2 Movement Disorders
Learning Objectives:
Neurology of movement disorders
- Differentiate between hyperkinetic and hypokinetic movement disorders
- List the four cardinal motor features of Parkinson disease
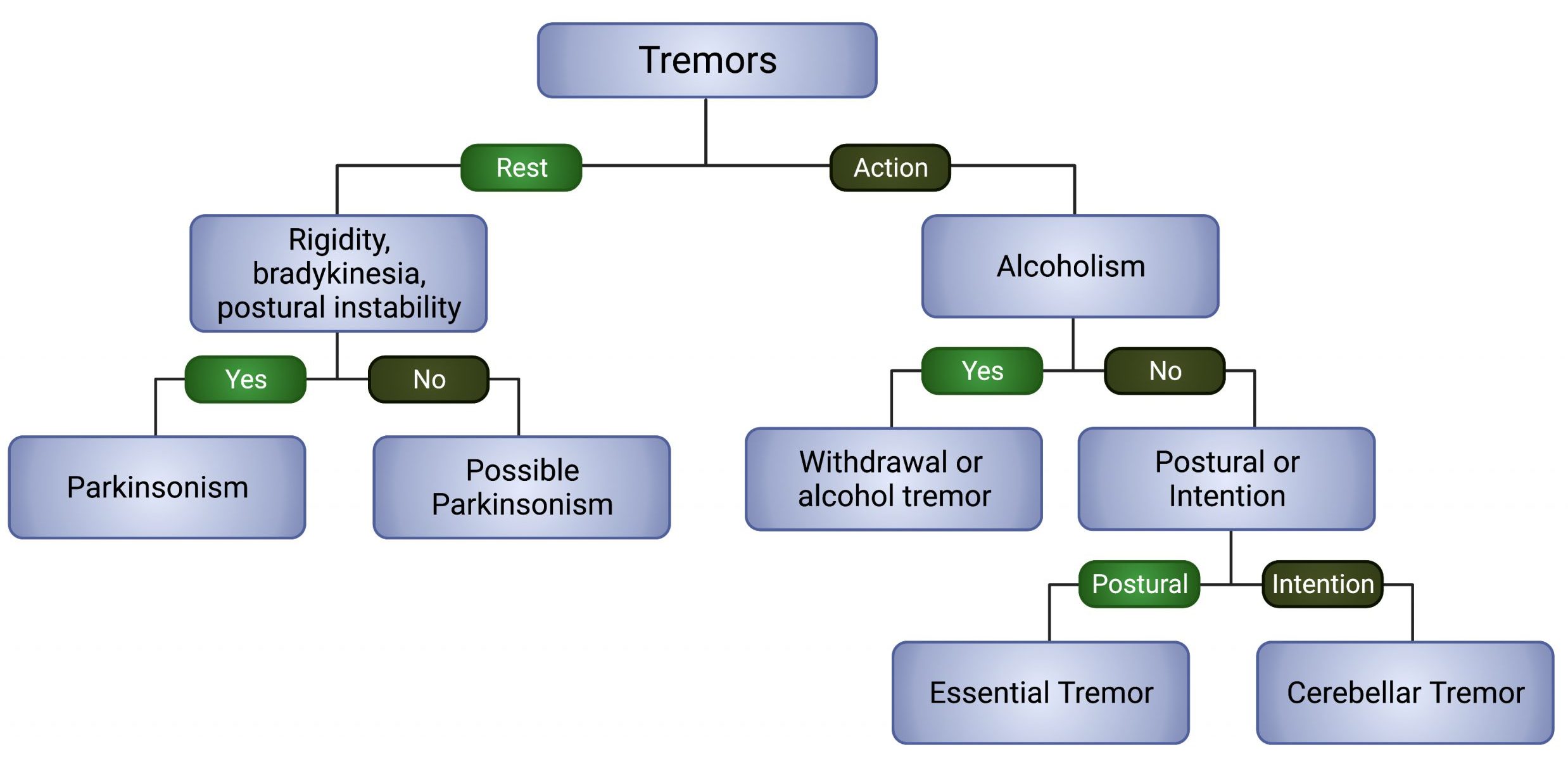
- Describe the differences between tremor types and list the two main treatment options for essential tremor
- List the clinical triad, etiology, and pathology of Huntington Disease
- Describe the clinical features of dystonia and tic disorders
Pharmacology for Parkinson disease and other movement disorders
- Explain the pathophysiology of Parkinson disease and the mechanisms of action of carbidopa/levodopa
- Describe the main side effects of dopamine agonists and monoamine oxidase B inhibitors (MAOB-I)
- Explain how botulinum toxin affects neurotransmission and conditions for which it is used therapeutically
- Explain the pharmacology of tetrabenazine
- Describe the clinical presentation and pathophysiology of Wilson disease and the mechanism for zinc treatment
- List the mechanisms of action, side effects and contraindications the drugs used to treat parkinsonism, tremor, Huntington disease, dystonia, and Tourette syndrome
Table of Contents:
Introduction and Historical Perspective
Hypokinetic Disorders
Hyperkinetic Disorders
Introduction and Historical Perspective:

Movement disorders are neurologic disorders that cause either an excess or a paucity of movement. These abnormal movements can occur at rest or with action, and can be involuntary or suppressible. Based on the presentation or “phenomenology” of the movement disorder, a clinical diagnosis can be made into what type of movement disorder the patient has.

Movement disorders have been described in the literature going back to at least 600 BC in which bradykinesia (slowness of movement) was referenced and treated in ancient India. Charaka (Fig. 1), considered a principal contributor to the ancient science of Ayurveda, described a coherent picture of parkinsonism by describing tremor, rigidity, bradykinesia, and gait disturbance.
In the 1500s, Paracelsus (Fig. 2) used mercury vapor to treat certain conditions. However, he noticed that the mercury exposure caused tremors in some of his patients. If he gave too much mercury vapor, some of his patients died. He made the astute observation that “All things are poison and nothing is without poison; only the dose makes a thing not a poison.” This is shortened to the more well-known adage: “The dose makes the poison.”
In the 1800s an English physician, James Parkinson wrote his famous manuscript “An essay on the shaking palsy” (Fig. 3). This essay describes six patients that James Parkinson either observed on the streets of London or during medical rounds without even examining the patient.
General Classifications:
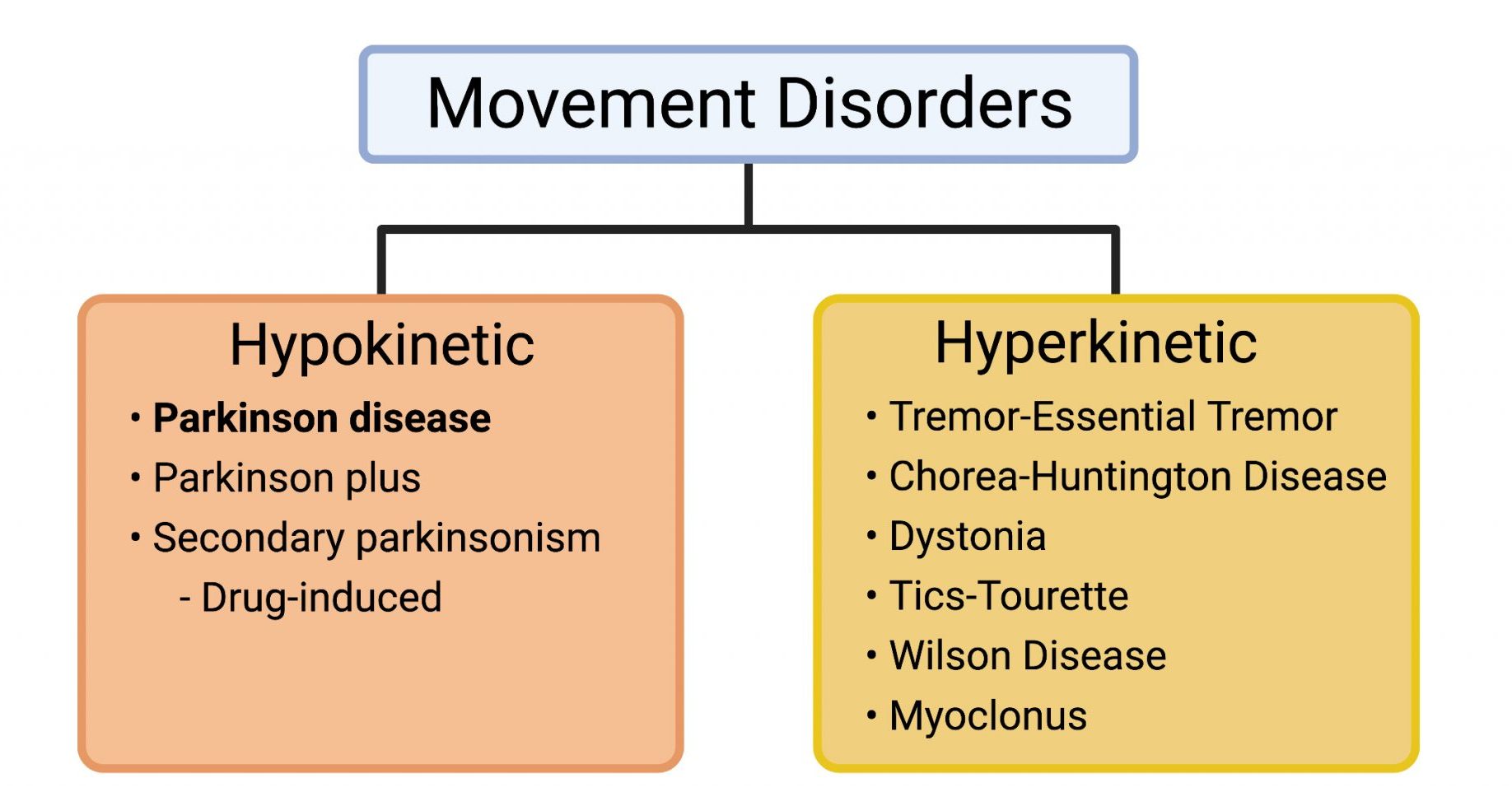
Movement disorders can be classified into two main categories: Hypokinetic and hyperkinetic disorders (Fig. 4).
The main feature of hypokinetic disordersis bradykinesia or slowness of movement. The prototype example is Parkinson disease. In this condition, bradykinesia is one of the four cardinal motor features of this condition and manifests itself in so many ways from small hand writing (micrographia) to the gait (shuffled steps). In general, many of the hypokinetic disorders have at its core principle reduced dopamine neurotransmission. In contrast, hyperkinetic disordersare characterized by an excess of movement. A classic example would be the chorea seen in Huntington disease. Chorea is characterized by involuntary dance-like movements of the body that is probably best described as “fidgety” movements. Some conditions will have features of both hypokinetic and hyperkinetic features (e.g., Huntington and Wilson diseases).
Hypokinetic Disorders:
Parkinsonism:
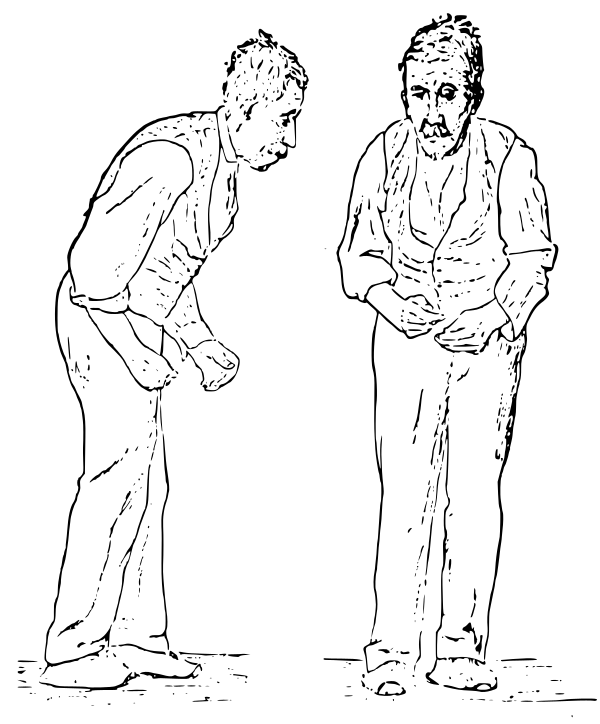
Parkinsonism should not be confused with Parkinson disease (PD). Parkinsonism is a general descriptor used to describe features seen in Parkinson disease such as bradykinesia, muscle stiffness (rigidity), tremor, and postural/gait instability. However, having parkinsonism does NOT always mean a diagnosis of PD. For example, parkinsonism because of haloperidol exposure can be drug induced (secondary parkinsonism). PD is a specific disorder that has both clinical and pathologic criteria for diagnosis. Figure 5 captures the main motor features of parkinsonism showing stooped posture, reduced facial expression (masked facies), shuffling gait, and flexed arms. Parkinsonism can also be due to other Parkinson look-alike disorders. Collectively, these are called “Parkinson-Plus” disorders (Fig. 6):
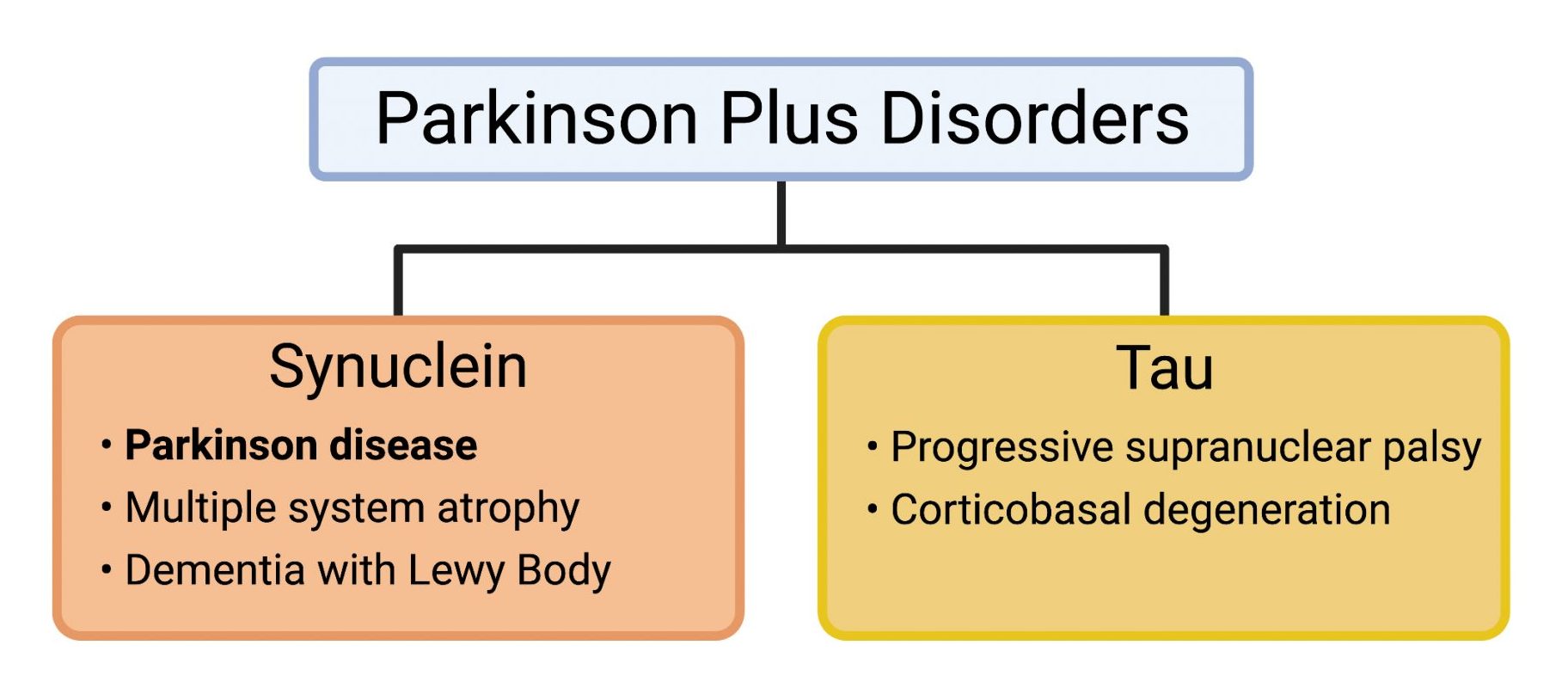
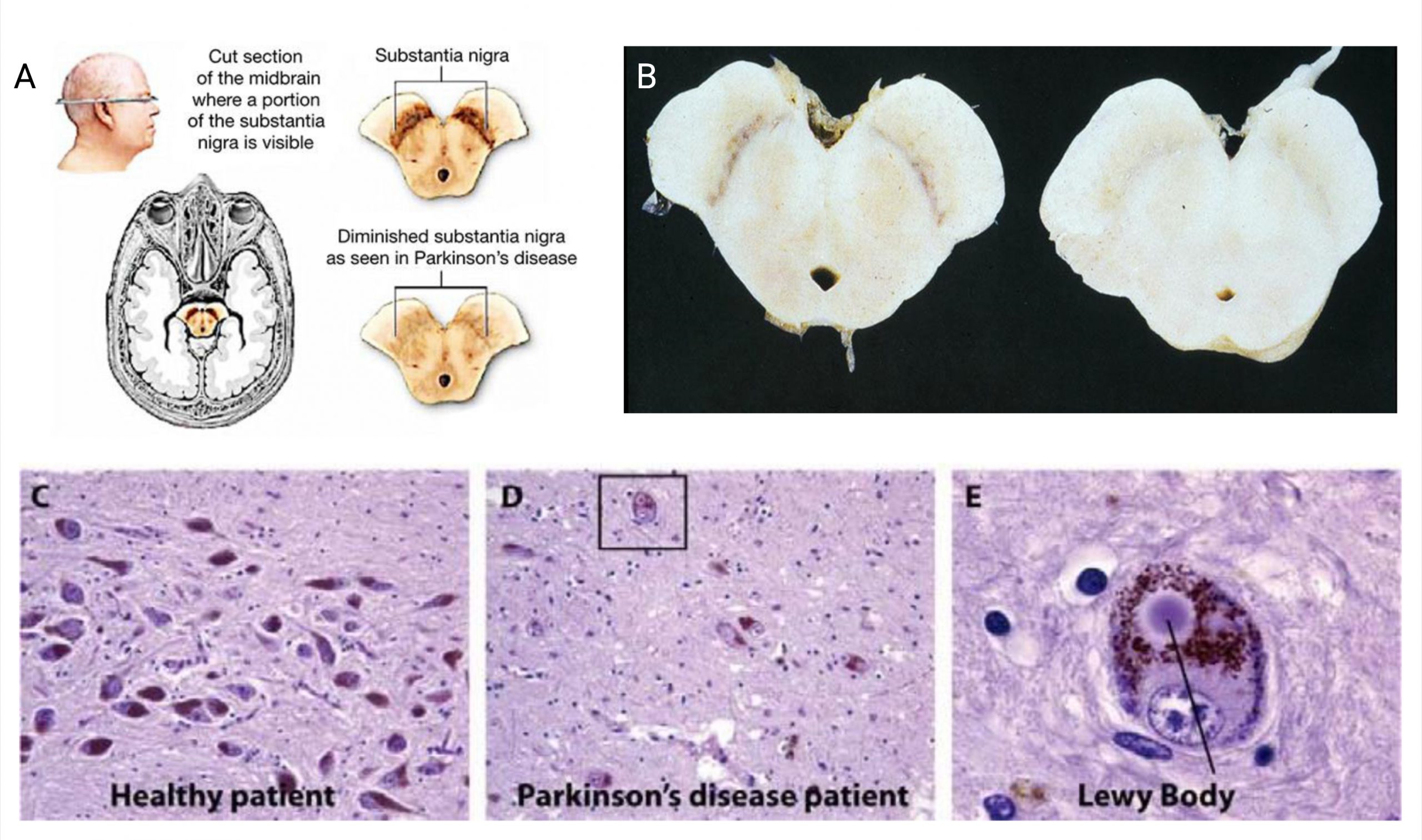
These other Parkinson Plus conditions are classified based on the neuropathologic process. For example, PD, multiple system atrophy, and dementia with Lewy Body all have alpha-synuclein protein aggregates in the brains (Fig. 7). This differs from the other conditions in which tau protein aggregation is the main process.
Parkinson Disease:
Key Facts:
- Second most common neurodegenerative disorder (after Alzheimer disease)
- Due to degeneration of dopamine (DA) neurons in the substantia nigra that project to the basal ganglia (Fig. 7A and B).
- Affects 1% of population > 60 yearsold.
Pathophysiology and etiology:
Loss of dopamine (DA) from the substantia nigra effects both the direct and indirect pathways. In the direct pathway, loss of DA leads to decreased stimulation of the striatum, causing a decrease in the inhibition of the GPi. This decreased GPi stimulation then causes an increase in inhibition to the thalamus. Increased inhibition to the thalamus decreases activation of the cortical motor areas, leading to hypokinetic movements.
The loss of DA in the indirect pathway leads to a decrease inhibition in the striatum. This leads to an increased inhibition of the GPe, which then reduces inhibition of the STN. This increases STN stimulation of the GPi, which leads to increased inhibition of the thalamus. Decreased output of the thalamus leads to a decrease in cortical activation, and thus suppresses movement.
Figure # – Image slider showing the effects of Parkinson’s disease on the direct and indirect pathways. The loss of dopamine from the substantia nigra pars compacta leads to a decrease in activation of cortical motor areas, and thus hypokinetic movements.
Risk Factors (selected):
- Environmental: Pesticide.
- Genetic: GBA (acid beta-glucocerebrosidase) mutations are the most common mutation in sporadic cases.
- Pre-motor symptoms: Anosmia (loss of smell) and REM sleep behavior disorder (acting out and talking in sleep during REM sleep)
- Can precede the onset of motor symptoms by 10-20 years.
- REM sleep behavior disorder is more specific to PD than to other neurodegenerative conditions and is considered a risk factor for the development of this condition later in life.
Clinical presentation and signs: Four cardinal motor features
Mnemonic-TRAP–Tremor, Rigidity, Akinesia, Postural/Gait instability
PD diagnosis is dependent on a collection of classic motor symptoms that is featured in the majority of diagnostic classifications:
- Tremor: Defined as an oscillatory, rhythmic movement of a body part. Usually a resting tremor (body position fully supported) but can also include other tremors (postural and kinetic). Frequency is usually 4-6 Hz and the classic description is a “pill-rolling” tremor. See Parkinson disease tremor video.
- Rigidity: Increased muscle tone that classically presents as cog-wheeling phenomenon (at the wrist) and lead pipe rigidity (at elbow). See Parkinson disease rigidity video.
- Akinesia/bradykinesia: Slowness of movement that can range from mild to very severe (akinesia). Considered the sine qua non for parkinsonism and PD. Manifests in many different ways including:
- reduced voice volume (hypophonia),
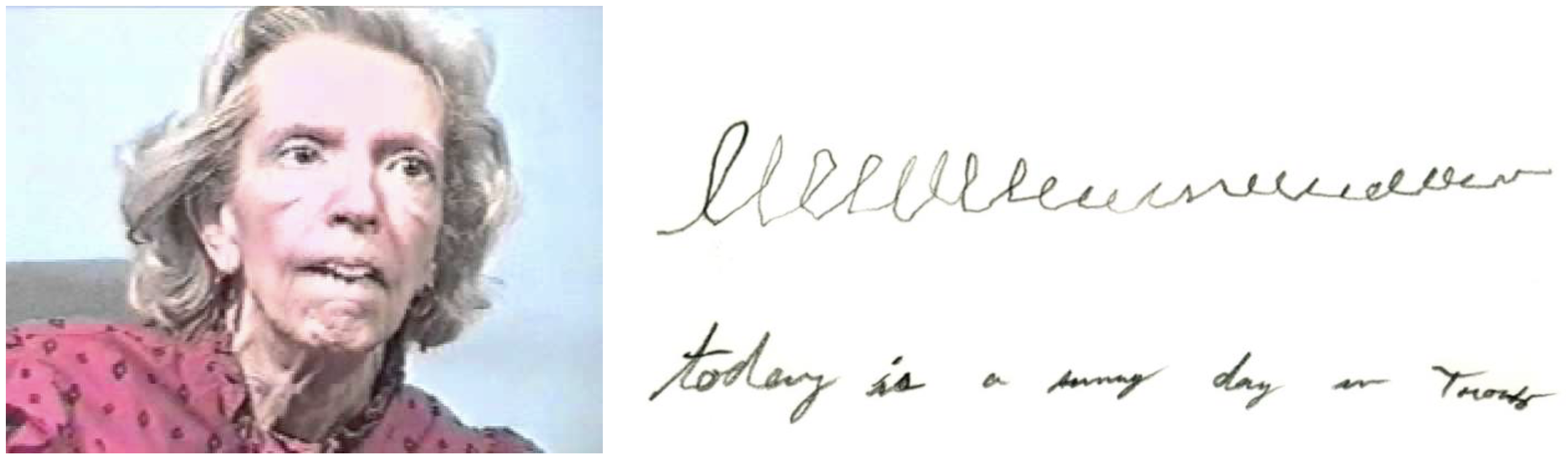
- reduced facial animation (hypomimia, Figure 8)
- small handwriting (micrographia, Figure 8)
- shuffled gait
- reduced limb dexterity
- drooling
- reduced blink
- Postural/gait instability: Loss of postural reflexes results in frequent falls. Gait changes include stooped posture, shuffling stride length, festination(increased speed of walking resulting in fall), en blocturning (multiple steps to turn), and freezing of gait.
Parkinson gait video from UC Dublin
Parkinson gait: Freezing & other features
Treatment:
All pharmacologic treatments for PD are symptomatic. No drugs available commercially have been proven to be “neuro-protective” in PD.
In general, there is no strict rule about when and how to treat PD. However, below are some basic guidelines:
- Timing: Consider how symptoms interfere with quality of life and activities of daily living (ADLs). For someone who is very active and still working, earlier treatment usually is chosen.
- Which drug to use: The side-effect profile and co-existing symptoms can help in decision making. For patients with cognitive impairment, avoid dopamine agonists due to behavioral and cognitive side-effects. If taking a SSRI or other serotonergic inhibitor, avoid monoamine oxidase-B (MAO-B) inhibitors (rasagiline).
PD medications can be broken down into 3 major categories for the purpose of this course: MAO-B inhibitors, dopamine agonists, and levodopa.1
Levodopa (L-DOPA) crosses the blood-brain barrier where it is taken up by the dopaminergic neurons and converted to dopamine. In the periphery, levodopa can also be converted to dopamine causing side effects. To counter-act these effects, carbidopa (a peripheral DOPA decarboxylase inhibitor) is co-administered.
1See Katzungand Trevor Figure 28.2 for important details on mechanism for carbidopa/levodopa pharmacology.
(Link Error – off campus denied)
Surgical options:
Deep Brain Stimulation (DBS) is a FDA approved surgical treatment option for PD and other movement disorders. The target of DBS therapy in PD is typically the subthalamic nucleus (STN). The globus pallidus internus (GPi) is also a target in PD. This video shows a patient with the stimulation off vs on.
Hyperkinetic Disorders:
Tremors:
Tremor is defined as an oscillatory and rhythmic movement (although can also be arrhythmic in certain tremors) movement:
The causes for tremors are extensive. It is normal to have a physiologic tremor in the body.2 Enhanced physiologic tremor due to a side effect of medications is also very common. Classic medications causing tremors include lithium, valproic acid, beta agonists, steroids, and selective serotonin re-uptake inhibitors. Hyperthyroidism can also enhance tremors and thus TSH should be checked. It is important to note that a condition can have more than one tremor type. For example, it is common for PD patients to have both a resting and action tremor.
2As an experiment, place a piece of paper on your hand with your arm in front of you and you will see the paper shake (more if you have a lot of caffeine)
The tremor types are:
- Rest tremor: Tremor that occurs when affected body part is fully supported and relaxed
- Arm resting on leg
- Prototype is Parkinson resting tremor
- Action tremor: Broad term that encompasses a tremor with movement
- Postural tremor: Occurs when muscles activated against gravity w/o movement
- Arms outstretched in front without movement
- Prototype is Essential Tremor
- Kinetic tremor: Tremor that occurs with movement of a body part
- Finger to nose testing Finger-to-nose test video
- Intention tremor: Tremor occurs near the target. Usually associated with a cerebellar process
- Postural tremor: Occurs when muscles activated against gravity w/o movement
Essential tremor:
Essential tremor (ET) is the most common adult-onset movement disorder worldwide. Age of onset follows a bimodal peak distribution with the 2nd and 6th decades occurring most frequently. Family history varies from around 20 to 60% of cases and follows an autosomal dominant pattern. The tremors usually affect the head (either yes-yes or no-no direction) and hands the most frequently (see Essential tremor video with deep brain stimulation off and on). An important clue is the response to alcohol—alcohol is often associated with an improvement in the tremors. Sometimes, this association is so strong that some individuals unfortunately become alcoholics.
An important learning tip is to remember that not all causes of action tremors is ET. ET is a specific diagnosis and should NOT be used as a descriptive term. For example, if a patient has prominent action tremors in her arms but is on lithium and does not have any family history of tremors, then the likely diagnosis is enhanced physiologic tremors secondary to lithium and NOT ET.
There are pharmacologic and non-pharmacologic (surgical) treatment options. If the tremors are not too severe, then adaptive devices might be helpful in making everyday activities more tolerable. A good example is the Liftware® spoon. DBS is another FDA indication for the treatment of ET. There are two, Class A evidence medications used as first-line options for the treatment of ET (See Table 2):
Chorea
Key Facts:
- Chorea is a hyperkinetic dyskinesia that results in quick (although not as fast as myoclonus) purposeless, involuntary, non-stereotyped movements that flow from one body part to another.
- Chorea means “to dance” in Greek – Chorea Video
Differential: There are many causes for chorea, but the more common causes are
- Drug-induced (PD meds like levodopa)
- Immune-mediated (Anti-phospholipid syndrome)
- Post-infectious (Sydenham’s chorea)
- Neurodegenerative (Huntington disease)
Classic feature found in chorea:
- Motor impersistence-inability to maintain ongoing muscle activity: Tongue protrusion, “milk-maid’s grip”.
Huntington Disease
Key Facts:
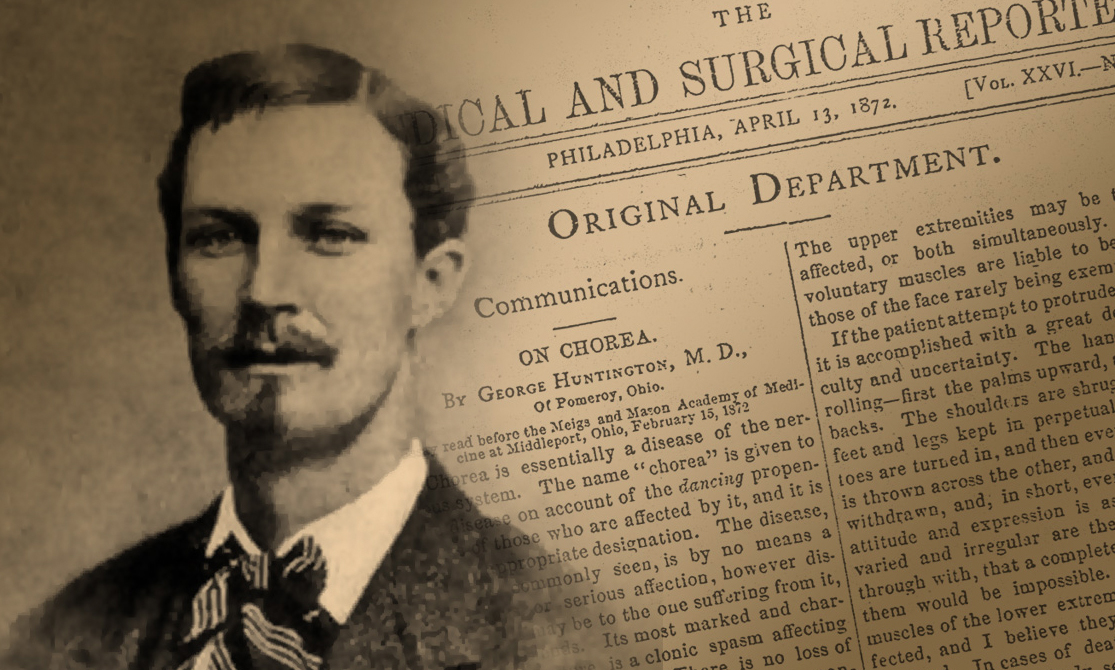
- Most common hereditary cause for chorea.
- Named after George Huntington, an American physician who described the abnormal movement in his manuscript “On Chorea” in 1872 after graduating from Columbia Medical School
Main pathophysiology is degeneration of medium spiny neurons in the striatum (GABAergic efferent projections)
Pathology:
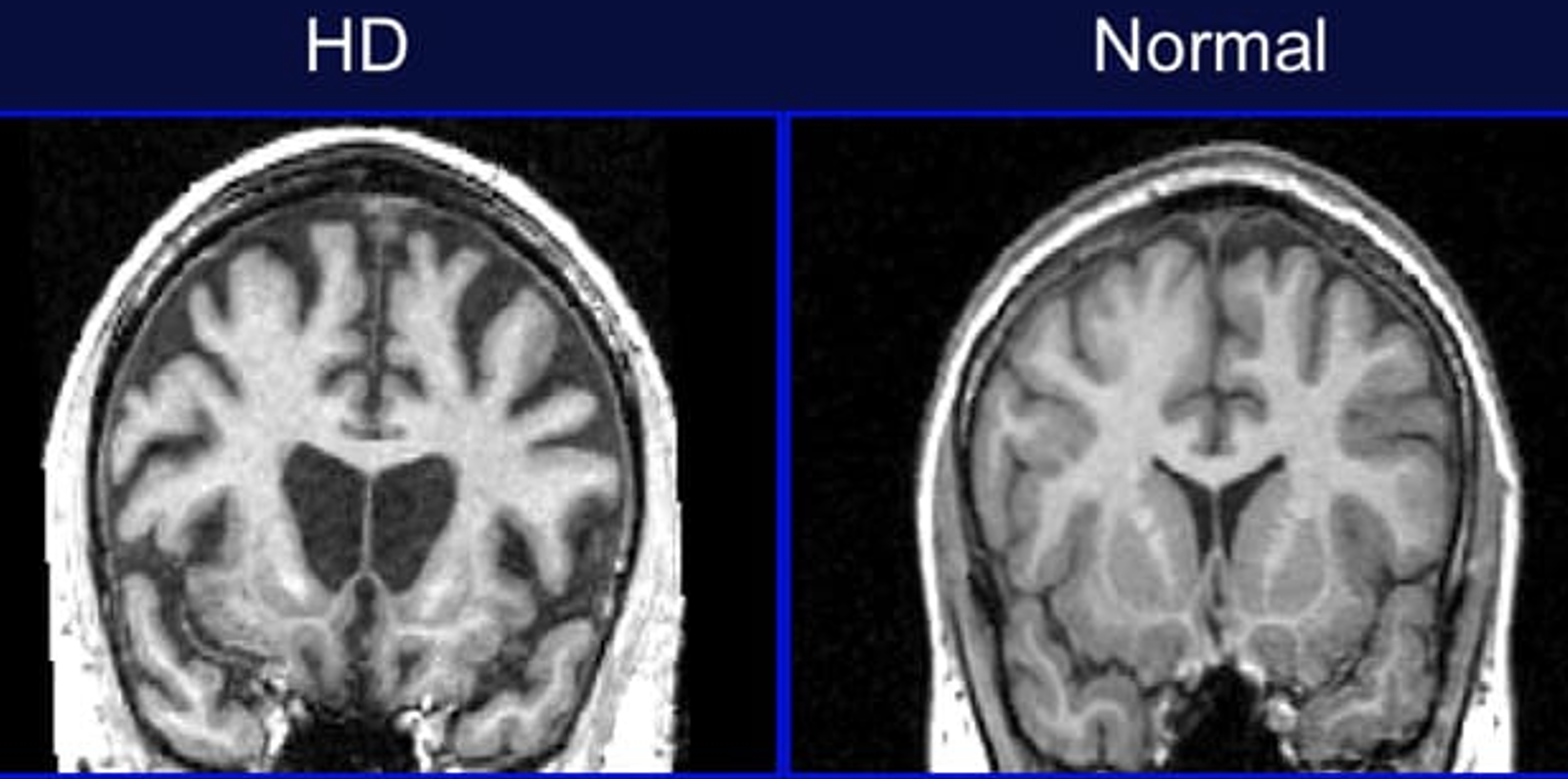
Bilateral caudate atrophy in Huntington disease patient.
Characterized by a clinical triad of:
-
- Movement disorder, predominantly chorea, but can also present with:
- Parkinsonism
- Dystonia
- Ataxia
- Myoclonus
- Psychiatric symptoms:
- Depression
- Irritability
- Psychosis
- Cognitive decline
- Movement disorder, predominantly chorea, but can also present with:
- Genetics: Autosomal Dominant, CAG trinucleotide repeat.
- Normal < 29 repeats.
- No risk for repeat size 30-35, but offspring increased risk.
- Intermediate Risk 36-39 (Incomplete penetrance).
- >40 repeats is 100% penetrant.
- Anticipation: The higher the number of repeats, the more severe and earlier onset of disease
- Paternal transmission is more unstable and results in significantly higher repeat size in offspring
- Treatment: Treatment is purely symptomatic; there are no proven neuroprotective drugs for Huntington disease. The focus of treatment should rely on a multi-disciplinary approach with medications as well as rehab services including physical, therapy, occupational therapy, and speech therapies. Social work is critical since this population is at risk of homelessness.
- For chorea management, the goal is to reduce the presumed excess in the basal ganglia output. This is achieved by reducing dopamine transmission. Classically, this was achieved by blocking post-synaptic dopamine receptors with neuroleptics (typical or atypical see Table 3).
Medications of the treatment of chorea:
To avoid complications arising from blocking post-synaptic dopamine receptors (e.g., tardive dyskinesia), reducing dopamine transmission pre-synaptically is another option. Monoamine depletors such as tetrabenazineachieve this by preventing the packaging of monoamines (dopamine, serotonin, norepinephrine) into the presynaptic vesicles through its effect on the transporter, VMAT2.
Hemiballimus:
Definition:
- Ballimus describes wild, flinging movement that appears more violent than chorea.
- Hemiballimus affects only one side of the body.
Pathophysiology:
- Hemiballimus is most frequently caused by a stroke in the subthalamic nucleus caused by blockage of a penetrating branch off the posterior cerebral artery and affects the contralateral side.
Wilson disease (WD)
Key Facts:
- Autosomal recessive hepatic and neurodegenerative disorder due to an inborn error in copper metabolism.
- The gene responsible for this condition doesNOT encode for ceruloplasmin, but a copper transporter, Copper-binding P-type ATPase, ATP7B. This copper transporter is responsible for transportation of copper in these 2 main functions:
- Copper incorporation into ceruloplasmin precursor, apoceruloplasmin
- Copper transportation into the bile canaliculus for excretion
Pathology:
- Excess copper in hepatocytes damages mitochondria, which produces oxidative damage to cells and allows spillage of copper into the blood, thereby overloading other organs such as the brain
- The main areas of the brain affected in WD are the lenticular nuclei, which macroscopically appear brown in color because of copper deposition
Clinical Presentation: The “Great Masquerader” Wilson disease video
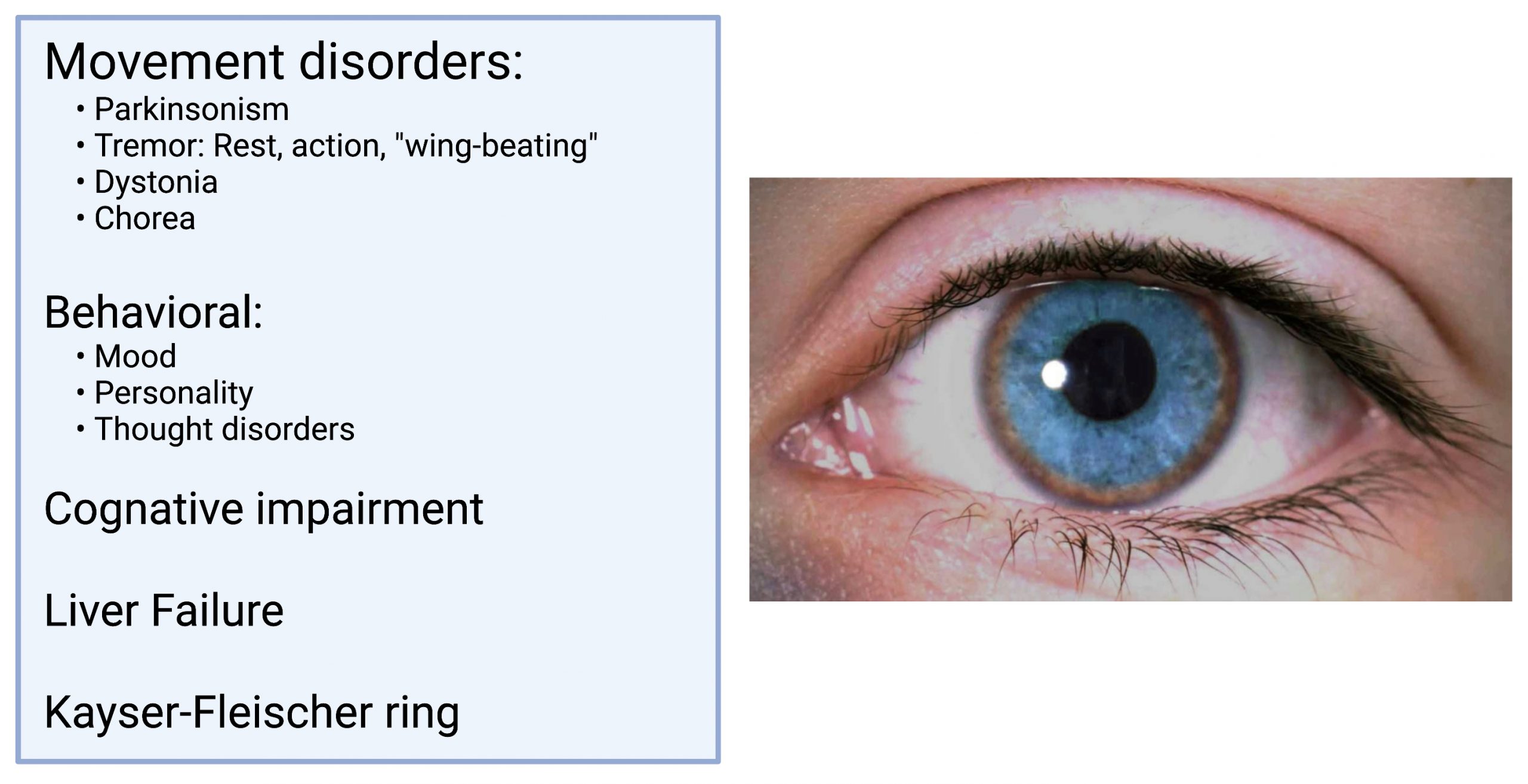
Diagnosis: The INCORRECT assumption is that serum copper/ceruloplasmin is increased.
| Serum Copper | Serum Ceruloplasmin | 24 Urine Copper | Liver Copper |
Treatment: There is presently no cure for this condition. The primary goal is to reduce copper levels. The main drugis zinc, but also trientine and D-penicillamine. Zinc blocks copper uptake. See Copper & zinc metabolism powerpoint -very important (Broken link in syllabus)
Dystonia:
Dystonia is defined as a syndrome of sustained muscle contractions, frequently causing twisting and repetitive movements or abnormal postures. The distribution of dystonia can vary from focal (Cervical Dystonia video with sensory trick), segmental (Meige Syndrome), multi-focal, and generalized.
Key Facts:
The most common clinically encountered cause is a drug-induced dystonia, i.e., acute dystonic reaction. This is seen most commonly in response to acute blockade of dopamine receptors (metoclopramide given in the ED for nausea).
Dystonias can often appear bizarre and have features commonly associated with non-physiologic causes. These include being very task-specific or very position dependent. Also, the consistency of dystonia can vary and give the impression of distractibility. Before a genetic cause was discovered for dystonia, it was thought to represent a psychogenic etiology.
The most common acquired adult-onset dystonia is cervical dystonia, a focal dystonia of the neck.
Treatment:
For focal dystonias, botulinum toxin injections are the most effective treatment. Medications such as anti-cholinergics, benzodiazepines, and muscle relaxants can also be beneficial. Dopa-responsive dystoniais the result of a neurochemical defect in the synthesis of dopamine, resulting in childhood onset dystonia that usually starts in the distal legs. Small doses of levodopa are effective in reversing the symptoms of this condition. Table 4: Medications for dystonia
Botulinum toxin:
FDA approved treatment for focal dystonias. Botulinum toxin prevents the release of acetylcholine at the neuromuscular junction—preventing neuromuscular transmission (see Figure 14). The end result is transient, local weakness/paralysis of the injected muscle. See Botulinum toxin Pharmacology video
Tics:
Tics are defined as recurrent, intermittent, stereotyped, semi-voluntary movements or sounds associated with an urge.
Core clinical features:
- Urge: A compulsion or desire to make a movement or sound
- Suppressibility: Patients can temporarily control the tics for a variable period of time
- Motor tics: These can range from simple (e.g.nose twitch) to more complex motor tics (e.g., copropraxia—showing the middle finger)
- Vocal tics: These can range from simple (grunting) to more complex vocal tics (e.g.,coprolalia—profanities).
- Semi-voluntary is a movement that is initiated in responseto an internal stimulus. A good example of this would be restless legs in which the person will describe an urge to move their legs while seated with an improvement in this urge once walking.
Tourette Syndrome:
Key Facts:
- Defined as a tic disorder > 1 year in duration
- Combination of both motor and vocal tics
- Symptom onset before 18 years old
- Psychiatric symptoms will often co-exist. These can range from obsessive-compulsive disorder (OCD) to attention deficit spectrum (ADD/ADHD) behaviors. Tourette syndrome video
Treatment:
Treatment only if the tics bother the patient (not caregiver). Similar to chorea, TS is considered a hyperkinetic disorder. Therefore, reducing DA transmission isone treatment option for TS.
TL/DR
Neurology of movement disorders:
1. Hyper vs hypo kinetic
Hyperkinetic – Excess of movement
Hypokinetic – Slowness of movement
2. The four cardinal motor features of Parkinson disease are: TRAP
Tremor
Rigidity
Akinesia/bradykinesia
Postural/gait instability
3. The differences between tremor types and list the two main treatment options for essential tremor
Rest tremor occurs when resting
Action tremor occurs with movement
4. The two main treatment options for essential tremor
Propranolol – Non-selective β-blocker
Primidone – Enhances GABA activity
5. The clinical triad, etiology, and pathology of Huntington Disease:
Clinical Triad:
Movement disorders
Psychiatric symptoms
Cognitive decline
Etiology:
Genetics – CAG trinucleotide repeats
Pathology:
Bilateral caudate atrophy
6. The clinical features of dystonia and tic disorders
Dystonia – sustained muscle contractions, frequently causing twisting and repetitive movements or abnormal postures
Tic disorders – recurrent, intermittent, stereotyped, semi-voluntary movements or sounds associated with an urge
Pharmacology for Parkinson disease and other movement disorders:
1. Pathophysiology of Parkinson disease
Loss of dopamine in substantia nigra
2. Mechanisms of action of carbidopa/levodopa
Levodopa converted into dopamine
Carbidopa keeps it from getting metabolized in the periphery
3. Main side effects of dopamine agonists and monoamine oxidase B inhibitors (MAOB-I)
Dopamine agonists: Hallucinations, sleepiness, edema
MAOB-I: Insomnia, Dizziness
4. How botulinum toxin affects neurotransmission and conditions for which it is used therapeutically
Prevents release of acetylcholine
Dystonia
5. The pharmacology of tetrabenazine
VMAT2 inhibitor – ↓SN DA signaling in the striatum
6. Clinical presentation and pathophysiology of Wilson disease and the mechanism for zinc treatment
- Movement disorders:
- Parkinsonism, Tremor, Dystonia, Chorea
- Behavioral
- Mood, Personallity, Thought disorders
- Cognitive impairment
- Liver failure
- Kayser-Fleischer ring
Zinc blocks copper uptake
7. List the mechanisms of action, side effects and contraindications the drugs used to treat parkinsonism, tremor, Huntington disease, dystonia, and Tourette syndrome
Check out the Pharm Page for all the drugs
