Connective Tissue
SESSION OBJECTIVES
- Be able to describe the general characteristics of connective tissue.
- Be able to classify types of connective tissue.
- Understand the functions of collagens, elastin and glycoproteins.
- Describe and name the types of cartilage and give examples of where each of them are found in the body.
OPTIONAL PRE-CLASS MATERIALS FOR THIS SESSION:
- Skim the section titles, bolded terms, and image captions from Junqueira’s Basic Histology, Chapter 5-7 (Click here for FMR library resources) to fill in any knowledge gaps you need.
OVERVIEW:
Connective tissue consists of cells and a matrix composed of extracellular fibers and ground substance produced by connective tissue cells. The amount and nature of each of these components varies, depending upon the type of the connective tissue. Connective tissue is derived from mesoderm and ectoderm during embryogenesis and influences the development of associated epithelia.
FUNCTIONS OF THE CONNECTIVE TISSUES (Session Objective #1)
- CONNECTION: The major function is to provide mechanical attachment (tendons, ligaments), to surround and enclose other structures (fascia, capsules), and to anchor tissues to each other (basement membranes, basal lamina).
- SUPPORT: Collagen fibers provide resistance to stretch (tendons) and provide supporting networks for non-connective tissue cells (reticular fibers of bone marrow, lymph nodes). Elastic fibers provide resilient attachment (yellow ligaments of vertebral column). The parenchyma (cells carrying out the function) of an organ is embedded in a connective tissue stroma (cells supporting the parenchymal cells).
- STORAGE: Fat, water, electrolytes and plasma proteins are sequestered in connective tissue in large quantities. Edema results from an increased accumulation of capillary filtrates in the loose connective tissue.
- DEFENSE: Resistance to invading organisms may be passive (due to the viscosity of matrix material and the barrier created by fiber bundles) or active (due to the presence of macrophages and cells of the immune system-e.g. plasma cells, lymphocytes). The spongy organization of loose connective tissue allows inflammation to occur as an orchestrated response to noxious stimuli (e.g. mosquito bite).
- SCARRING: Connective tissue serves to provide a strong repair matrix in damaged areas of organs or other tissues that regenerate poorly (e.g. cardiac muscle).
CLASSIFICATION OF CONNECTIVE TISSUE (Session Objective #2)
- CONNECTIVE TISSUE (CT) PROPER
- Loose (areolar) CT-relatively low density of fibers; no ordered orientation of fibers-irregular.
- Dense -fibers more tightly packed-predominantly collagen fibers
- Irregular-random orientation of fibers
- Regular-fibers more tightly packed-predominantly collagen fibers, directional organization of fibers to resist stress.
Dense irregular connective tissue has randomly oriented fiber bundles to resist stress in all directions (e.g., dermis of skin, submucosa of gut, organ capsules) whereas the fiber bundles in dense regular connective tissue have a parallel arrangement to resist stress in one direction (e.g., tendons, ligaments).
- SPECIALIZED CONNECTIVE TISSUE
Specialized connective tissues have an abundance of a usually minor connective tissue component.
-
- Elastic connective tissue occurs infrequently. It contains many bundles of elastic fibers embedded in a small amount of loose connective tissue (e.g., yellow elastic ligaments of vertebral column).
- Reticular connective tissue contains many reticular fibers and reticular fibers that form a supporting framework for other cells (very widespread and prominent in lymphatic and hematogenous tissues).
- Adipose tissue includes accumulations of fat cells subdivided into lobules by connective tissue partitions. It is rich in blood vessels, is the most metabolically active connective tissue, and responds to neural and hormonal stimuli.
- Cartilage (covered later in this chapter)
- Blood (covered in an earlier chapter)
- Bone (will be covered in an upcoming chapter)
COMPOSITION OF CONNECTIVE TISSUE PROPER (Session Objective #1)
- CELL TYPES: There are two cell types in connective tissue, those that are resident and those that enter the connective tissue from the blood (transient or immigrant).
- RESIDENT CELLS
- Fibroblasts are the predominant resident connective tissue cell in most connective tissues. Their major role is to synthesize fibers and matrix material. They can be stimulated to undergo division and resume active synthesis during wound healing. The mature cell is sometimes called a fibrocyte.
- Fat cells (adipose cells) are another type of resident cell that occur in small groups in loose connective tissue, or form larger, homogeneous accumulations throughout the body. Unilocular (yellow) fat consists of cells with one large droplet of fat in their cytoplasm. The cells of multilocular (brown) adipose tissue, which is present in fetal and newborn humans, contain several lipid droplets and have mitochondria that can uncouple oxidative phosphorylation to produce heat rather than ATP.
- Mesenchymal (adventitial) cells are stem cells thought to give rise to several other kinds of connective tissue cells, and to smooth muscle cells.
- RESIDENT CELLS
-
- TRANSIENT (IMMIGRANT) CELLS
- The most common immigrant cell type in connective tissue is the macrophage that enters the CT from the blood. The major role of macrophages is defense of the body by phagocytosis and pinocytosis of cellular remains, degraded intercellular substances, and foreign particles. You will learn that macrophages can contribute to tissue damage when inappropriately stimulated. Macrophages are most common in loose connective tissue.
- Mast cells are secretory cells with many large granules containing heparin (an anticoagulant) and histamine (a substance that stimulates dilation and increased permeability of capillaries). When released, these products contribute to allergic symptoms. Products released from mast cells can recruit other blood cells (eosinophils and neutrophils) to sites of mast cell activation.
- Lymphocytes and plasma cells (which are differentiated lymphocytes that secrete antibody) are usually rare in the connective tissue of most areas of the body, but are common in sites exposed to bacteria and foreign proteins and in regions of chronic inflammation. Granulocytic leukocytes are normally very rare in normal tissue.
- TRANSIENT (IMMIGRANT) CELLS
EXTRACELLULAR MATRIX PRODUCED BY RESIDENT CELLS OF CONNECTIVE TISSUE PROPER
Extracellular matrix (ECM) is mixture of fibrillar proteins and ground substance. The extracellular matrix (ECM) consists of several different macromolecules (the most important being proteins and proteoglycans) plus water and inorganic material such as salts. Since the proteins and proteoglycans are secreted by the widely different cells that form each tissue, the ECMs in these tissues are different as well. For example, the ECM of skin is different from the ECMs of bone and ligament. In general, cells that are attached produce some kind of ECM but a skin fibroblast produces considerably more ECM than a hepatocyte. ‘Free” cells such as erythrocytes and lymphoid cells do not secrete an ECM
ECM is most often associated with connective tissue, where it literally fills the space among the cellular constituents. For example, some ligaments are composed of specialized fibroblasts that secrete a fibrillar ECM consisting mostly of elastin, while a tendon’s ECM contains primarily collagen and the ECM of hyaline cartilage is largely proteoglycan and water (more on cartilage later).
Knowledge Check: Identify the Structures of the ECM in Loose Connective Tissue:
COMPONENTS OF THE ECM (Session Objective #3)
- FIBERS
- COLLAGENS: The collagens are a multigene family of proteins including at least 10 different molecular types. Collagen type is determined by the composition of the polypeptide chains which make up the collagen molecule. They are specialized for different functions and their synthesis is developmentally regulated. You are expected to know where these major types of collagen are found.
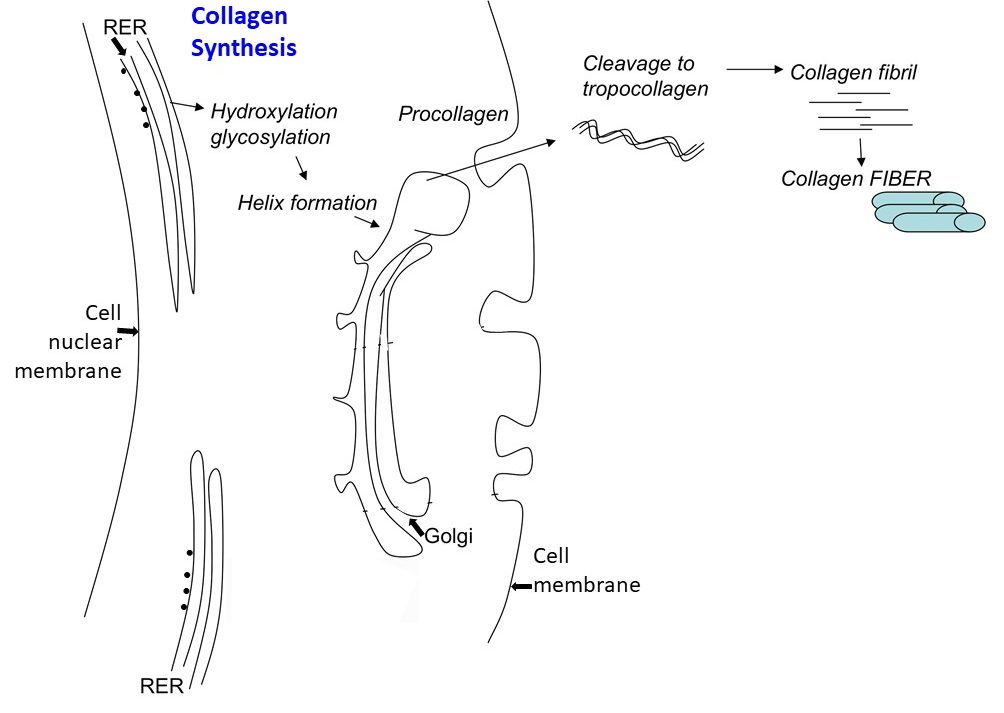
- It is important to understand the biosynthesis of collagen as it is tied to many clinical conditions when incorrectly/incompletely synthesized:
| Examples of Some Defects of Collagen Synthesis That Can Cause Clinical Conditions: | ||
| Condition | Collagen Synthesis Defect | Presentation |
| Ehlers-Danlos Syndrome | Inability to cross-link procollagen molecules | Defects of intestine, acsending aorta, augmented skin elasticity and articular hypermobility. |
| Scurvy | Lack of vitamin C = deficiency in proline and lysine hydroxylase. | Impaired wound healing, deficient fibroblast and bone cell function, defective tooth formation, ulceration of gums, hemorrhages. |
| Osteogenesis imperfecta | Genetic mutation in collagen type I preventing helix formation. | Bone fragility, laxity of skin and ligaments, easily bruise, short wormian bones, blue sclerae, opalescent teeth, cardiac insufficiency. |
-
-
- THE COLLAGEN GENE FAMILY: Synthesis of collagen fibers requires intracellular (synthesis of pro-collagen) and extracellular (cleavage of pro-collagen to form tropocollagen, self-assembly of tropocollagen to form collagen fibrils, and the cross-linking of collagen fibrils to form collagen fibers). There is large family of different collagens. For our purposes here we will consider only a small subset of them.
- Fibrillar Collagens
- Type I. Very abundant; Skin, Tendon, Bone, Dentin
- Type II. Cartilage
- Type III. Internal organs “reticular” fibers
- Collagens of Specialized Extracellular Structures
- Type IV. Basement membrane
- Type VII. Anchoring filaments to basement membrane
- Fibrillar Collagens
- THE COLLAGEN GENE FAMILY: Synthesis of collagen fibers requires intracellular (synthesis of pro-collagen) and extracellular (cleavage of pro-collagen to form tropocollagen, self-assembly of tropocollagen to form collagen fibrils, and the cross-linking of collagen fibrils to form collagen fibers). There is large family of different collagens. For our purposes here we will consider only a small subset of them.
-
-
- ELASTIN
- Elastin is a fibrillar, rubbery, polymeric protein that is found in distensible tissues such as aorta, some ligaments, and skin. In the electron microscope it appears as an amorphous blob, often- with small microfibrils at the periphery. The turnover of elastin in the body is extremely low.
- Elastin Composition
- An elastin core of cross-linked elastin molecules
- An outer sheath of Fibrilin
- Elastin Composition
- Elastin is a fibrillar, rubbery, polymeric protein that is found in distensible tissues such as aorta, some ligaments, and skin. In the electron microscope it appears as an amorphous blob, often- with small microfibrils at the periphery. The turnover of elastin in the body is extremely low.
- ELASTIN
- GLYCOPROTEINS (Adhesion Proteins)
- Fibronectin. Fibronectin helps in the attachment of fibroblasts to collagen, in the migration of certain cells during embryonic development, and in anchoring cytoskeletal proteins to ECM proteins by forming a bridge across the plasma membrane.
- Laminin. Laminin is a large, cruciform glycoprotein that binds to type IV collagen, to heparin sulfate proteoglycan, and to cells. It is found exclusively in basement membranes.
- Laminin and fibronectin serve as ligands for a family of cell surface glycoproteins called integrins. Binding of laminin and fibronectin by integrins provides a mechanism for cells to receive signals from their extracellular environment and provides a means of cell attachment to the extracellular matrix.
- PROTEOGLYCANS (A protein core with associated Glycosaminoglycans)
- There are several classes of proteoglycans which show preferential distribution in given tissues. For example, chondroitin sulfate proteoglycan is located in cartilage. Proteoglycans give tissues (especially cartilage) a high degree of hydration. They are often complexed with other proteins of the ECM such as collagen. Proteoglycans are high molecular weight proteins with polysaccharide branches. Each consists of carbohydrate polymers called glycosaminoglycans (GAG) covalently linked to a protein core. GAG are chains of repeating disaccharide units: Amino sugar + hexuronic acid. As such, this group of molecules form strong polyanions-this accounts for their ability to be stained by cationic dyes. The highly charged nature of proteoglycans allows them to bind and concentrate positively-charged soluble factors, like water.
-
Examples of Glycosaminoglycans making up “Ground Substance” Example Location Hyaluronic acid (often forms the “back-bone” for proteoglycans to link to) Broadly: Connective tissue, synovial and vitreous fluid, cartilage Chondroitin sulfate Cartilage, bone, aorta Heparan sulfate Aorta, liver, lung, basal lamina Keratan sulfate Cornea, intervertebral discs
SPECIALIZATIONS OF ECM
- BASEMENT MEMBRANE: Basement membranes (BM) can be thought of as specialized ECMs. As you learned in the epithelia chapter, the basement membrane is a sheet-like structure that lies beneath epithelial and endothelial cells, separating epithelia from the underlying tissue. A basement membrane is a combination of the basal lamina and a layer of connective tissue (recall it is called the reticular lamina). The basal lamina contains principally type IV collagen, the glycoprotein laminin, and heparin sulfate proteoglycan and is intimately associated with the cell that produced it (epithelial, muscle, glial). The reticular lamina is produced by cells of the surrounding connective tissue. Type VII collagen fibers anchor the basal lamina to the reticular lamina and are sometimes called anchoring filaments.
- Fibroblasts, lymphoid cells and blood cells lack a BM; in contrast, epithelial cells, endothelial cells lining blood vessels; cardiac, smooth, and skeletal muscle cells; and adipocytes have BMs. BMs are important for filtration and the maintenance of ion fluxes. Several types of disease, many of which are immunologic in nature, cause characteristic BM pathology. For example, in diabetes, the BM of several (but not all) tissues becomes quite thick, notably in the capillaries of the retina and in the kidney.
- The transition from in situ to invasive carcinoma involves a breakdown of BM integrity. Epithelial cells normally rest on a continuous BM. Invasive tumor cells penetrate the BM and gain access to the underlying connective tissue. Eventually, the tumor cells enter blood vessels (by traversing the capillary BM) or lymphatics (no BM). In many instances tumor cells dissolve the BM in their path by secreting a special enzyme, type IV collagenase, that specifically degrades the type IV collagen in the lamina densa of the BM
- DERMIS: This connective tissue of the skin, under the epidermis, consists of a thin, outer, connective tissue layer called the papillary layer and a thick, inner irregular dense connective tissue layer called the reticular layer. Both layers contain many elastic fibers and a rich network of blood vessels, lymph vessels, and nerves. Leather is made of the reticular layer of animal dermis. We will revisit the dermis in the skin histology session of your INDE Block.
OTHER SPECIALIZED FORMS OF CONNECTIVE TISSUE
Fascia is a sheet of dense connective tissue that surrounds the body beneath the skin and encloses the bones, muscles, and organs. Aponeuroses are flat tendons of dense connective tissue (regular) attaching muscles to bone or connective tissue. Capsules are wrappings of dense connective tissue that contain organs. Trabeculae are partitions of dense connective tissue extending into an organ from the capsule.
CONNECTIVE TISSUE – EPITHELIAL TISSUE INTERACTION
Connective tissues act as a determinant of the pattern of the overlying epithelia. For example, an embryonic lung bud placed in tissue culture will develop branches in the presence of its surrounding connective tissue, will stop branching after the connective tissue is removed, and will branch again if lung connective tissue (but not other connective tissue) is restored. Dermis from the sole of the foot induces epidermal cells to form unusually thick, heavily keratinized epidermis, typical of the sole of the foot, irrespective of the epidermal cells’ site of origin.
CARTILAGE (Session Objective #4)
Cartilage is a specialized type of connective tissue that will get its own section in this chapter.
- CHARACTERISTICS: Rigid, but less resistant to pressure than bone, cartilage is rich in extracellular matrix and essential for the growth of long bones before and after birth. It supports soft tissues, covers joint surfaces, lacks blood vessels, nerves, and lymphatics, and repairs slowly.
- COMPONENTS: Like all other connective tissues, cartilage is composed of cells and extracellular matrix (ECM). Chondrocytes are cells that lie in lacunae and secrete ground substance and fibers (collagen and elastic). Chondrocytes arise from chondroblasts which in turn are derived from stem cells in the perichondrium, the connective tissue covering of cartilage. In the embryo, chondroblasts are derived from mesenchymal cells.
- The ECM of cartilage is composed of fibers and ground substance. The fibers are collagen (mostly Type II in hyaline and elastic cartilage; Type I in fibrocartilage) and elastin (in elastic cartilage). Cartilage ground substance is highly hydrated due to its chondroitin sulfate-containing proteoglycans, which includes a common unsulfated GAG: Hyaluronic acid.
- THE TYPES OF CARTILAGE:
- Hyaline Cartilage is the most common type of cartilage. It caps joint surfaces, forms the cartilage rings of the respiratory passages, and attaches the ribs to the sternum.
- Elastic Cartilage is similar to hyaline cartilage, but contains abundant elastic fibers. This flexible cartilage supports the epiglottis, the auricle of the ear and surrounds the auditory structures.
- Fibrocartilage has characteristics intermediate between those of hyaline cartilage and dense connective tissue. It contains chondrocytes and irregular bundles of collagen. Fibrocartilage is found in areas of stress, such as in the fibrous part of intervertebral discs and at the attachment sites of some ligaments to bones, notably the pubic symphysis.
- GROWTH OF CARTILAGE
1. Interstitial growth occurs from within by mitotic division of chondroblasts (can be thought of as growth in length, for example). It occurs mainly during early phases of cartilage growth, before the matrix becomes firm. This is reflected by clusters (often pairs) of chondrocytes, each cluster within individual lacunae. These clusters represent progeny of a dividing chondrocytes (“isogenous group”).
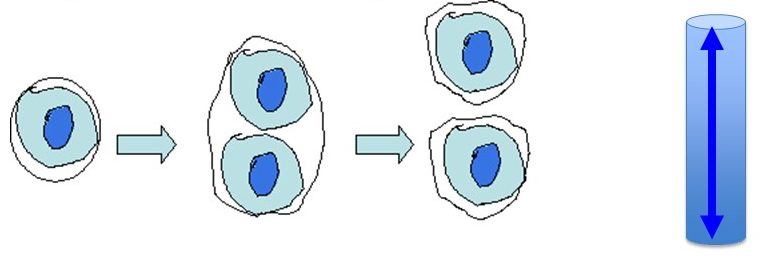
2. Appositional growth occurs by the addition of new cartilage onto the surface of pre-existing cartilage (can be thought of as growth in girth, for example). Cells responsible for appositional growth come from the perichondrium.
- REGENERATION AND REPAIR of cartilage occurs slowly and damage often results in a fibrous scar. The low metabolic rate of cartilage cells is probably related to the fact that the matrix is not vascularized, so nutrients and gases must diffuse across significant distances to reach the chondrocytes.
HISTOLOGY ATLAS AND PRACTICE EXERCISES
CONNECTIVE TISSUE PROPER
1. Loose Connective Tissue
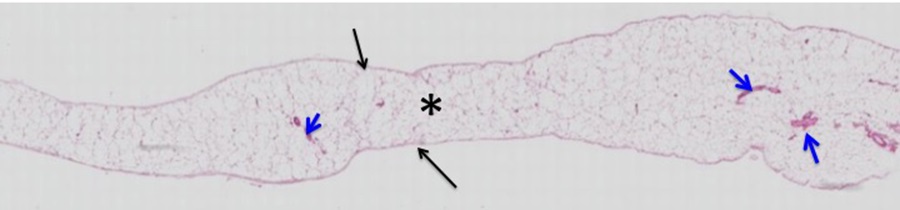
Slide 1: Mesentery of the Large Intestine
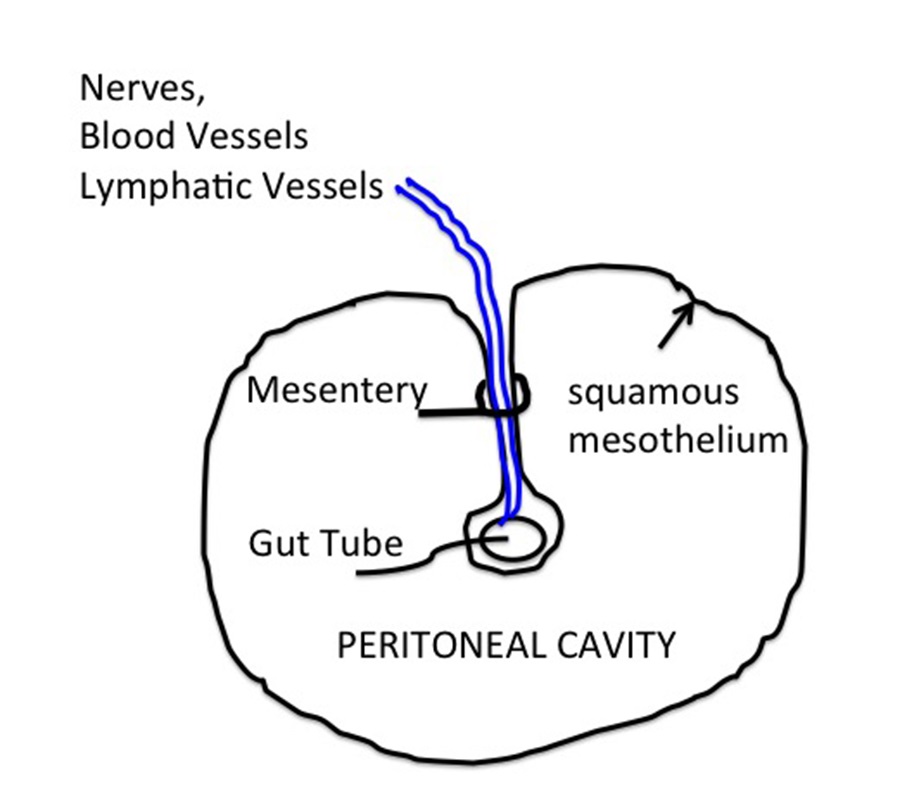 What is a mesentery? The mesentery consists of a squamous serosal epithelial cell layer (mesothelium, black arrows) covering loose connective tissue (black asterisk). Vessels (blood and lymph, blue arrows) and nerves that supply the intestine are found within the mesentery, and the gut tube (or any structure that has “grown” into the peritoneal cavity) will also be covered with mesothelium. The section below shows mesentery associated with the large intestine.
What is a mesentery? The mesentery consists of a squamous serosal epithelial cell layer (mesothelium, black arrows) covering loose connective tissue (black asterisk). Vessels (blood and lymph, blue arrows) and nerves that supply the intestine are found within the mesentery, and the gut tube (or any structure that has “grown” into the peritoneal cavity) will also be covered with mesothelium. The section below shows mesentery associated with the large intestine.
Stain Information: Hemotoxylin and Eosin. Low Magnification
Higher Magnification:
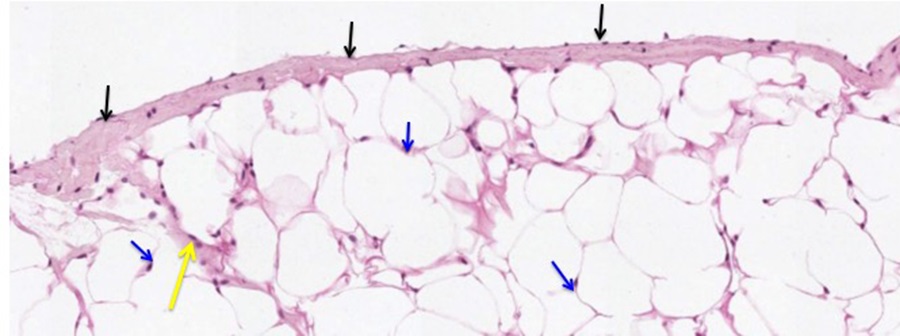
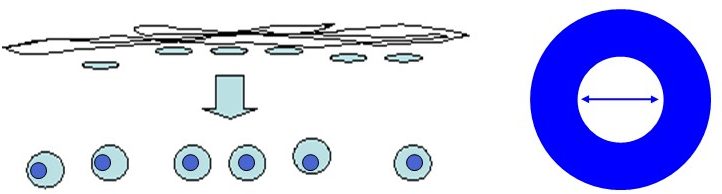
At higher magnification, note the unilocular adipocytes that comprise most of the connective tissue here. Due to the organic solvents used to process tissues for histologic analysis, the lipids within the adipocytes have been extracted, making the adipocytes appear “empty”. Note the thin rim of cytoplasm that surrounds the lipid droplet and the laterally displaced nuclei within the adipocytes (blue arrows). Also examine the squamous serosal mesothelium (black arrows) and the framework of connective tissue within the mesentery (yellow arrow).
Slide 2: Whole Mount of Mesentery.
Stain Information: Elastic Fiber Stain. Higher Magnification
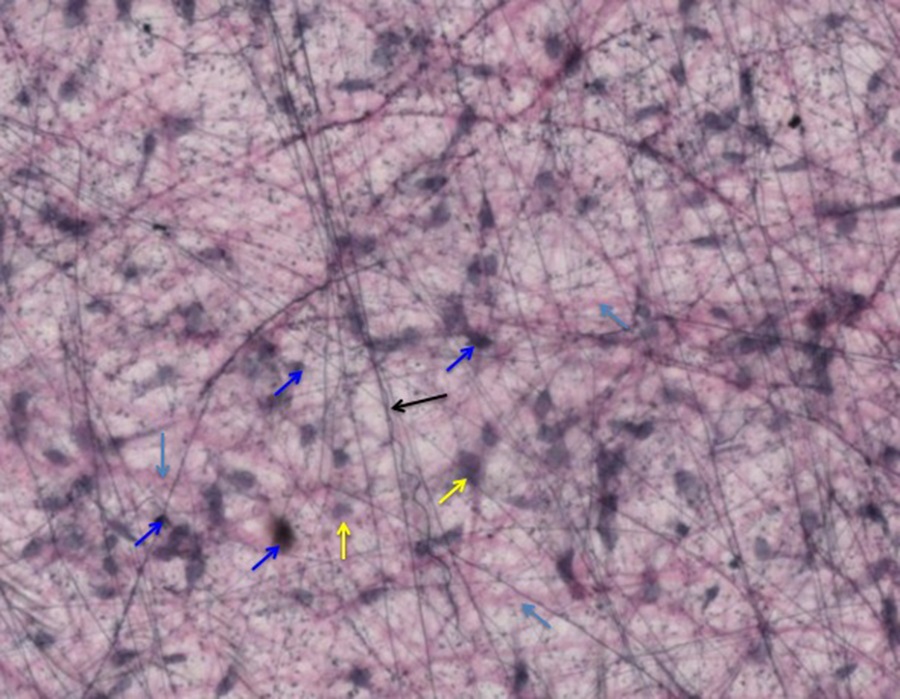
You are looking through two layers of squamous mesothelium with fibroblasts and two types of connective tissue fibers, elastic and collagen in between them. The mesothelial cell nuclei (yellow arrows) are relatively large and stain less intensely than the nuclei of fibroblasts (blue arrows), which are smaller. You will notice two types of fibers within the mesentery. The delicate and branched ones (black arrows) are elastic fibers and the thicker and more eosinophilic ones are collagen fibers (light blue arrows).
Optional activity: You can practice looking at loose connective tissue using a virtual microscope with guiding text in the right panel at this link.
2. Dense irregular connective tissue
Slide 3: Testis.
Stain Information: Hemotoxylin and Eosin. Low Magnification
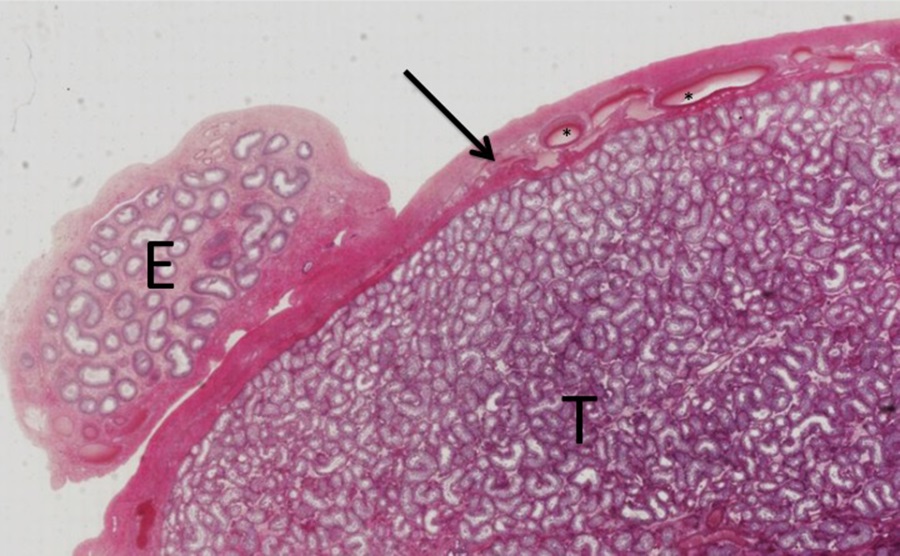
This is a portion of the testis (T) and epididymis (E) demonstrating the thick capsule of dense irregular CT (arrow) that encompasses the testis. Dense irregular CT encapsulates most organs. While dense irregular and regular connective tissue both have a high representation of extracellular matrix proteins, these extracellular matrix proteins are much more randomly oriented in irregular connective tissues.
Higher Magnification: Dense irregular connective tissue
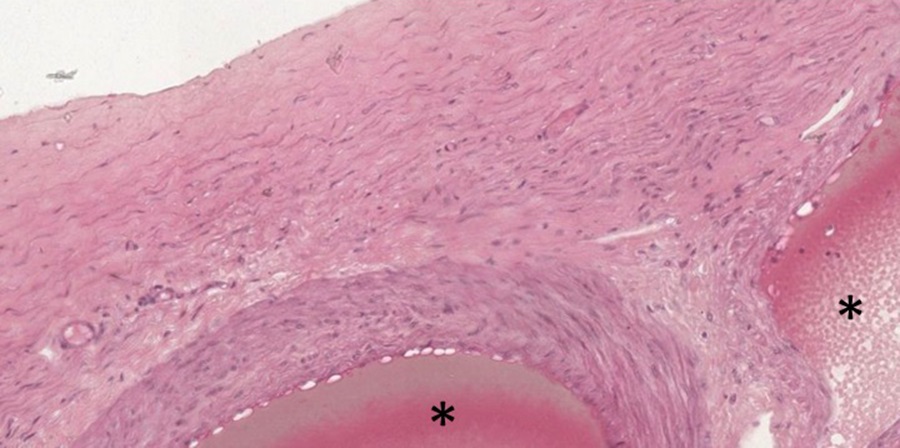
At higher magnification, the paucity of nuclei is evident. Embedded within the capsule are blood vessels (asterisks), here cut in cross section.
Slide 4: Skin/Integument
Stain Information: Hemotoxylin and Eosin, some discoloration of section. Low Magnification
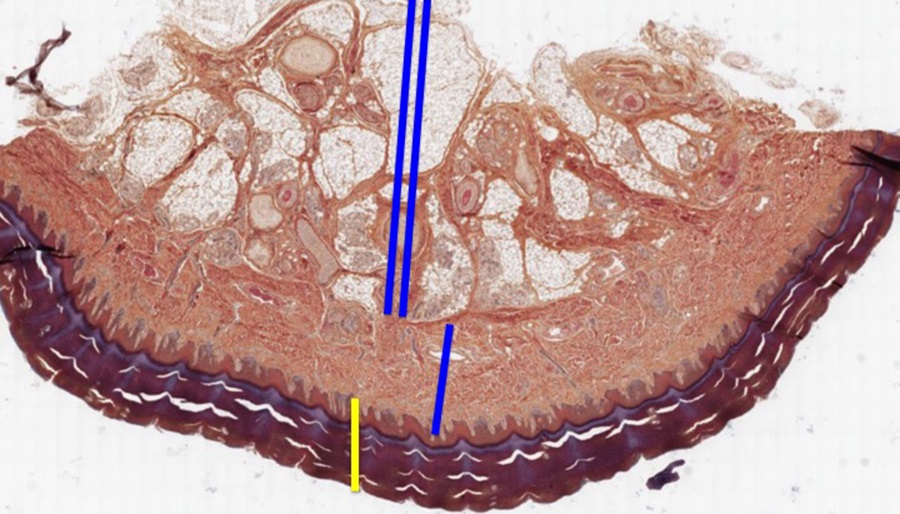
Both dense irregular and loose connective tissues contribute to the organization of skin. In the low magnification image of skin above, the epithelium comprising the epidermis is indicated by a yellow bar. The epithelial compartment interdigitates with the connective tissue of the dermis. The connective tissue compartment of skin is divided into the dermis immediately below the epithelium (dense irregular connective tissue), indicated by a single blue bar and the hypodermis/subcutaneous connective tissue (loose connective and adipose tissue) deep to the dermis indicated by a double blue line. The hypodermis is the target of subcutaneous injections.
Higher Magnification: Dense Irregular Connective Tissue of the Dermis
The dermis contains a lot of fibrillar extracellular matrix material (collagen and elastic fibers) that is eosinophilic (discolored slightly in the image above). Notice the haphazard arrangement of ECM fibers characteristic of well-named dense irregular connective tissue.
Lower Magnification: Dense Irregular Connective Tissue
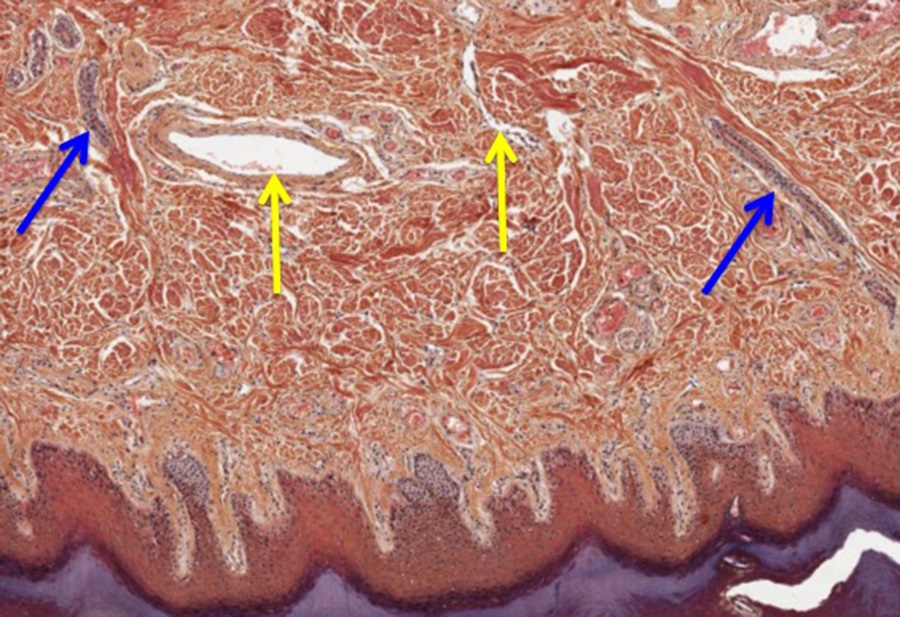
Within the dermis you will find blood vessels (yellow arrows) and ducts from glands (blue arrows) in the hypodermis making their way to the periphery of the skin.
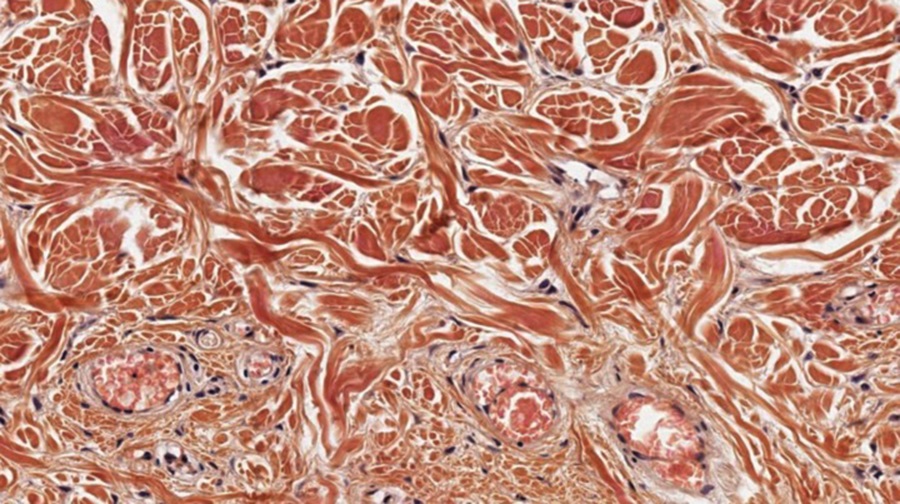
Higher Magnification: Loose Connective Tissue and Adipose in the Hypodermis
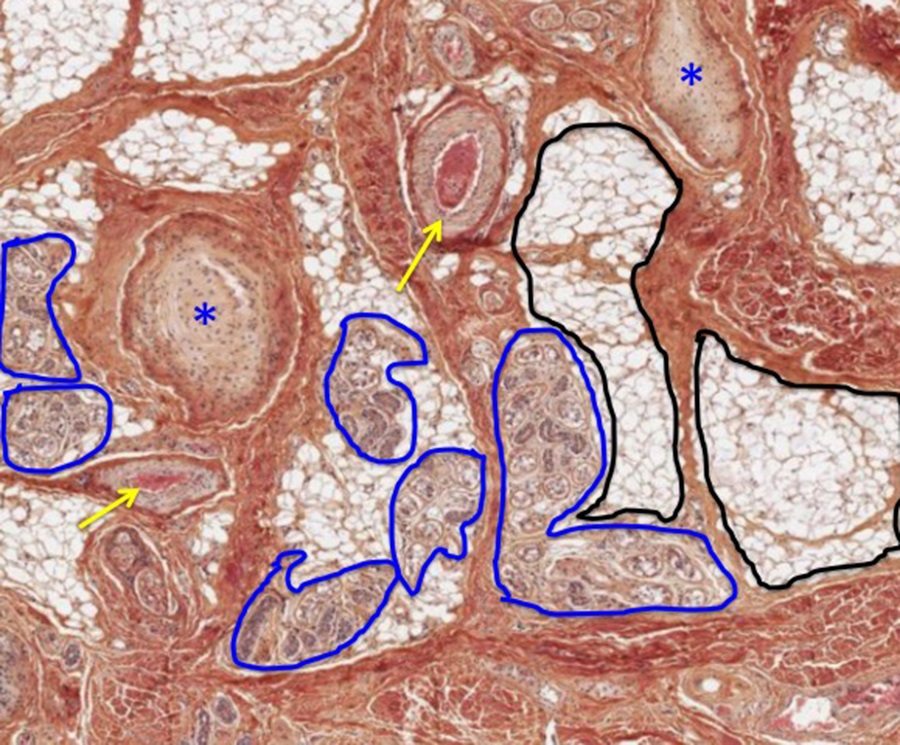
The deeper layer of connective tissue (Hypodermis or subcutaneous tissue) is much more loosely arranged and can be considered as loose connective tissue. Here you will find epithelial glands (outlined in blue) that are connected to the outside world via ducts penetrating to the epidermis, other special sensory nerve endings, Pacinian corpuscles (blue asterisks, more about these in the INDE block), larger blood vessels (yellow arrows), and unilocular adipose tissue (outlined in black). In gross anatomy, the hypodermis is known as superficial fascia.
Slide 5: Mammary Gland.
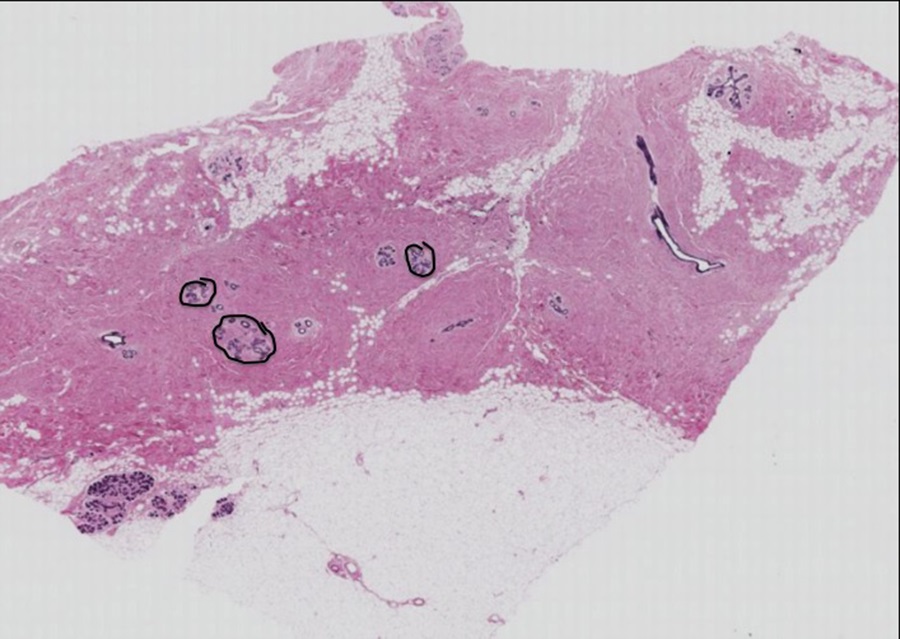
Stain Information: Hemotoxylin and Eosin. Low Magnification
The section below is of an inactive mammary gland. This section demonstrates mammary gland epithelium (circled and shown at higher magnification below) embedded in a mixture of loose and dense irregular connective tissue in addition to adipose tissue.
Higher Magnification: Inactive mammary gland epithelium in loose and dense irregular CT
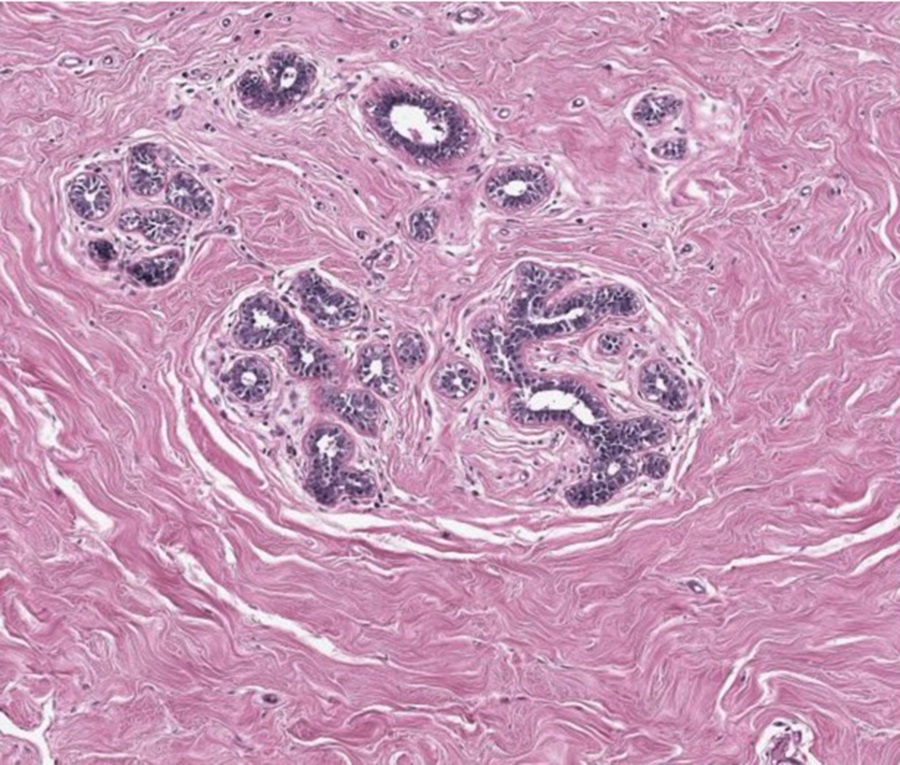
Similar Magnification, different location of the section: Inactive mammary gland
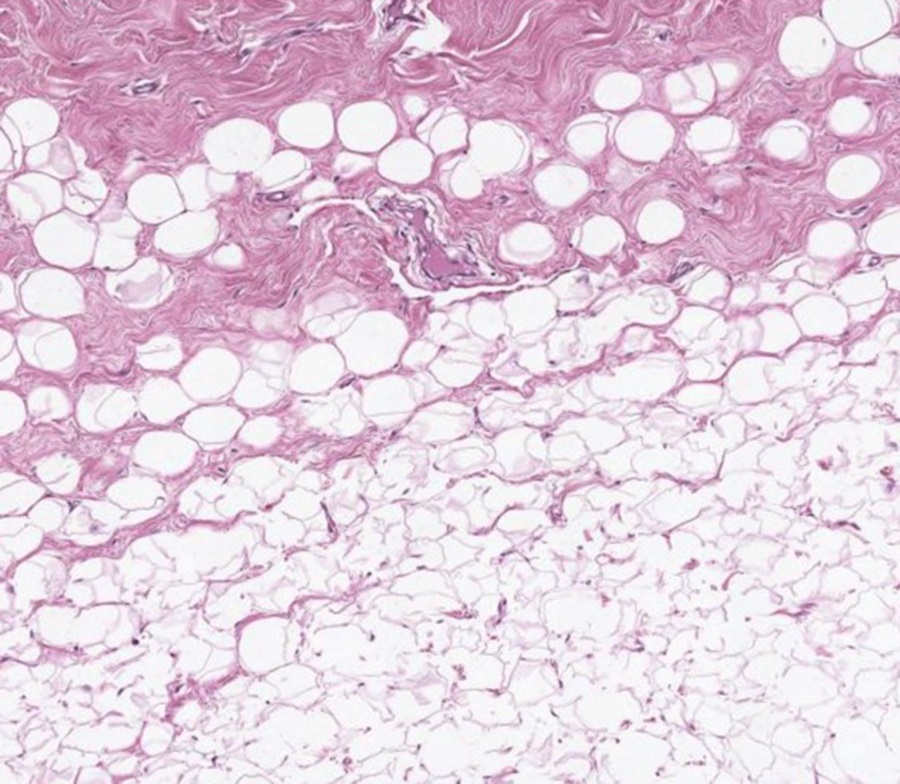
You can identify the characteristic adipose tissue and the more eosinophilic connective tissue below. The scarcity of nuclei in both the sections above and below tells you that there is a lot of extracellular matrix protein compared to cells.
3. Dense regular connective tissue
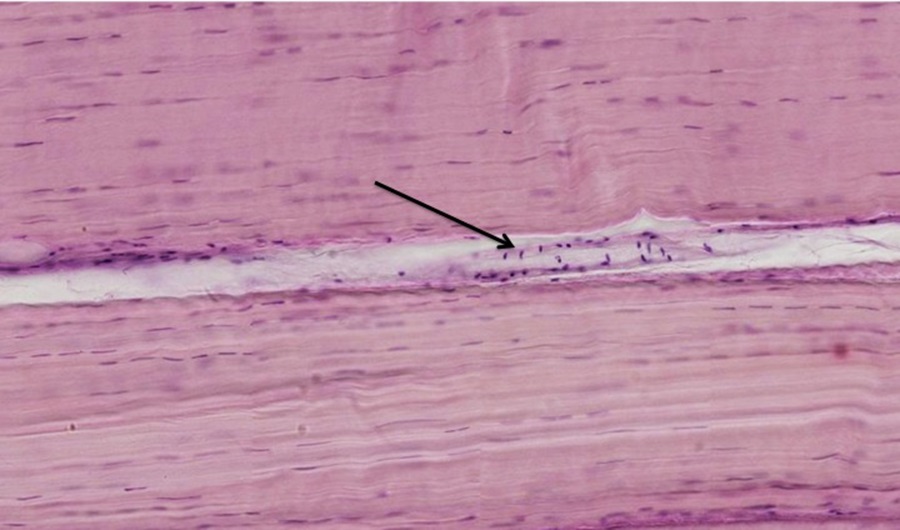
Slide 6: Tendon.
Stain Information: Hemotoxylin and Eosin. Low Magnification
This type of connective tissue is highly ordered and oriented to resist mechanical forces, with parallel collagen fibers and relatively few cells (image below). Except for the parallel orientation, there is little organization of the eosinophilic material. This dense regular connective tissue is organized in bundles separated by thin sheets of connective tissue (arrows).
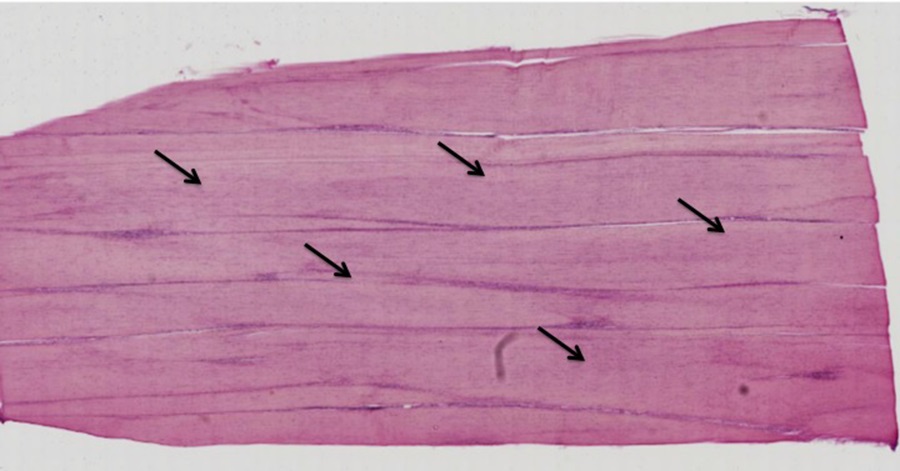
Higher Magnification: Dense Regular Connective Tissue
The relative scarcity of basophilic nuclei is apparent and a blood vessel between the bundles of collagen is indicated by the arrow on the image below. This vessel will feed into a capillary bed within the tendon.
Optional activity: You can practice looking at dense regular connective tissue using a virtual microscope with guiding text in the right panel at this link.
Tissues rich in elastic fibers
Slide 7: Blood Vessel, Elastic Fibers.
Stain Information: Hemotoxylin and Eosin with Verhoeff Special stain. Low Magnification
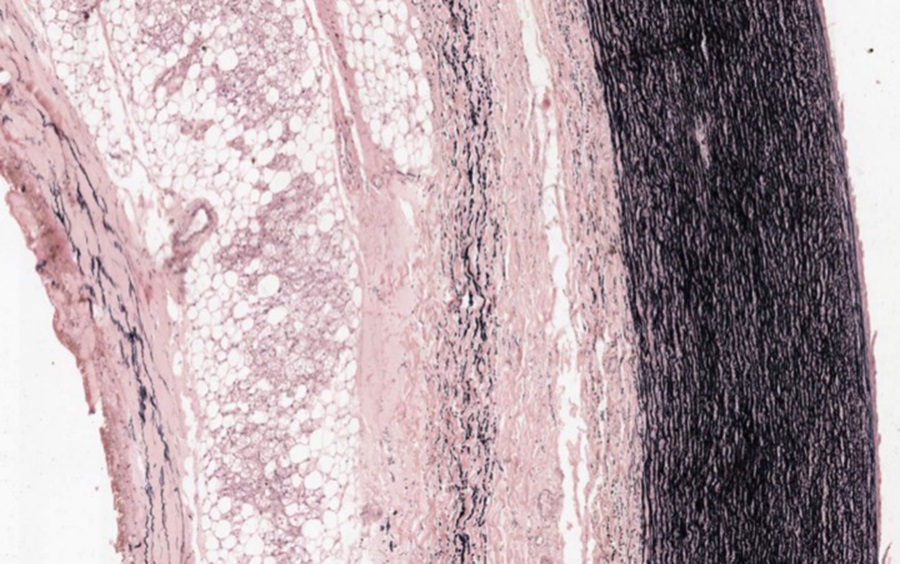
The image above depicts the connective tissue associated with the aorta. This section has been processed to demonstrate elastic fibers (black squiggly lines). We will examine the organization of blood vessels later in the course, but here you are to notice that some connective tissue can include elastic fibers.
SPECIALIZED CONNECTIVE TISSUES
1. Reticular Connective Tissue
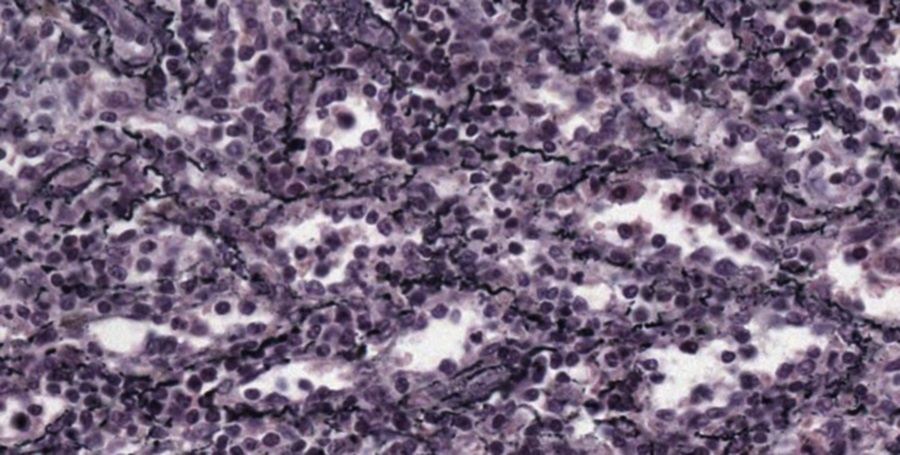
Slide 8: Spleen, Reticular CT
Stain Information: Silver Stain. Low Magnification
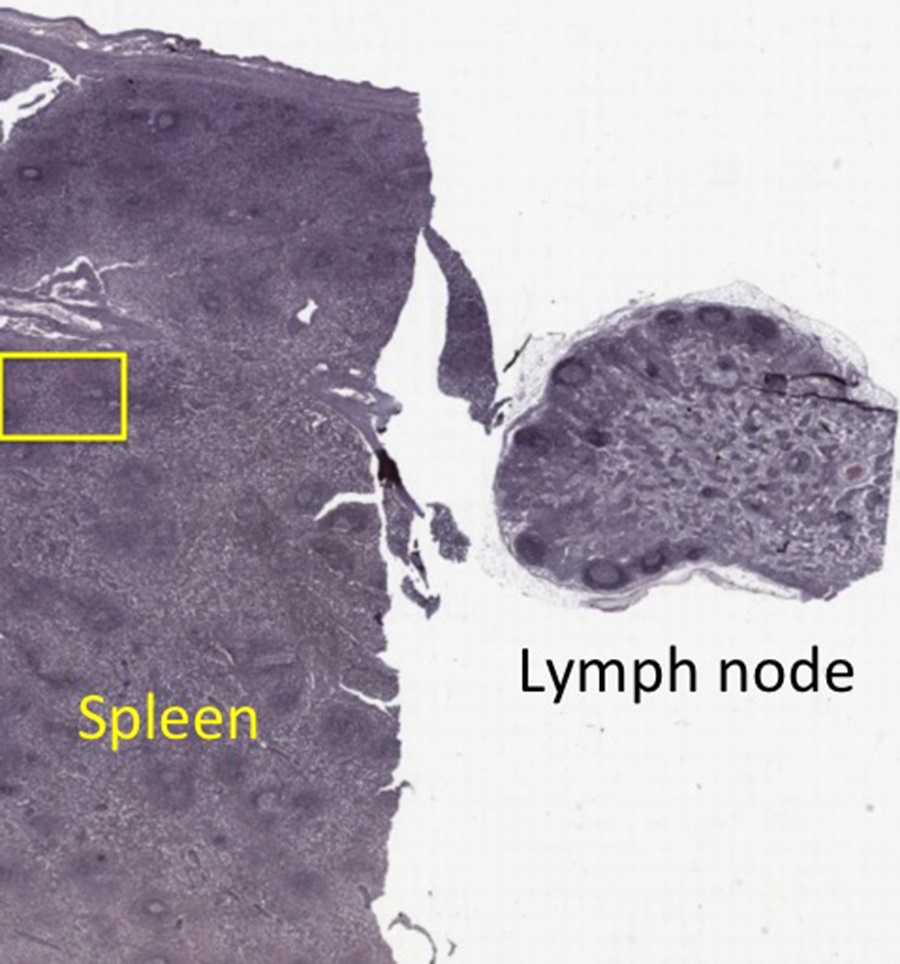
Spleen and lymph node samples shown above were prepared with silver stain to demonstrate reticular fibers (Type III collagen). These fibers form the structural framework for many tissues, including spleen. The fibers appear as discreet black lines, (see higher magnification of yellow box below) while other tissue detail is minimal. We will revisit this material when we consider the organization of the spleen.
Optional activity: You can practice looking at reticular connective tissue using a virtual microscope with guiding text in the right panel at this link.
2. Cartilage
Slide 9: Trachea, Hyaline Cartilage
Stain Information: Hemotoxylin and Eosin. Low Magnification
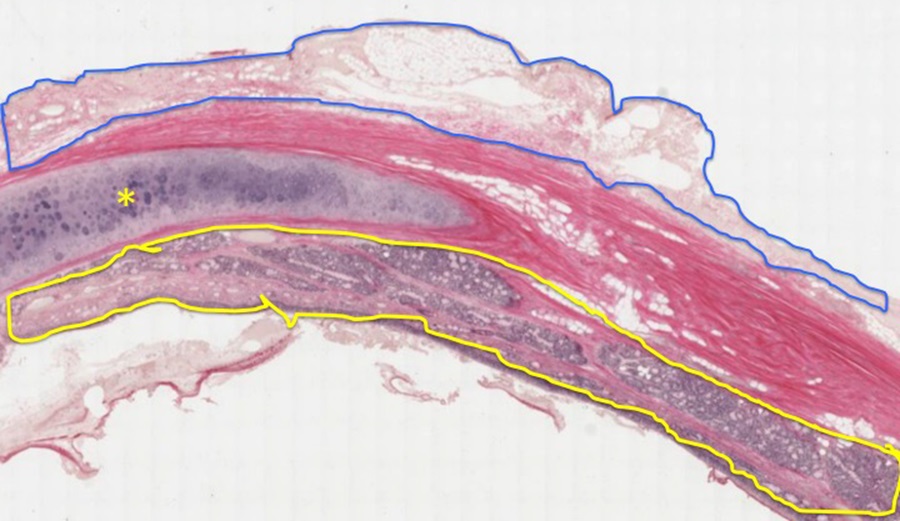
A sample of trachea containing part of a tracheal cartilage ring (yellow asterisk) is shown at low magnification above. Surrounding the cartilage is eosinophilic dense irregular connective tissue with scattered islands of adipose tissue. On the luminal face, outlined in yellow above, is a layer of respiratory epithelium (pseudostratified ciliated columnar) and associated glandular tissue. On the abluminal side, outlined in blue, is loose connective tissue, sometimes called adventitia.
Higher Magnification: Chondrocytes are in lacunae surrounded by extracellular matrix (see higher magnification image below).
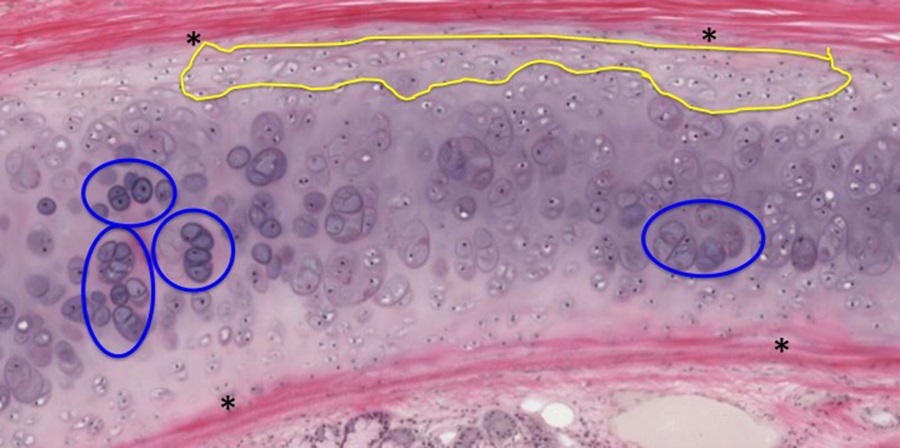
At the periphery of the cartilage is dense connective tissue of the perichondrium (asterisks). Some of the cells arising from perichondrium differentiate to become chondrocytes (appositional cartilage growth area outlined in yellow). Some of the lacunae contain more than one chondrocyte or are clustered together (circled in blue). This represents interstitial or growth of cartilage from isogenous groups of chondrocytes.
Optional activity: You can practice looking at hyaline cartilage using a virtual microscope with guiding text in the right panel at this link.
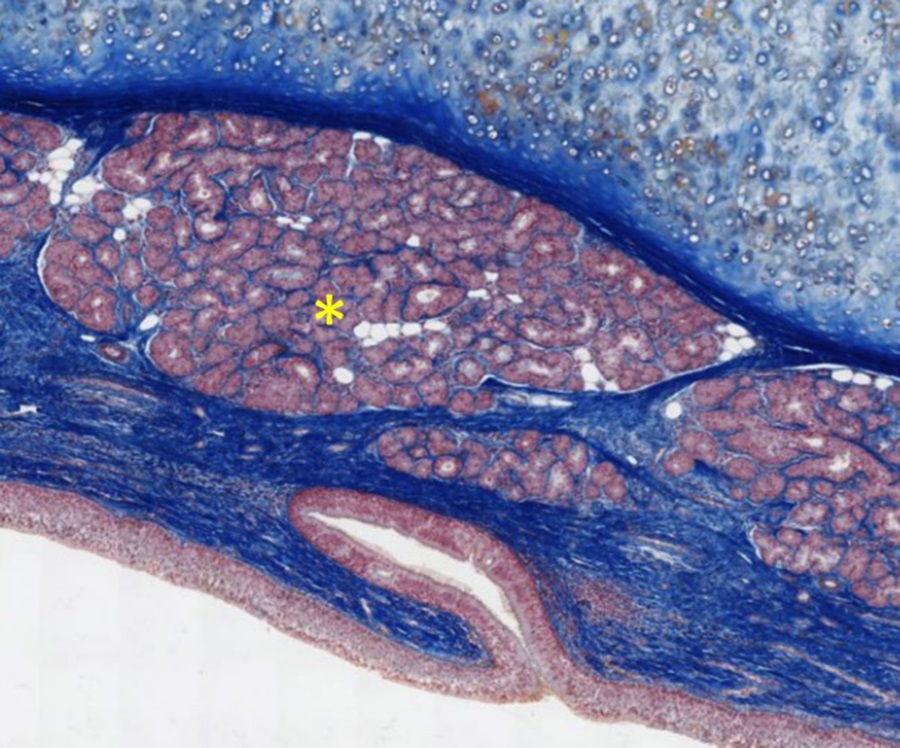
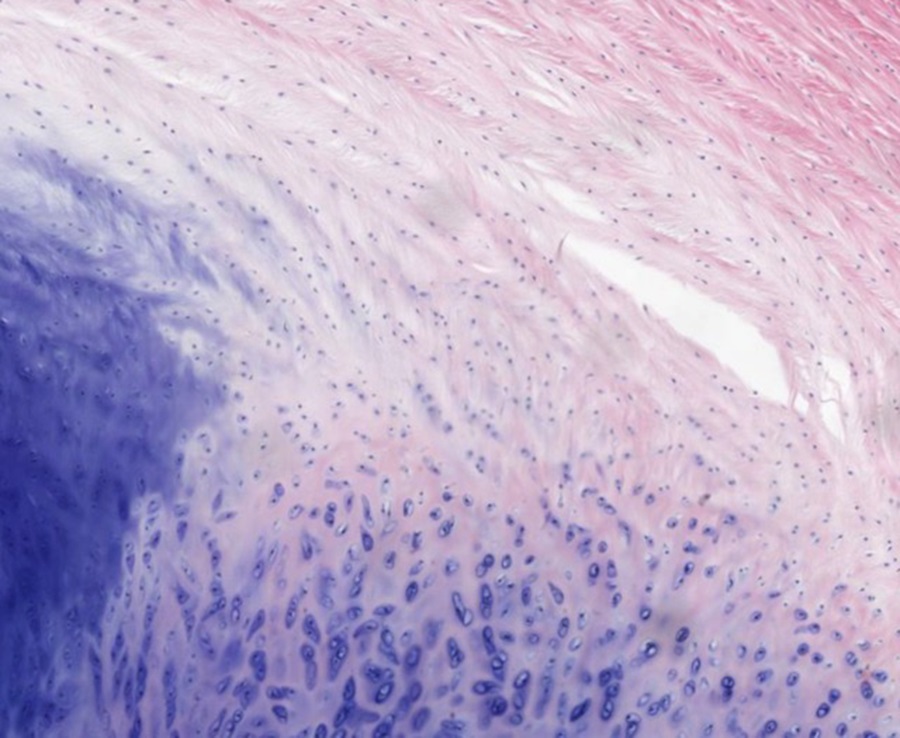
Slide 10: Epiglottis, Elastic Cartilage
Stain Information: Mallory Trichrome stain. Low Magnification
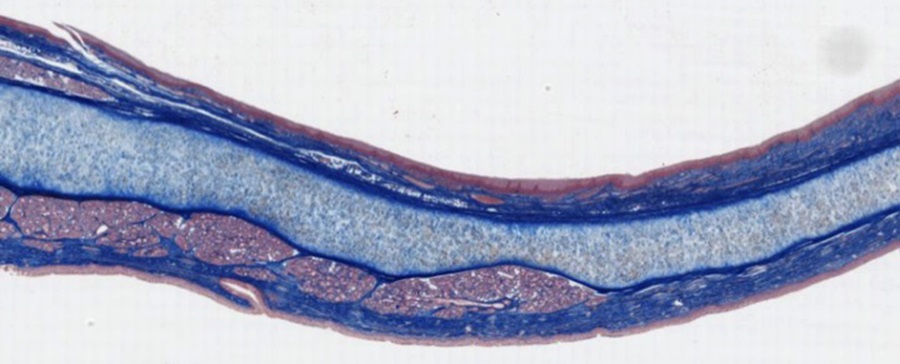
The epiglottis is a flap of elastic cartilage, covered with stratified squamous non-cornified epithelium. Sometimes the epithelium on the lower side transitions to respiratory epithelium. This is one of a few places where elastic cartilage is found.
Higher Magnification:
At higher magnification, you can see elastic cartilage (light blue area at top of image shown below) also has chondrocytes within lacunae and perichondrium (dark blue area below elastic cartilage) similar to the section of tracheal hyaline cartilage viewed above. Without specifically staining for elastin, these fibers are not obvious in histological samples. A mixed serous/mucous exocrine gland is indicated with an asterisk.
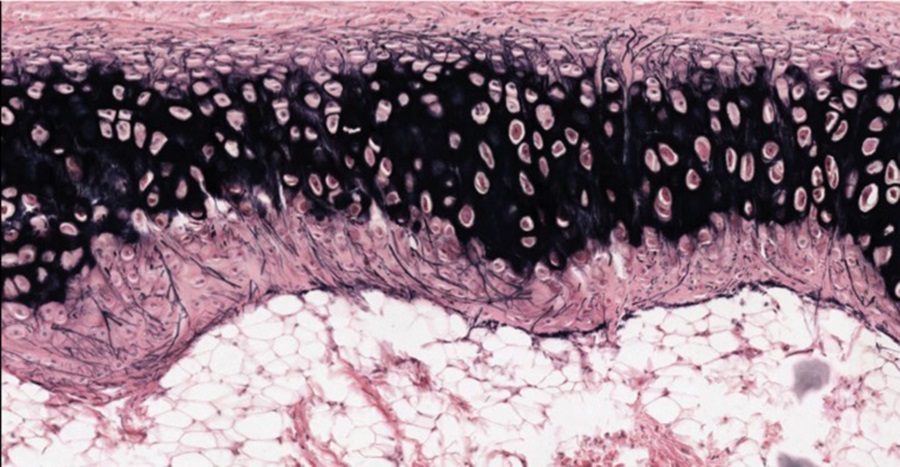
Slide 11: Epiglottis, Elastic Cartilage
Stain Information: H&E and Verhoeff. Low Magnification
Another sample of epiglottis that has been stained with H&E and Verhoeff to show elastin. The muscle that moves the epiglottis is indicated by an asterisk. Here also note that there are two plates of elastic cartilage separated by a layer of loose connective tissue.The lacunae are surrounded by matrix rich in elastin.
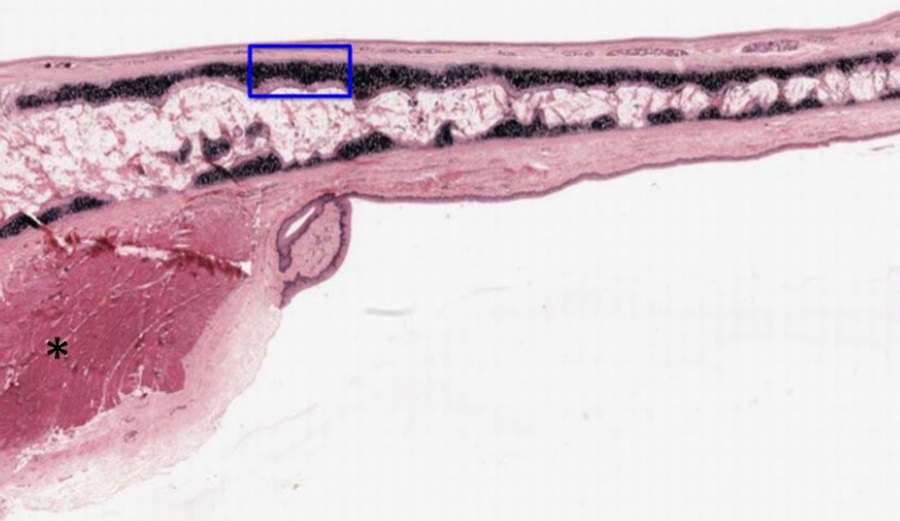
At high magnification of the region shown in the blue box, you can see that elastic fibers extend up into the perichondrium on the image below.
Optional activity: You can practice looking at elastic cartilage using a virtual microscope with guiding text in the right panel at this link.
Slide 12: Human vertebra, Fibrocartilage
Stain Information: H&E. Low Magnification
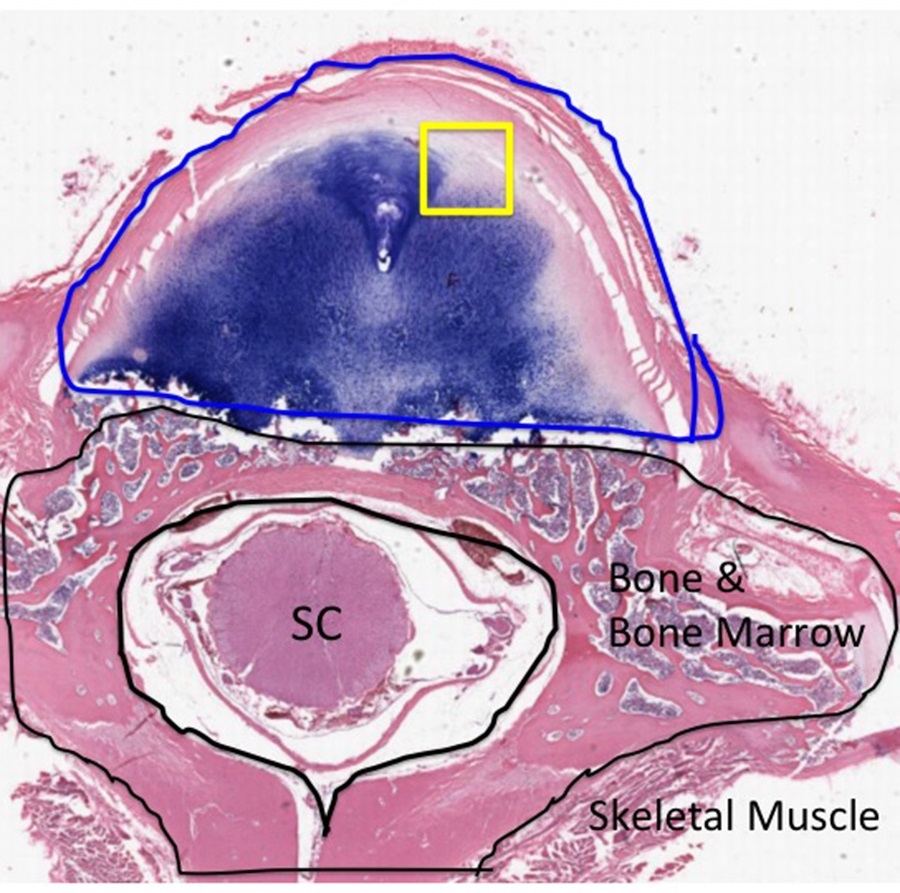
This section shown above displays a vertebral body and part of the intervertebral disc. The bone and bone marrow portion of the vertebral body are outlined in black and surrounds the spinal cord (SC). The intervertebral disc is outlined in blue. This section is through the upper or lower segment of the disc because no nucleus pulposus is included in the plane of section. Toward the center of the disc, the tissue clearly resembles cartilage, with prominent lacunae and chondrocytes. Toward the periphery of the disc, there are streaks of eosinophilia as the cartilage transitions into dense regular connective tissue. The spaces and irregularities represent artifacts of preparation. Note that this type of cartilage does not have a perichondrium.
Higher Magnification: Fibrocartilage
At higher magnification, you will note the fibrillar nature of the extracellular matrix. Note that the chondrocytes in the fibrocartilage are in characteristic lacunae. If this were dense irregular connective tissue, lacunae would be absent.
Optional activity: You can practice looking at fibrocartilage using a virtual microscope with guiding text in the right panel at this link.
Critical Concept:
This Chapter’s PDF
- Note: The interactive features of this chapter are not reproducible in this PDF format.
ARCHIVAL PRE-CLASS MATERIALS FOR THIS SESSION:
- Pre-recorded videos: Connective Tissue
- Part 1 (18:51)
- Part 2 (14:56)
- Part 3 (10:49)
- Error correction: On slide 20, elastin was said to stain with silver stain. Actually, elastin stains black with a special type of elastin stain. The ppt file has been corrected.
- Part 4 (12:55)
- Video Powerpoint file

Feedback/Errata