6 Transradial Prosthesis Project Critique Guidelines
The project critique is based on two interdependent goals
| 1) Technical Goals | 2) Functional goals |
|
|
The following 12 guidelines provide a step-by-step process to evaluate the adequacy of the prosthesis.
- Professionalism
- Safety
- Bench test
- Socket fit
- Tissue fit and anatomical landmarks
- Trimlines and ROM
- Load test – test stability of the socket fit, efficiency and comfort
- Modify the trimlines to allow the balance the ROM and load needs, as necessary
- Joint axis location
- Length
- Alignment of the forearm component
- Harness checkout
- TD opening and closing
- Quality of fabrication, fit and function
- Comprehension
- Patient-centered context and functional goals/outcomes
12 Guidelines Explained |
1) Professionalism
- Preparedness
- Read appropriate readings, review clinical evaluation skills and practice taking a history, knows what is expected of them, has a check list of what needs to be done and the appropriate evaluation forms, etc.
- Gentle treatment of the pt
- Greet pt respectfully, explain what you plan to do before you do it, pay attention to pts eyes for signs of irritation, etc.
- Your words, actions, appearance and body language
- ***Before fitting, check that all edges and the inside of the socket are smooth.
- Begin the fitting procedure with care. Some patients go home at the end of a fitting in more irritation than when they came in.
2) Safety
- Universal precautions taken.
- Action taken to reduce risk of injury to pt, others and self.
3) Bench test: Check efficiency of control system and operation of components (see images ) You should do this BEFORE the patient comes in for fitting.
- Check the harness
- The ends of all Dacron should be singed to prevent fraying of the fabric.
- The largest loop on the 4-bar buckle goes toward the ring.
- Standard: flexible hinges should be secured 2.5cm proximal to wrist (to allow maximum pronation/supination).
- Location of base plate and retainer
- 2.5cm distal to trimline at the anterior/lateral quadrant, close to elbow joint center for mechanical advantage and to save shirts.
- Check the housing length:
- full ROM of TD in pronation and supination.
- no stretching of the housing when the elbow is in full extension between baseplate and crossbar.
- 2cm of housing proximal to the crossbar to prevent strain.
- NO sharp bends.
- Check the cable length:
- long enough to allow full ROM of pronation and supination without activating the TD.
- fittings crimped or soldered without concentrating bending forces at transition.
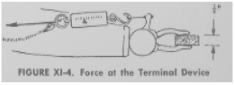
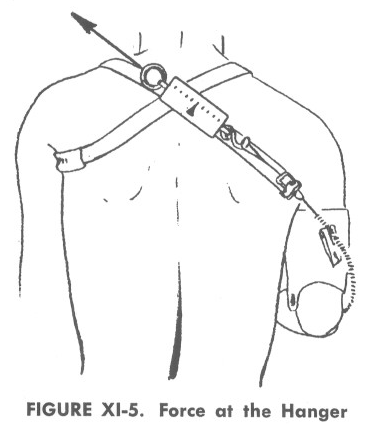
- Measure the control system efficiency:
- Efficiency = Force at TD/Force at harness
- Standard: At least 80% for single control harness
- Standard: At least 50% for dual control harness
|
Measure control system efficiency:
 |
 |
|
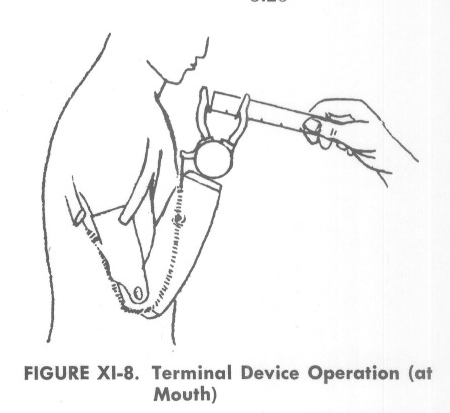
Technical Operation of TD: Assess technical operation of prothesis by user. |
 |
4) Socket Fit
The upper limb prosthetic socket provides six distinct purposes: 1) it provides a solid purchase on the residual limb; 2) it extends control function for the individual; 3) it provides fixation of components; 4) it provides for movement and direction; 5) it transmits force and displacement of the components; and 6) it provides a source of energy and excursion.
When evaluating the socket, you need to ensure that the socket provides a solid purchase, which distributes pressure over large areas of soft tissue and relieves bony prominences. Your clinical evaluation of the socket fit involves 4 phases a) tissue fit and anatomical landmarks, b) evaluate the trimlines and ROM, c) load test – test stability of the socket fit, efficiency and comfort, and d) modify the trimlines to allow the balance the ROM and load needs, as necessary.
Importantly, the socket should be comfortable with and without loads applied in all ranges of motion. Socket Comfort Score is one method to assess the individual’s perspective about the comfort of the socket. Administer this question at the end of the appointment after you have finished all your modifications.
- Tissue fit and anatomical landmarks
Try the socket on the patient; observe the location of the anatomical landmarks and check for total contact, snug, yet comfortable fit. Always start by checking a bony reference to make sure the socket has the proper axial location and rotation orientation by referring to your bony reference (humeral epicondyles and/or olecranon). You may want to mark a dot on the check socket that corresponds to a bony reference so that you don the socket on the patient’s limb the same way each time.
Check for total contact, snug, yet comfortable fit. If the socket is too loose, add appropriate socks so it is in the correct place. The socket should fit so that the anatomical landmarks (olecranon, humeral epicondyles, distal radius/ulna, biceps tendon) are located appropriately within the socket.
The location of the bony landmarks may change with fluctuating limb volume. There is a close relationship between how the tissue fits in the socket and the location of the bony landmarks.
- Trimlines and ROM
***When checking the ROM, gently load the socket as it will be used to observe the fit.
Adjust the trimlines so they do not impede the range of motion. If the ROM is within functional limits, flare the edges to relieve edge pressure before trimming.
|
Standards |
Flexion |
Pronation/ Supination |
|
Active ROM |
0-150`
|
85-90` / 85-90’ |
|
Flexible hinges |
within 10` of active ROM |
Half of the residual ROM |
|
Rigid hinges |
within 10` of active ROM |
Restricted |
|
Self-Suspension |
~105-110` |
Restricted |
Anterior trimline
- Biceps tendon located at the anterior brim when in the correct flexion position.
- No more than 50% of arm should be exposed.
|
|
Medial/Lateral Trimlines |
Posterior Trimline
|
|
Flexible Hinges |
Follows a gentle arc from posterior to anterior while allowing maximum supination. |
Encompass the olecranon for protection.
|
|
Rigid Hinges |
Encompasses the epicondyles to locate elbow center. |
|
|
Self-Suspension |
Encompass the epicondyles at the level of the P-M-L with enough of a brim to flare the soft tissue. Standard: 25mm proximal |
Trimline should extend about 2.5-5cm above olecranon to capture the triceps bar. |
Elbow flexion/extension
- Standard with rigid hinges: within 10` of active elbow ROM
- Standard with self-suspension: ~105-110` elbow flexion
- The socket should not migrate distally in flexion. Observe the movement of the olecranon in the socket; it should remain in the socket.
- In flexion, if the socket is migrating distally, determine if it is the tendon, or soft tissue. The movement of the socket may be due to one of the following issues:
- Anterior trimlines may be too high.
- Anterior trimlines may be too low, resulting in tissue bunching. If so, more relief in the antecubital area may be needed to accommodate the tissue inside the socket.
- Olecranon relief may be too distal giving a false impression of socket movement. Reassess the location of the bony anatomy with socket donned at 90’ elbow flexion.
- Inadequate relief at olecranon or the overall length of the socket may be too short.
- or decide to limit the range for socket coverage and transmission of force.
- In extension, check that the posterior trimline does not impinge on the triceps in elbow extension.
Supination/ Pronation
- Flexible hinges:
- Standard: Rotation of the prosthesis should be half of that with the prosthesis off.
- Rigid hinges and self-suspension: Trimlines/hinges encompass the humeral condyles, so supination and pronation are restricted
Load test – test stability of the socket fit, efficiency and comfort
When evaluating the fit under load, look at the areas of the socket supporting the axial load and also areas for transmission of the force couples in the socket design. We do not want isolated skin discoloration/contact on bony ends. Constantly check the bony reference to position your socket in the correct place for each load test.
|
Direction of movement |
Aims |
|
With elbow at 90 degrees of flexion, Extend the socket on patient while patient resists the extension force. You are pushing down on the socket. You should see, increased pressure just proximal to the distal end in broad areas on anterior (radial) surface and posterior proximal (ulnar) surface of the residual limb.
|
|
|
Flex the socket on patient while patient resists with elbow at 90 degrees of flexion. You will see, increased pressure proximal to the distal end in broad areas on posterior (ulnar) surface and anterior proximal surface (the anterior trimline) of the residual limb. |
|
|
Pronate the socket on patient while patient resists. Patient is trying to supinate. You may see increased pressure at the distal ends (dorsal radius and palmar ulnar surfaces) and the proximal trimline.
|
|
|
Supinate the socket on patient while patient resists. You may see increased pressure at the distal ends (dorsal ulna and palmar radial surfaces) and the proximal trimline.
|
|
|
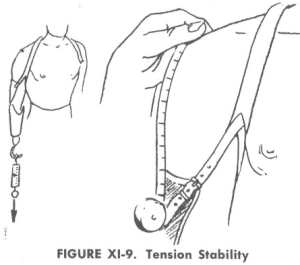
Standard for rotation: minimal, if any, rotation of the socket with 3 lbs. force. |
|
|
Compressive loading: Press socket up onto the pts limb. Look for relief at the distal end of the limb and look at the pts facial expression. Ask what they feel. |
|
| Axial loading
Standard: the prosthesis should not slip more than 1 inch and harness should not tear with 50lbs (or 1/3 body wt.) for axial load. |
|
Socket Fit
- Identify areas of high pressure and modify the trimlines to balance ROM and load needed to stabilize the socket.
- Administer the socket comfort scale.
5) Joint axis location
Joint Axis Location for Rigid Hinges for joint spacer installation
Standard: Joint center located at axis of anatomical center
Standard: Distance from humeral cuff to olecranon is 25mm
6) Length of the prosthesis
Standard: TD tip matches thumb tip of contralateral side
There are three approaches to determine the appropriate length:
- Match the contralateral length.
- lateral epicondyle or olecranon to distal thumb in a relaxed position = lateral epicondyle or olecranon (or elbow joint center) to distal end of TD
- Functional length:
- The length that most easily allows the person to reach their mouth with the prosthesis or do the things they want to do. This may be shorter than the patient’s contralateral limb or shorter than the result from the Carlyle index.
- Use the Carlyle index (ratio of the limb length to height) to determine the length.
- This works for both women and men.
Humeral length (AC to lateral epicondyle) = 0.19 times body height
Forearm length (lateral epicondyle to thump tip) = 0.21 times body height
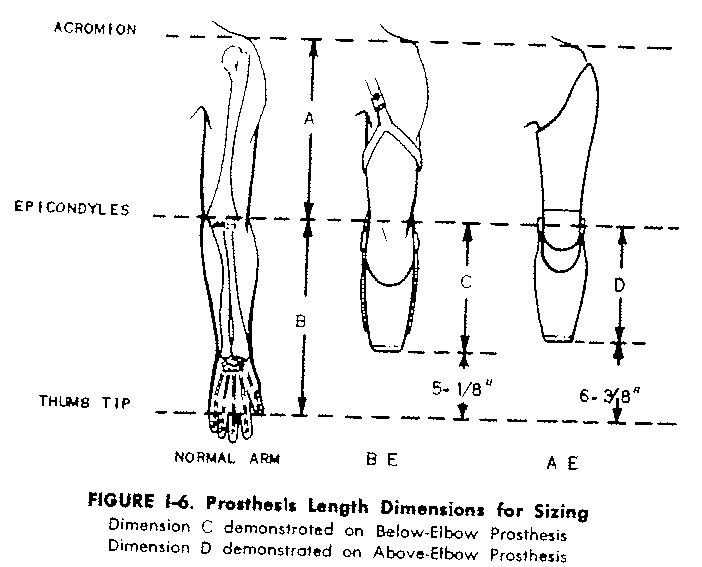
Mark length references on the test socket over the lateral epicondyle so the correct forearm extension can be fabricated.
Flexible hinges: put a reference mark for the lateral epicondyle (unless you took an olecranon to thumb tip measurement, then reference the olecranon)
Rigid hinges: you may use the lateral epicondyle for a reference.
7) Alignment of the forearm component
Alignment of the forearm component (variations)
- Long transradial alignment
- Align the PVC tube so that the axis of the tube is in line with the axis of the socket; and so the tube is at a right angle to the elbow axis.
- Pre-flexion angle refers to the flexed alignment of the forearm component relative to the socket.
- Short transradial alignment
- Align the tube so that the forearm is preflexed relative to the socket if the patient needs to reach their mouth. Or you may extend the forearm relative to the socket for a more natural appearance.
- Double check forearm length again
Alignment of the wrist unit (variations)
- Square off the wrist unit so that it is perpendicular to the form axis
- Cant the wrist 5 degrees anteromedially
8) Technical Operation of TD
- Check that full opening and closing can be obtained in these positions.
Standards:
- With elbow at 90 degrees 90% opening
- TD at waist 70% opening
- TD at mouth 70% opening
Box and blocks provides another method to assess the individual’s ability to operate the TD, specifically, the ability to grasp and release of small objects.
9) Harness critique
Don the prosthesis on the pt and check the harness fit
Standards:
- harness should lay flat on the patient’s body, no edges cutting in
- inverted Y splits within 2.5cm proximal to the pectoralis tendon to 2.5cm distal to clavicle
- anterior suspensor is positioned in the delto-pectoral groove
- crosspoint is inferior to C-7 and 2.5cm (1”) toward the contralateral side
- cable should either be completely off the back or fully in contact with it to prevent skin from being pulled into the housing when releasing pressure and closing the TD.
- This issue typically occurs at the posterior-lateral aspect of the back, where the cable travels around the curve and passes over areas with more soft tissue. If the cable and housing are positioned away from the back, this problem can be avoided.
- If positioning the cable completely off the back not possible, position the cable and housing along the flat part of the back to reduce the likelihood of this occurring. Additionally, we want to avoid skin breakdown due to the hanger/cable wrapping around the corner of the back without protection of the housing.
- flexible hinges secured 2.5cm proximal to wrist and fall through elbow joint center through ROM. Adjust crosshanger as necessary.
-
Double check
- suspension – the socket should be suspended through the anterior suspensor, inverted-y strap, and flexible hinges. It should not be suspended through the control strap
- pronation/supination ROM with attached harness
- ease of donning and doffing
10) Technical Quality of Fabrication
-
- Pads are glued securelyPlastic pulled with good suction
- Trimlines appropriateSmooth and even edges
- No defects in plasticStraps and materials are clean
- Rivets smooth with no sharp edges
11) Comprehension
Excellent comprehension includes the ability to (1) state the standards, (2) describe how the prosthesis varies from the standard, (3) identify all problem areas, (4) explain the reason for the problems, (5) explain possible solutions to resolve the problems and (6) address “what if” questions.
Do you understand if and why you obtained a “good fit”, do you understand why you did not obtain a “good fit”? Were you able to ask specific questions in a way that allowed you to obtain help? Were you afraid to ask for help? Do you know how to avoid making the same mistakes next time? Did you need a lot of help because you had a challenging patient and are just learning or because you were not prepared?
“What if” questions are asked to challenge your thinking about cases when the context is slightly different. Examples include: what might you do differently with the harness if the patient had bilateral limb loss? What is the main suspensor? OR What if the pt body type was different – how might you alter the harness design and cable setup?
12) Patient-centered context functional evaluation
This criterion is not part of the ‘Technical Evaluation’ of the prosthesis, but rather an evaluation of the contextual fit/match. In other words, how the prosthesis matches the activity and participation needs (ICF condition) for the specific patient (the specific context). The construct of interest is typically in the activity and participation domains of the ICF. It is ALWAYS something that is important to the patient and something that the prosthesis can affect.
- What is the goal, beyond a well-fitting prosthesis, of the prosthetic treatment?
Standard: a patient is expected to be able to lift 20-30lbs using a transradial prosthesis, unless the residual limb is extremely short of sensitive
|
Desired outcome |
Outcome Measurement Tool |
|
Aesthetic quality |
Amputee Body Image Scale (ABIS) |
|
Quality of life |
Trinity Amputation and Prosthetic Experience Scales (TAPES) |
|
Improve capability to perform specific activities |
Patient Specific Functional Scale (PSFS) |
|
Evaluate Upper Limb Function |
Disability of the Shoulder Arm and Hand (DASH) |
|
Evaluate Upper Limb Function |
Southampton Hand Assessment Procedure (SHAP) |
- Images from the UCLA manual, Prosthetic Checkout Chapter 11, William R. Santschi, Lester Carlyle and Norman Berger ↵
