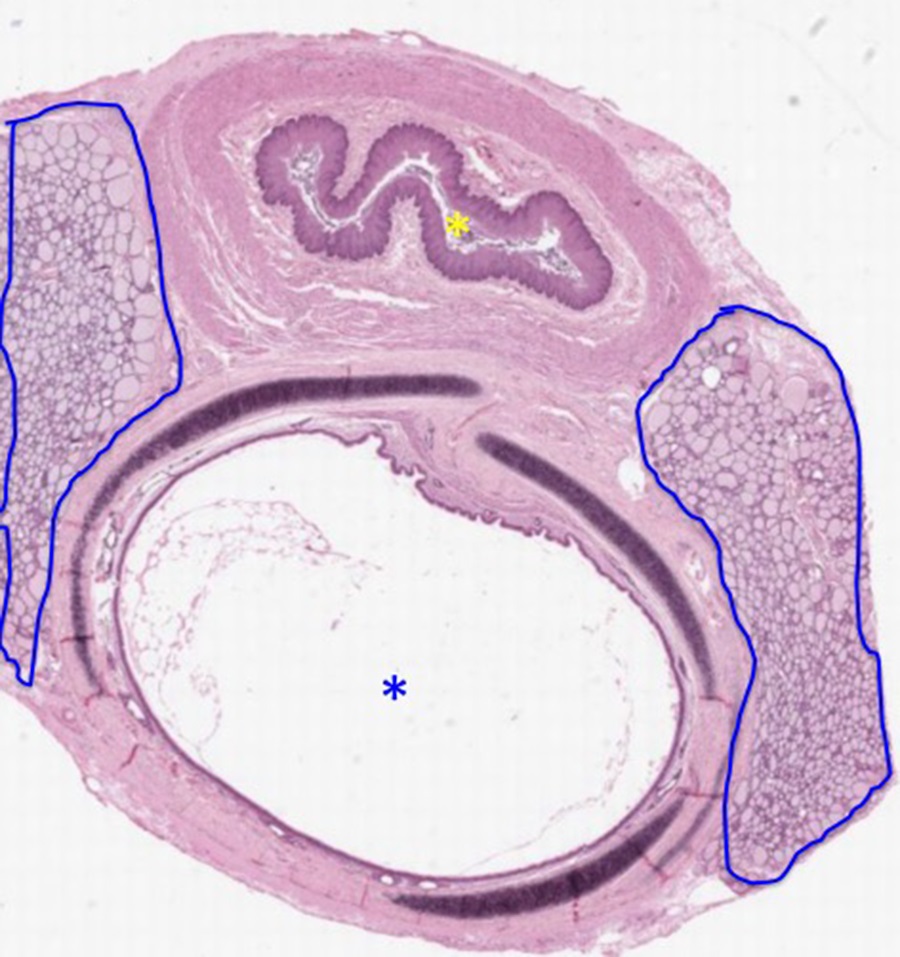
Slide 3: Trachea and esophagus : Low magnification of a light micrograph of the trachea (blue asterisk) and esophagus (yellow asterisk) below:
- Stain Information: Hematoxylin & Eosin:
- Pink/light purple = Cellular and extracellular proteins
- Dark purple/blue = Nuclei
- Very pale blue = Mucus
- Very dark blue/black = Cartilage
These two adjacent structures are lined by different types of boundary epithelium. The esophagus has an irregular profile and the lumen is indicated by a yellow asterisk, while the lumen of the trachea (blue asterisk) is maintained by rings of cartilage (very dark thin structures). Laterally on both sides are masses of thyroid tissue outlined in blue.
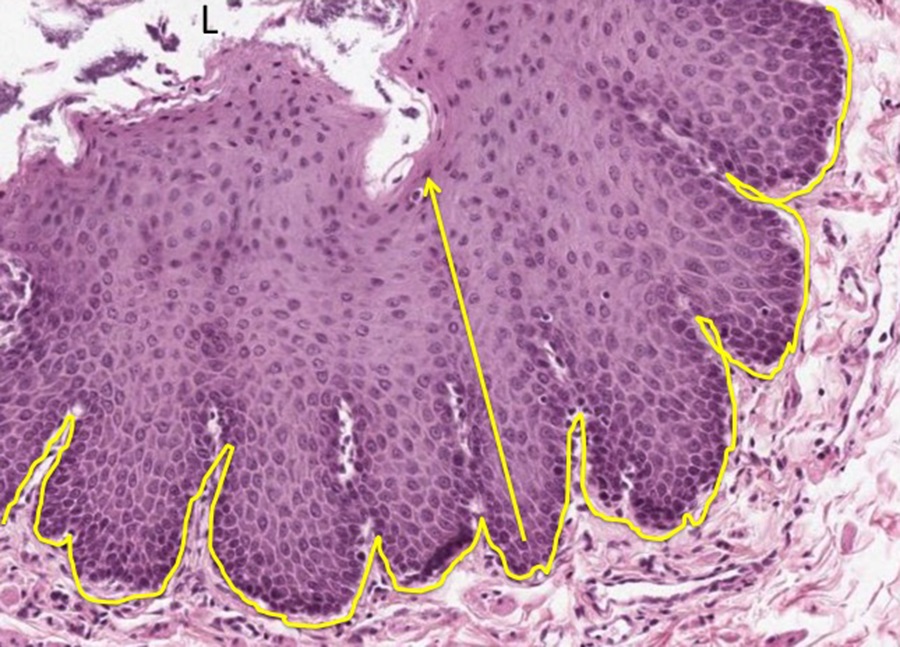
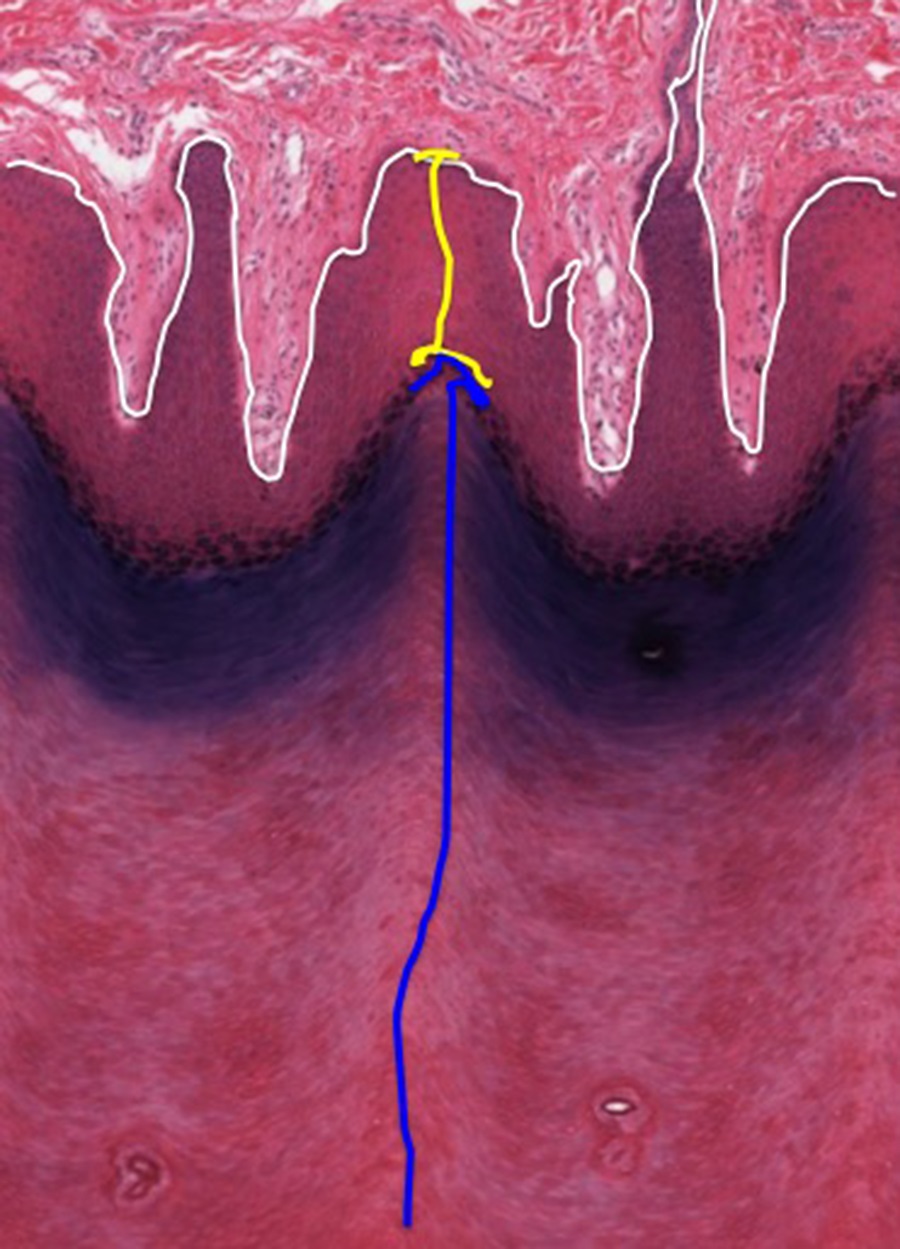
The epithelium lining the esophagus is stratified (many layers), squamous (because the outer layers toward the lumen are flattened) and non-cornified (because there are nucleated epithelial cells along the luminal surface). Replacement of the epithelial cells occurs centripetally, as basal cells replace luminal cells that are sloughed off into the lumen(in the direction of the yellow arrow). The approximate location of the basement membrane separating the epithelium from the underlying connective tissue is indicated by the yellow line. This type of epithelium lines structures in moist/wet locations that require a degree of mechanical strength (esophagus, parts of oral cavity, vagina).
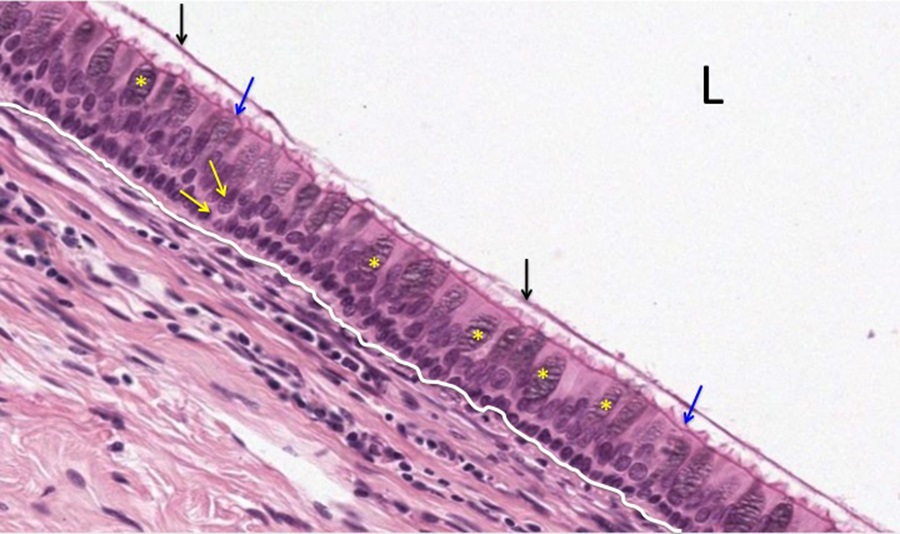
The epithelium of the trachea displays nuclei at multiple levels (indicated by yellow arrows). While this gives an appearance of stratified epithelium, all of the epithelial cells have contact with the underlying basement membrane (indicated by white line), hence the term pseudo-stratified. The luminal aspect of the epithelium is specialized and most of the cells express cilia (indicated by blue arrows. Scattered among the ciliated cells are mucus- producing cells/goblet cells (indicated by yellow asterisks). Mucus secreted by the goblet cells covers the epithelium (indicated by black arrow) and this “sheet” of mucus is moved by the action of the underlying cilia. Because this type of epithelium is so characteristic of some portions of the respiratory system, it is often referred to as “respiratory epithelium”. L= lumen.
TRANSITIONAL EPITHELIUM
Slide 4: Bladder :
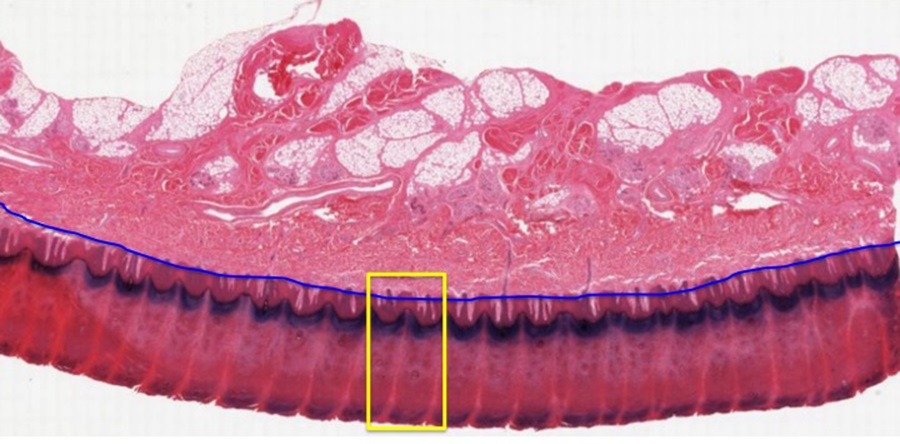
The bladder is a fibromuscular sac that is lined by a unique epithelium, termed transitional epithelium. The separation between epithelium and underlying connective tissue and muscle is indicated by a white line on the micrograph below:
- Stain Information: Plastic section stained with phyloxine -like eosin- and celestine blue -like hematoxylin:
- Compared to H&E, the “redness” is more intense and the basophilia is weaker

This epithelium has multiple layers of cells that are not all in contact with the basement membrane, and thus could be considered as stratified. However, this epithelium is classified as transitional because of the morphological changes that it undergoes in the bladder, depending on how full the bladder is with urine and how stretched the epithelium is as a consequence. When the bladder is relaxed, the luminal cells are some of the largest within the epithelial layer. A few are indicated by black arrows. Note that these cells possess nuclei. Termed “facet” or “pillow” cells, these cells flatten out dramatically when the bladder is distended with urine, so the epithelial layer “transitions” when stretched to look much more squamous. This type of epithelium lines much of the structures of the urinary system. Compare the appearance with that of non-cornified stratified squamous epithelium in other samples. E= epithelium
CORNIFIED STRATIFIED SQUAMOUS EPITHELIUM
Slide 5: Epidermis: Skin or integument consists of an epithelial covering (epidermis) and associated underlying connective tissue (dermis and hypodermis). This separation is indicated by the blue line in the micrograph below:
- Stain Information: Hematoxylin & Eosin:
- Pink/light purple = Cellular and extracellular proteins
- Dark purple/blue = Nuclei
- Very pale blue = Mucus
Focus on the region highlighted in yellow to see the cellular detail of the epidermis. This boundary epithelium consists of multiple layers of cells (stratified) and as moving from the basal region (separated from the dermis by a basement membrane approximated by the white line) to the luminal surface, the cells get flatter. The region of this epithelium that contains nucleated cells is indicated by the yellow bar. The outermost layer of nucleated cells contain cytoplasmic granules that have a brown color in this sample. The layer indicated by the blue bar consists of the remains of epithelial cells. Termed the stratum corneum, it consists of waxy, non-nucleated cell envelopes that form a water repellent mechanical barrier. The staining properties of the stratum corneum is highly variable-the basophilia exhibited by the stratum corneum is not a reproducible feature. An epithelium that possesses a stratum corneum is classified as cornified. Hence the distinction between cornified stratified squamous epithelium of the skin and the non-cornified stratified squamous epithelium of the esophagus or vagina.
- Exocrine gland
Slide 6: Parotid Gland: The parotid gland, the largest salivary gland in the body, is shown at low magnification in the micrograph below:
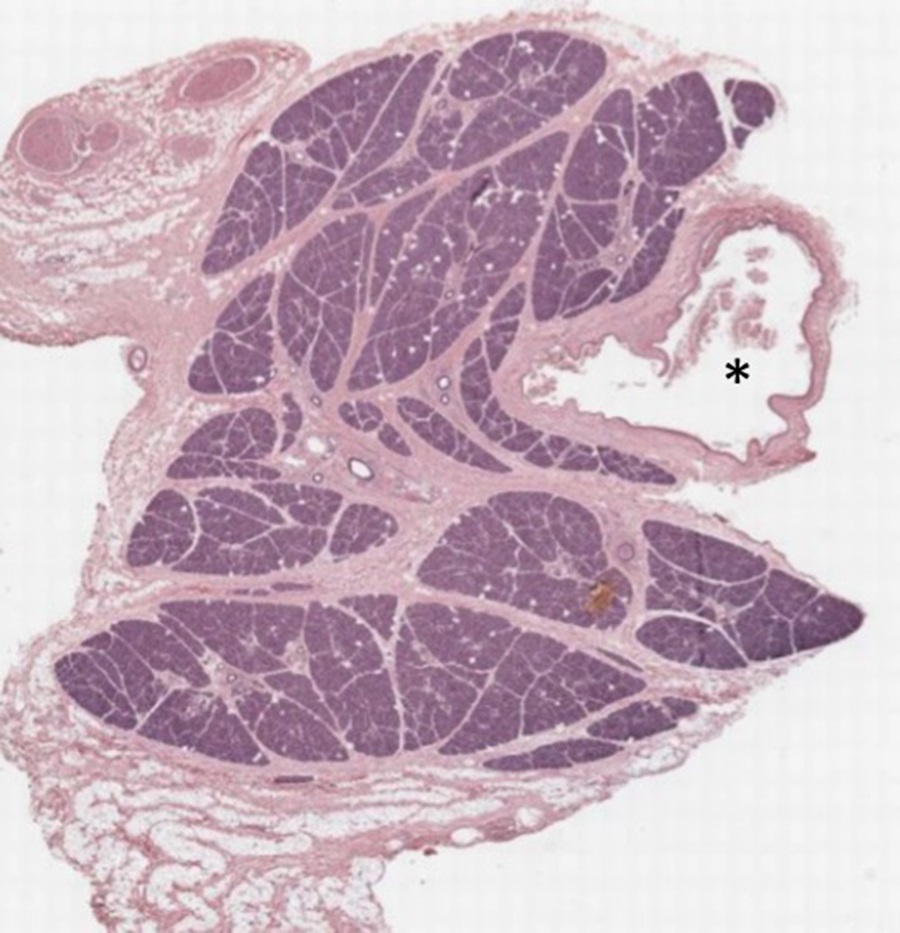
- Stain Information: Hematoxylin & Eosin:
- Pink/light purple = Cellular and extracellular proteins
- Dark purple/blue = Nuclei and cytoplasm rich in RNA
- Bright red = cytoplasm of erythrocytes
This sample demonstrates the organization of epithelium into secretory endpieces, acini. Collections of epithelial cells are separated by strands of connective tissue. The lumen of a large blood vessel (vein) is indicated by an asterisk in the image above.
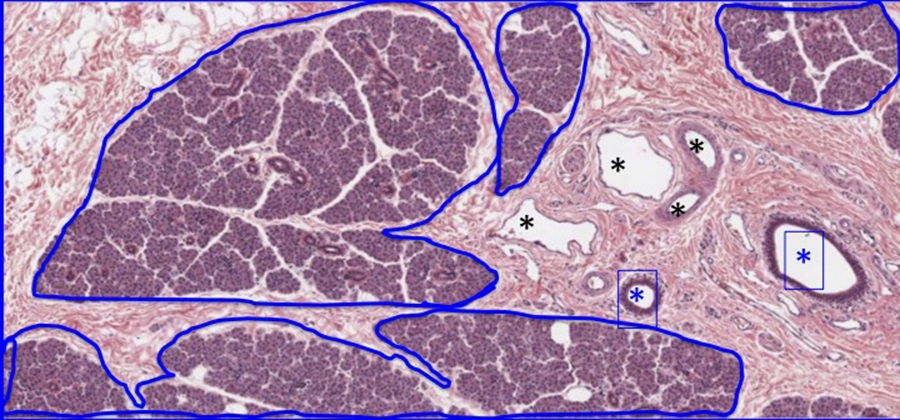
The parotid gland is a serous gland with a branched acinar organization. Lobules of serous acini encased in connective tissue are outlined above in blue. Blood vessels (black asterisks) and exocrine ducts (blue asterisks) are found within the connective tissue and are called interlobar ducts. They have a cuboidal epithelium that may be stratified.
The acini (circled in blue) secrete into a network of small ducts (blue arrows) that in turn drain into larger, more eosinophilic duct segments indicated by blue asterisks. These larger segments will drain into the interlobar ducts.
- Endocrine Gland
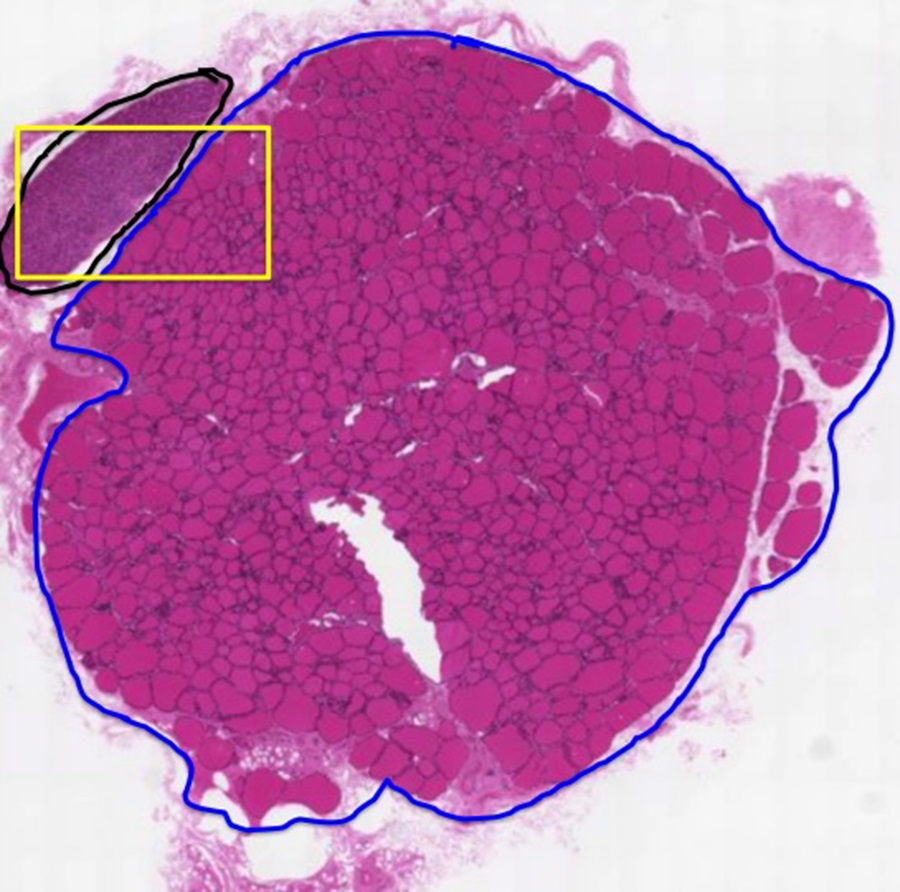
Slide 7: Thyroid and Parathyroid Gland: The section below contains two endocrine tissues, the thyroid gland (T) outlined in blue, and the parathyroid gland (PT)
outlined in black:
- Stain Information: Hematoxylin & Eosin:
- Pink/light purple = Cellular and extracellular proteins
- Dark purple/blue = Nuclei and cytoplasm rich in RNA
- Bright red = cytoplasm of erythrocytes
The thyroid tissue is comprised of many spherical follicles, each formed by a single layer of epithelial cells (one is outlined in yellow in the section below).
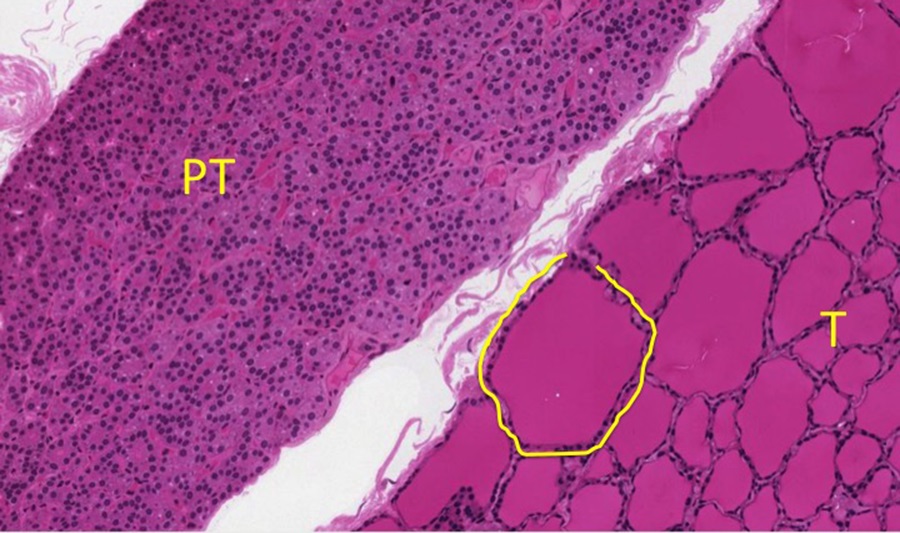
Depending on the metabolic activity, these cells may be flattened or quite tall. The intense eosinophilic material in the center of each follicle is a storage form of the hormone that these cells produce. The lack of any ducts in this tissue is a reflection of the endocrine nature of the tissue. The parathyroid gland is comprised of cords of epithelial cells invested with an extensive capillary network. Again, note the lack of ducts in this endocrine tissue. The high density of epithelial nuclei in the parathyroid tissue gives it a basophilic appearance at low magnification.
Optional activity: Can you complete the quiz at this link?
- ARCHIVAL PRE-CLASS MATERIALS FOR THIS SESSION:
-
- Pre-recorded videos: Epithelia
- Part 1: Introduction to Epithelia
- Note: The cytoskeletal elements are mentioned in the video, but don’t forget there are also important transmembrane protein elements that you need to know (see the review table below):
Cell Junction Cytoskeletal Components Major transmembrane link proteins Tight junctions Actin microfilaments Occludins, claudins Adherens (Belt) junctions Actin microfilaments E-cadherin, catenin complexes Desmosomes Intermediate filaments (keratins) Cadherin family proteins (including desmogleins) Hemidesmosomes Intermediate filaments Integrins Gap Junctions NONE! Connexins
- Note: The cytoskeletal elements are mentioned in the video, but don’t forget there are also important transmembrane protein elements that you need to know (see the review table below):
- Part 2: Classification of Epithelium
- Powerpoint files for each video:
- Part 1: Introduction to Epithelia
- Pre-recorded videos: Epithelia
-

Feedback/Errata