Blood
SESSION OBJECTIVES
- Define blood and list its basic functions.
- Explain the basic composition of blood, namely its plasma and its cells (formed elements).
- Describe how to make and view a blood smear.
- Know the basic shapes and functions of erythrocytes and platelets.
- Recognize the five types of leukocytes, and their distinctive cellular structures and functions (this is the most important objective).
- Learn the relative abundances of all the blood cells, especially of the different leukocytes.
OPTIONAL PRE-CLASS MATERIALS FOR THIS SESSION:
- Skim the section titles, bolded terms, and image captions from Junqueira’s Basic Histology, Chapter 12 (Click here for FMR library resources) if you feel you need more explanation.
OVERVIEW:
This is a summary of key concepts from the pre-recorded videos and arranged by session objective.
BLOOD (Session objective #1)
Blood is a specialized type of connective tissue that includes the liquid portion (plasma) and the formed elements (cells and platelets).
- Function: Delivers solutes (e.g. nutrients, hormones, ions, oxygen) to all parts/organs of the body and transports metabolic waste products (e.g. carbon dioxide) away from those same parts/organs.
- Tissue homeostasis is maintained by the soluble (liquid portion) and cellular constituents of blood.
- Changes in blood can give important clinical information about a patient:
COLLECTION AND PREPARATION OF A BLOOD SMEAR
(Session Objective #2)
Knowledge Check: To collect and prepare a blood smear, place the images in the correct order:
BLOOD COMPOSITION (Session Objective #3 and #6)
- 55% of total blood is plasma, the fluid portion that the cells are suspended in;
- 92% of blood plasma is water
- 7% are proteins (albumin, globulins, fibrinogen)
- 1% other solutes (e.g. electrolytes, nutrients, waste products)
- ~45% of total blood is erythrocytes (red blood cells);
- 4-6 x 106/μL
- Hematocrit is the packed RBC volume.
- ~<1% of total blood is leukocytes (white blood cells including granulocytes, monocytes, lymphocytes) and platelets (aka thrombocytes; pieces of cell membrane from megakaryocytes).
- 4.5 – 11.5 x 103/μL
- Neutrophils (60-70%)
- Lymphocytes (18-42%)
- Monocytes (2-11%)
- Eosinophils (1-3%)
- Basophils (0-2%)
- A handy mnemonic to remember the cell type names: Never Let Monkeys Eat Bananas
- Another handy mnemonic to remember the percentage of cell types in blood: 60-30-6-3-1 is the proportion of cell types normally found in blood.
- Platelets: 150-450 x 103/μL
- 4.5 – 11.5 x 103/μL
Blood Cell Death and Renewal (Hematopoiesis)
- Most blood cells are relatively short lived and are continuously replenished from a pool of progenitor cells located in the bone marrow. These stem cells are called Hematopoietic Stem Cells (HSC). Hematopoiesis, the formation of new blood cells, occurs in the bone marrow.
- Red blood cells: Live ~120 days
- 150-200 X109 RBCs are produced every day
- Platelets: Live ~9-12 days
- 150-200 X109 platelets are produced every day
Granulocytes (also called polymorphoneuclear cells, or PMNs): Live ~12 hours to several days
- 50-100 X109 PMNs are produced every day
- Lymphocytes: (Most) live for a month, others a lifetime
- Red blood cells: Live ~120 days
Changes in Blood Composition:
- Changes in RBCs can indicate anemias, reduced O2-carrying ability of blood
- Changes in platelets can indicate bleeding (thrombocytopenia)
- Changes in leukocyte numbers can indicate a number of immune responses or infections depending on the type of leukocyte that has increased numbers:
- Elevated neutrophils: Severe inflammation; typically indicative of bacterial infections (phagocyte response)
- Elevated lymphocytes: Often indicative of viral infection
- Elevated monocytes: Usually indicate a chronic inflammatory process
- Elevated eosinophils: Either an allergic response or parasitic infections
- Elevated basophils: usually only found in the context of myeloproliferative diseases (cancerous diseases of the blood-see lab practice below).
- The infiltration of immature forms of blood cells into the blood stream or tissues from the bone marrow indicates depletion of adult forms and serious conditions, such as leukemia. This is called a “left shift” and is often used in reference to immature neutrophils, or band cells, that are observed in peripheral blood.
ERYTHROCYTES (Session Objective #4)
- STRUCTURE: Mature red blood cells, erythrocytes, are:
- anuclear cells with smooth, eosinophilic cytoplasm;
- shaped like a biconcave disc;
- This shape enhances gas exchange,
- maximizes cell deformability through small vessels and intracellular spaces,
- is a product of the RBC’s specialized cytoskeleton.
- generally 7 – 8 μm in diameter;
- packed with hemoglobin.
- FUNCTIONS:
- Deliver oxygen (bound to hemoglobin) from lungs to peripheral tissues;
- Transport CO2 from tissues to the lungs;
- Buffer pH through HCo3– production
PLATELETS (Session Objective #4)
- STRUCTURE:
- Anucleate cell fragments
- Derived from the cytoplasmic fragments of bone marrow resident megakaryocytes (the largest cells of the body, ~50-150μm).
- Average size = 2.5μm
- Mean platelet volume (MPV) = 8-10 fL
- They have a granular internal structure and often look like “debri” on a blood smear in between cells.
- Anucleate cell fragments
- FUNCTIONS:
- Platelets are the key component of primary hemostasis (essential to initiate blood clotting)
- Store coagulation factors
-
Produce vasoactive substances
-
Thromboxane
-
Serotonin
-
-
Provide a phospholipid surface over endothelial injury surface for coagulation factors to bind and activate.
- Platelets are the key component of primary hemostasis (essential to initiate blood clotting)
LEUKOCYTES (Session Objective #5)
Knowledge Check:
- Leukocytes are a highly motile group of cells that can leave the blood stream in a directed manner.
- They are critical effector cells of the immune system with diverse functions.
-
They can be microscopically distinguished by the
-
Shape of nucleus
-
Polymorph- versus mononuclear
-
-
Granularity
-
Azurophilic primary granules
-
Specific secondary granules
-
-
Color of cytoplasm and granules in Wright stain
-
Determined by specific protein content
-
-
Types of Leukocytes Include:
A. Polymorphonuclear Granulocytes
- Neutrophils
-
- STRUCTURE:
- 12-15μm diameter
- Segmented nucleus (3-5 segments)
- Can look like “Mickey Mouse” cells
- FUNCTION:
- Active phagocyte:
- Recognize, engulf and kill bacteria and fungi
-
Use oxidative and non-oxidative killing mechanisms
- Will be elevated in blood stream during a bacterial infection
- Leave blood stream via diapedesis following a chemotactic gradient to enter tissues.
- Active phagocyte:
- STRUCTURE:
2. Eosinophils
-
- STRUCTURE:
-
12-15μm in diameter
-
Bilobed nucleus
- Prominent eosinophilic granules in cytoplasm
-
- LOCATION:
- Most eosinophils are found in connective tissue of mucosal linings
- Most eosinophils are found in connective tissue of mucosal linings
- FUNCTION:
-
Kill parasites and worms
-
Eosinophil secondary granules contains toxic major basic protein (MBP), eosinophilic cationic protein (ECP), eosinophilic peroxidase & neurotoxin
-
Have IgE receptors that furthers activation
-
-
Promotes allergic inflammation via secretion of cytokines and leukotrienes
-
Eosinophila (elevated blood count) indicates parasitic or allergic disease
-
- STRUCTURE:
3. Basophils
-
-
-
- STRUCTURE:
-
Bilobed nucleus (irregular; granules usually obscure shape of nucleus)
-
Specific granules stain cytoplasm a very grainy blue (basophilic)
-
-
- FUNCTION:
-
Promote anaphylactic reactions
-
Specific granules contain heparin, histamine and other factors of inflammation
-
-
Similar to mast cells in function
-
Migrate to tissue
-
Increased blood levels are suspicious of chronic Myelogenous Leukemia
-
- STRUCTURE:
-
-
B. Mononuclear Agranulocytes
1. Lymphocytes
-
- STRUCTURE:
- Smallest leukocyte (7-16μm), larger when activated
- Spherical nucleus that occupies ~90% of cytoplasm
- Sky blue cytoplasm
- TYPES:
-
Distinct lymphocyte subsets that cannot be microscopically distinguished include:
-
T-cells (CD4+; CD8+)
-
B cells (differentiate to plasma cells)
-
Natural Killer cells (aka NK cells, large granular; innate)
-
-
- FUNCTION:
- Lymphocytes are the effector cells of the acquired immune system
-
Antigen specific defense
-
Cytotoxic or antibody mediated immunity
-
Create memory
-
Mediators of autoimmunity
-
- Lymphocytes are the effector cells of the acquired immune system
- STRUCTURE:
2. Monocytes
-
- STRUCTURE:
-
Largest leukocyte (15-20μm)
-
Bean-shaped nucleus
-
Blue-gray cytoplasm light with “dust-like” membrane bound granules
-
Vacuoles often visible
-
- FUNCTION:
-
Monocytes are precursors to tissue resident macrophages and dendritic cells
-
Tissue resident macrophages are phagocytic cells (Mononuclear phagocytic system)
-
Contain azurophilic granules
-
- Antigen presenting cells
-
- Increased numbers in the blood during chronic inflammation.
-
- STRUCTURE:
HISTOLOGY ATLAS AND PRACTICE EXERCISES

Peripheral blood smear: The staining on this sample shown above is called Wright’s Stain. This stain is used for peripheral blood smears and it is similar to H&E in that it uses eosin as one of the dyes. However, instead of hemotoxylin it uses methylene blue dyes. As the image is scanned at an intermediate magnification, nucleated cells can be identified because of their basophilic nuclei. Below are images of leukocytes taken from this smear.
Optional activity: You can practice looking at mature RBCs using a virtual microscope with guiding text in the right panel at this link (please don’t worry about learning the immature forms at this point).
Optional activity: You can practice looking at platelets using a virtual microscope with guiding text in the right panel at this link.
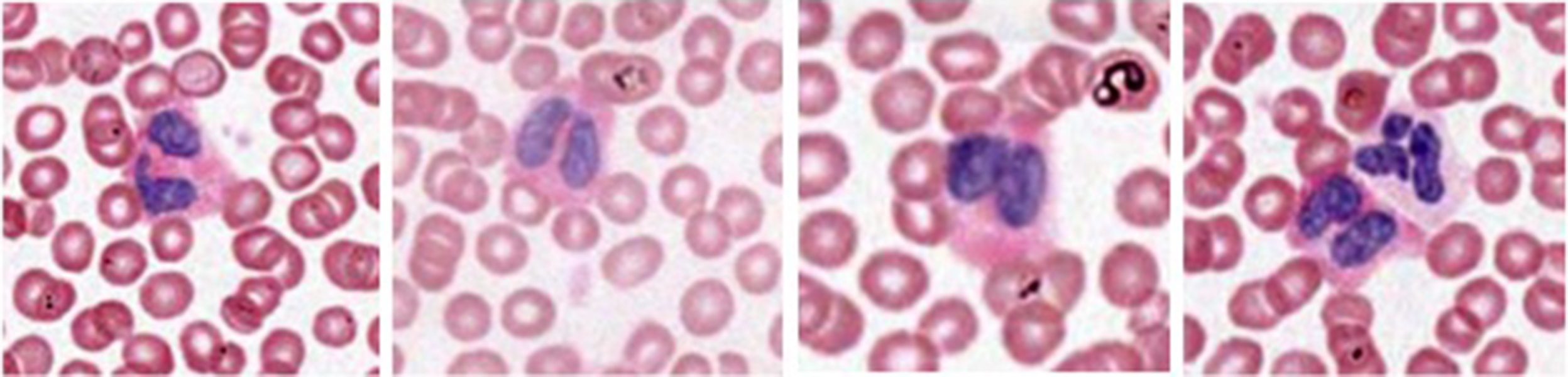
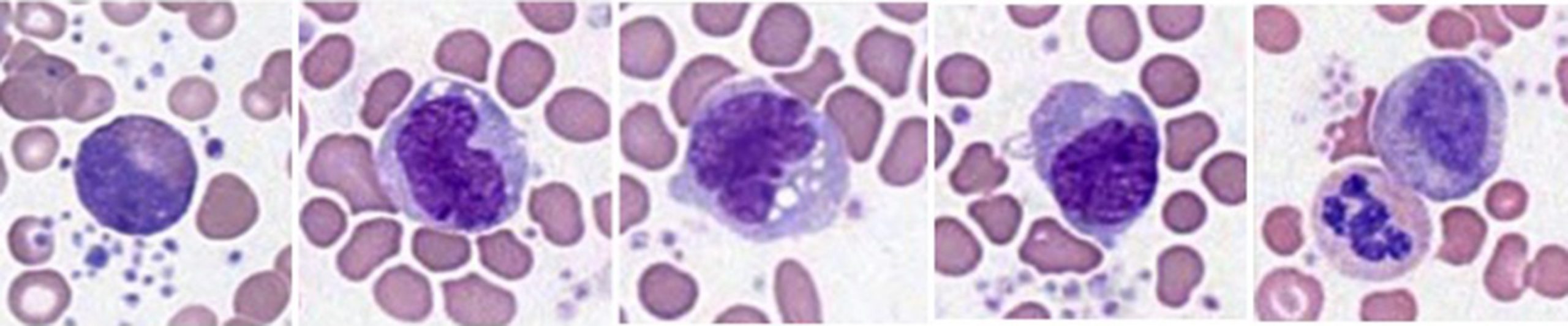
Neutrophils-Polymorphonuclear leukocytes

No distinctively stained granules. “Neutral” to acidophilic or basophilic dyes. Distinctive nuclear segmentation. The lower panel of images shows less mature neutrophils with less segmented nuclei. Remember that the nuclei of less mature neutrophils/polymorphonuclear leukocytes have less segmentation. “Shift to the left” of neutrophils in blood smear differential may be indicative of possible inflammatory response, when less mature neutrophils are recruited into the blood in response to systemic inflammatory stimuli.
An important concept is the “left shift” observed when mature neutrophils are depleted from fighting a severe infection. Examine the band neutrophils and left shift phenomenon at this link.
Optional activity: You can practice looking at mature neutrophils using a virtual microscope with guiding text in the right panel at this link (please don’t learn the immature forms except for band neutrophils at this point).
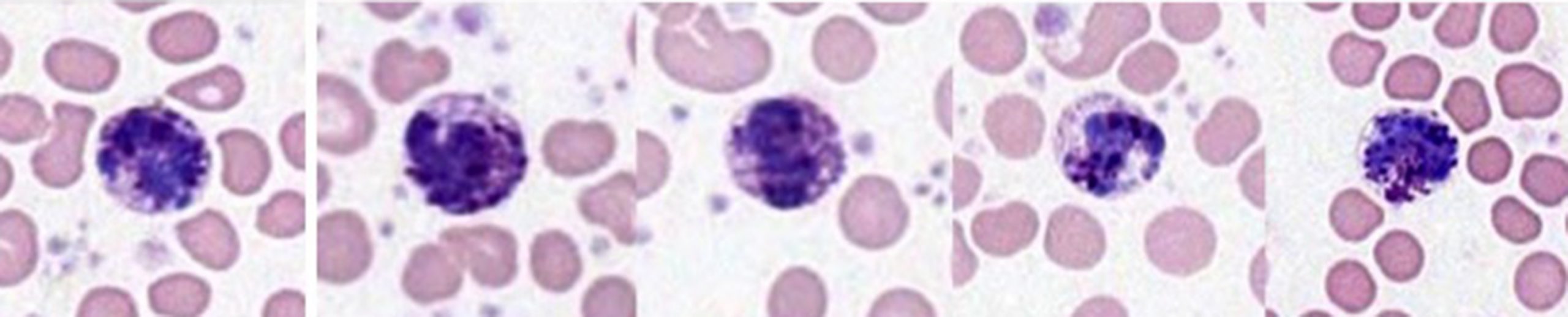
Eosinophils
Cytoplasmic granules are intensely eosinophilic. Nuclei are bilobed. The panel on the far right contains an eosinophil and a neutrophil so you can compare typical nuclear morphologies and cytoplasmic staining of the two cell types.
Optional activity: You can practice looking at mature eosinophils using a virtual microscope with guiding text in the right panel at this link (please don’t worry about learning the immature forms at this point).
Basophil
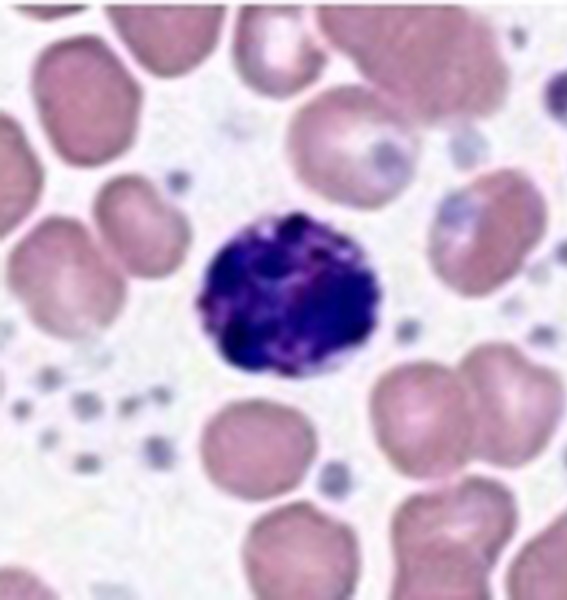
Basophils are pretty infrequent in normal blood. (this is a reminder to know the relative abundance of nucleated blood cells in peripheral blood!). Similar to eosinophils, the basophil nucleus is bilobed. Because of the coarse basophilic cytoplasmic granules, the nuclear morphology of basophils may be difficult to discern.
Optional activity: You can practice looking at mature basophils using a virtual microscope with guiding text in the right panel at this link (please don’t worry about learning the immature forms at this point).
Lymphocyte
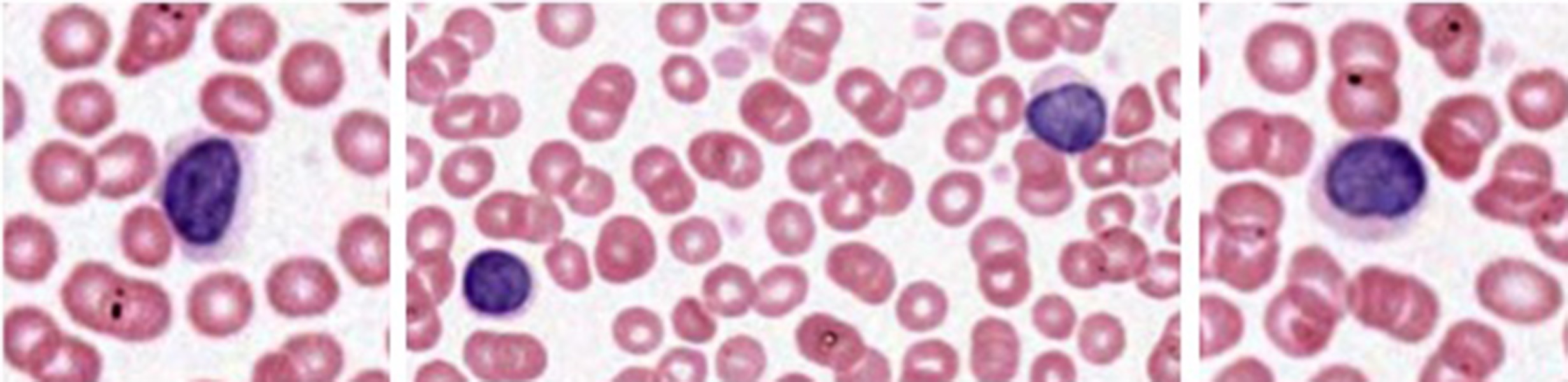
Lymphocytes have relatively little cytoplasm compared to their nuclei, which are densely packed with chromatin and are very basophilic. In contrast to the granulocytes, which are post-mitotic by the time they reach the peripheral blood, lymphocytes retain the ability to undergo replication during an immune response (more on that later). This means that the peripheral blood will contain lymphocytes of different size, depending on their replicative history (small, medium, and large lymphocytes). This info is provided to you as an explanation for why you will see heterogeneous lymphocyte profiles in blood smears- you will not be required to make this subclassification of lymphocyte morphology.
Lymphocytes are a type of cell that you will find in lymphatic tissue sections throughout the body (some lymphatic tissue is encapsulated like seen in the link below, but often it is scattered, or diffuse, within a tissue). Examine the lymph node at low magnification seen at this link to gain a sense of 1) increased cell density of lymphatic tissues (particularly because of the large amounts of lymphocytes), and 2) the basophilic staining properties of these tissues compared to the cells in the surrounding tissues. Zoom in on the section to examine individual lymphocytes that are outside of the blood stream.
Optional activity: You can practice looking at lymphocytes using a virtual microscope with guiding text in the right panel at this link.
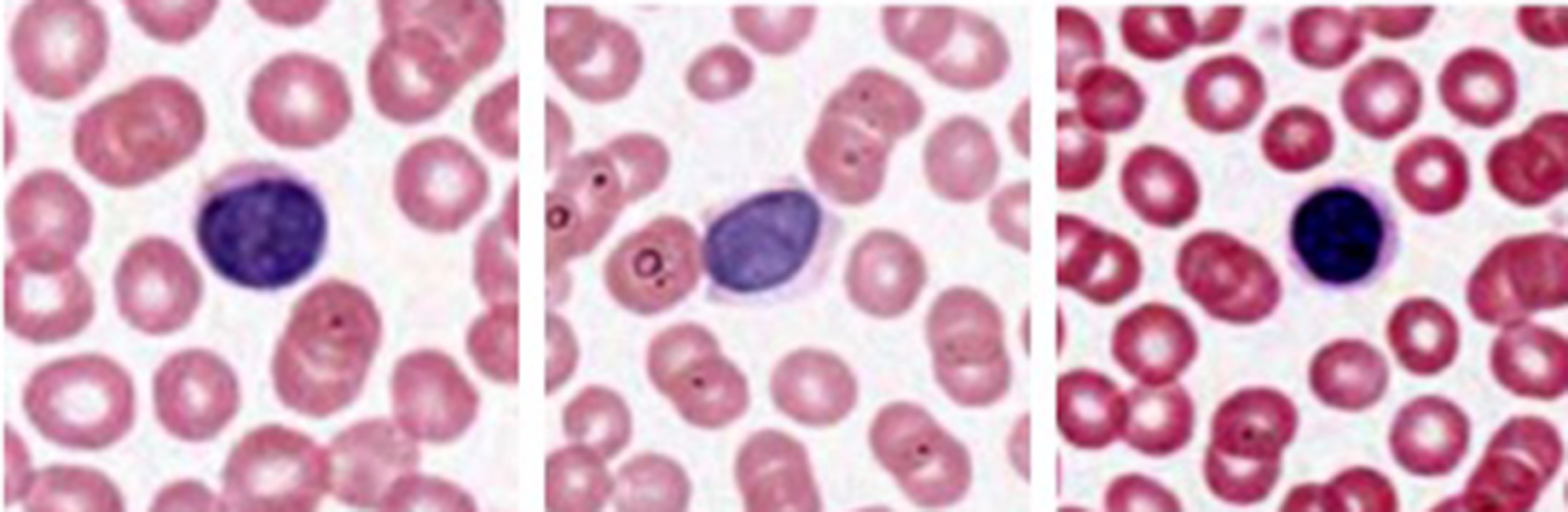
Monocytes
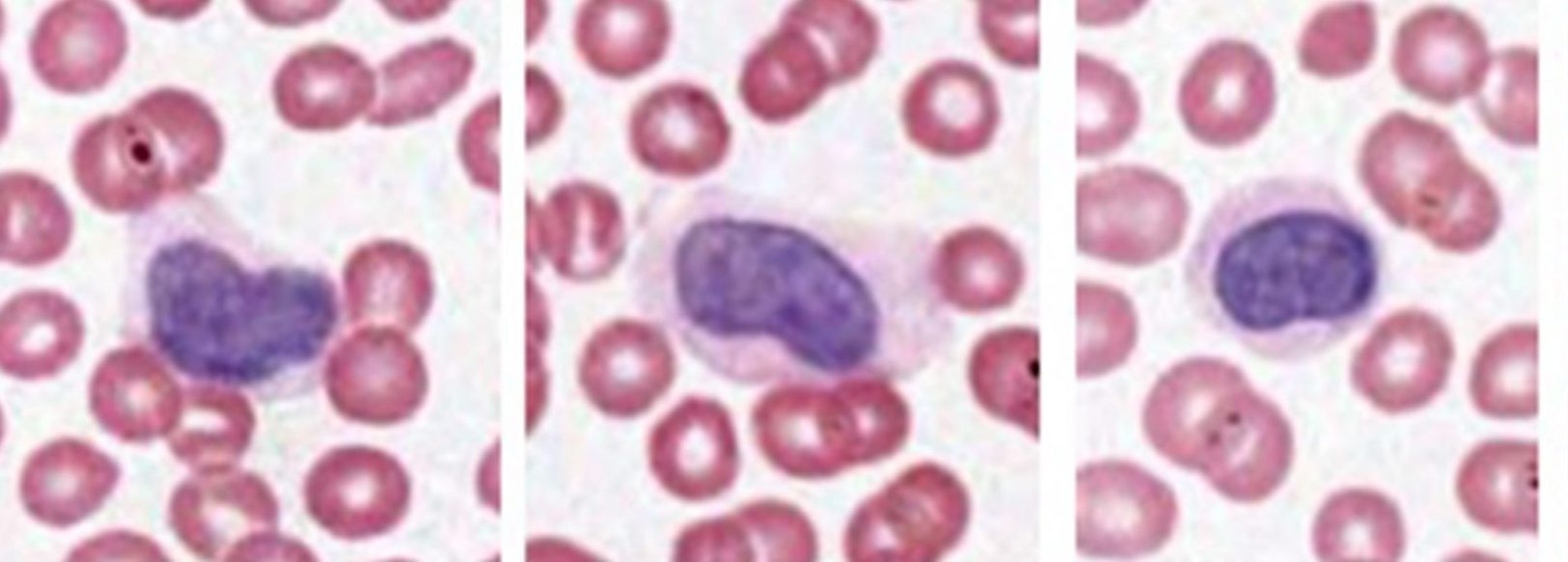
Monocytes are macrophage precursors that circulate in the blood. They can extravasate (leave the blood vessel to enter tissue compartments) to become tissue macrophages. Like lymphocytes, they are mononuclear (not segmented or bilobed). Monocytes are typically larger than lymphocytes and may have a cleft or notch in their nuclei.
Optional activity: You can practice looking at monocytes using a virtual microscope with guiding text in the right panel at this link.
Some Abnormal Blood Cells:
Smear from patient with Chronic Myelogenous Leukemia (CML). The micrograph below highlights some differences from normal and serves to reinforce the expected representation of cells in a normal sample. Scanning this smear at intermediate magnification will demonstrate profiles of cells that resemble immature myeloid cells in the normal bone marrow but are not observed in normal peripheral blood. Lots of immature forms. Other common features in CML include variable elevation in peripheral blood basophils, elevated platelet counts and alterations of erythropoiesis-reticulocytes and normoblasts in the smear.
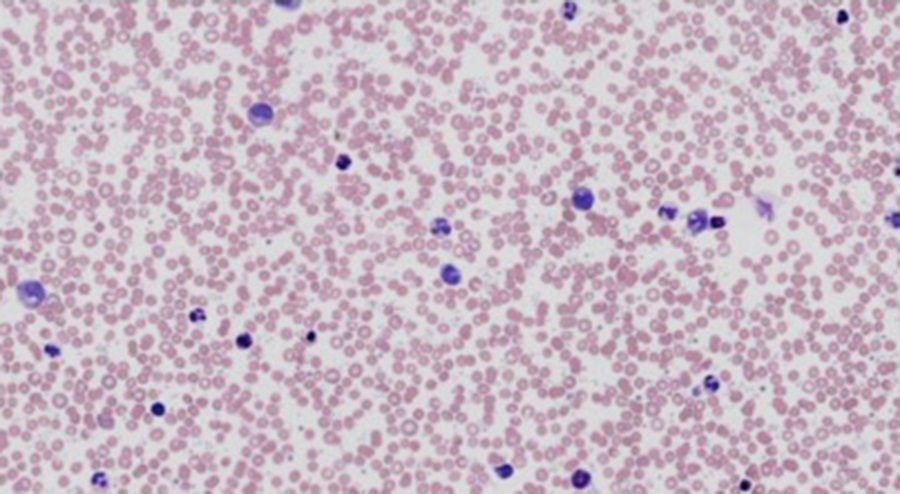
Leukemic cells resembling normal myeloblasts and platelets (basophilic cell fragments in micrographs):
-Very large cells, abundant cytoplasm; nucleus not segmented; variably basophilic cytoplasm reflecting active protein synthesis, modest abundance of granules that stain indistinctly.
Elevated Number of Basophils in the Smear. The most likely explanation if a patient presents with elevated basophil counts is CML. Refer to a hematologist!
Basophils are more readily detected. Note the frequency of platelets in the smear.
Immature Erythrocytes in Peripheral Blood
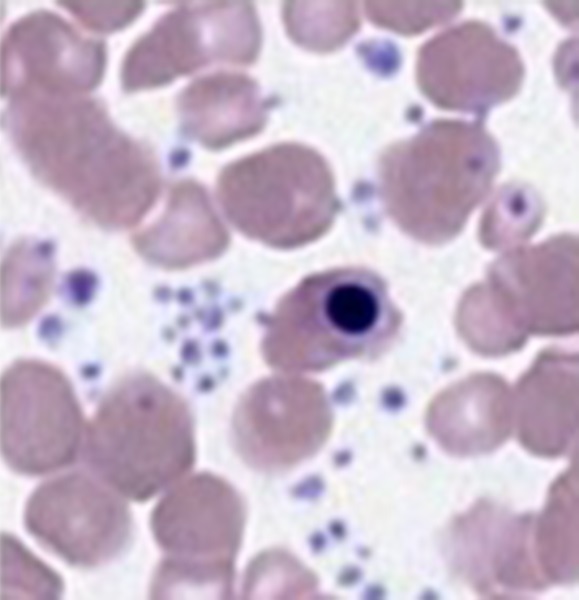
Immature erythroid lineage cells are seen in the peripheral blood in some conditions like anemia. Also note the variability of erythrocyte diameter in the smears and the slightly elevated basophilia in some erythrocytes. What would be one interpretation of these findings related to erythrocytes?
Compare the blood smear of a patient with bacterial sepsis at this link to the case presented in the multiple choice question above.
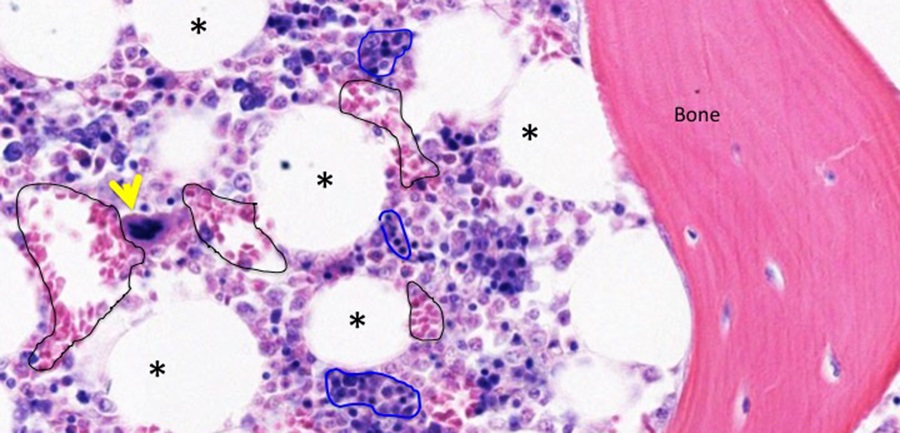
Bone marrow
Stain information: Hemotoxylin and Eosin

This is a plug of bone marrow that has been removed from surrounding bone before subsequent processing. Normally, surrounding bone would make identification of bone marrow trivial. Even without surrounding bone, bone marrow has some characteristic features. At this low magnification, note presence of scattered adipocytes that appear as white spots where tissue processing has extracted fats and lipid from adipocytes.
Slide 14:

The basophilia of bone marrow reflects the high density of nucleated cells with relatively little cytoplasm. Note that the cellularity of bone marrow is comprised of heterogeneous cells that reflect the active hematopoiesis occurring here and the different lineages of cells produced. You will see later that lymphoid tissue is also basophilic, but is of one predominant cell type-lymphocytes. Several large polyploid megakaryocytes (the source of platelets) are indicated by yellow arrowheads. Adipocytes are indicated by asterisks. The eosinophilic structure at lower left is an artery (squamous endothelium forming the lumen and surrounded by smooth muscle. Hash mark is in the lumen.
Optional activity: You can practice looking at megakaryocytes using a virtual microscope with guiding text in the right panel at this link.

Adipocytes are indicated by asterisks and a megakaryocyte is indicated by a yellow arrowhead. An irregularly shaped vascular sinusoid (a type of blood capillary in bone marrow) is outlined in black. Cells of the eosinophilic myeloid lineage can be picked out based on staining and some neutrophilic myloid cells can be identified based on nuclear morphology. Many of the cells with very small round condensed nuclei are normoblasts (nucleated immature RBC). One group is outlined in blue.

This is a sample of bone marrow with associated bone. The presence of spicules of trabecular bone (arrowheads) together with cortical bone and cartilage (arrow) suggests a vertebral body. In this sample, the presence of trabecular bone spicules is an important indicator that the basophilic tissue represents hematopoietic tissue.
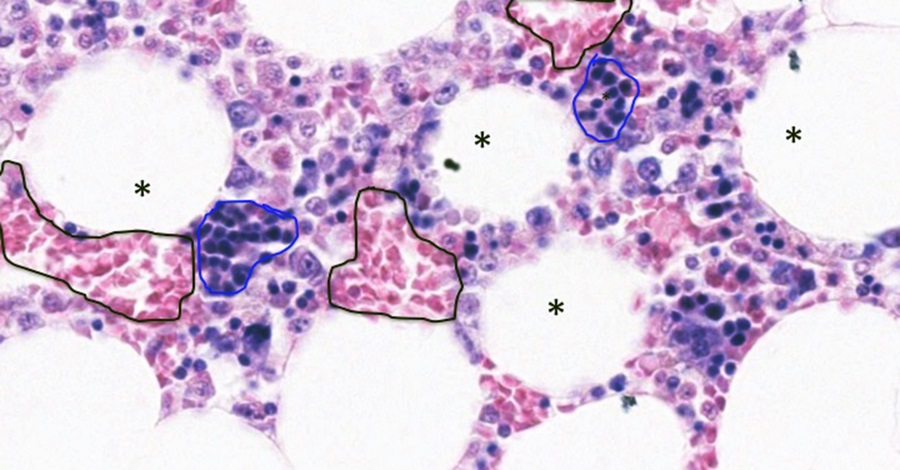
The staining of this sample allows good discrimination between vascular sinuses (filled with blood-mostly RBC; outlined in black) and the surrounding tissue comprised of hematopoietic tissue and adipocytes. The more distal or terminal aspects of erythroid cell development can be seen to good advantage in this sample because these cells have very basic nuclei with eosinophilic cytoplasm. Chromatin of other lineages of cells and the earlier phases of erythroid lineage is not very condensed and doesn’t stain very well. These erythroblastic islands are circled in blue. A megakaryocyte is indicated with yellow arrow and some adipocytes are indicated by asterisks.
This Chapter’s PDF
- Note: The interactive features of this chapter are not reproducible in this PDF format
ARCHIVAL PRE-CLASS MATERIALS FOR THIS SESSION:
- Pre-recorded videos: Basic Concepts of Blood Cells and Their Functions

Feedback/Errata