4 Spectrum of Immune-Mediated Rheumatologic Diseases
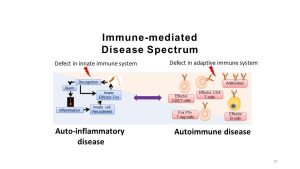
As we noted in the introduction, most of the diseases treated by Rheumatologists involve dysregulation of the immune system. In the past, people referred to these diseases as ‘autoimmune‘ in nature. With increased understanding of the different aspects of the immune system, we are discovering that some diseases involve defects in different portions of the immune response. The term immune-mediated is a broader term that encompasses both traditional autoimmune diseases characterized by loss of tolerance and generation of autoantibodies to self antigens as well as other diseases where defects in the innate system do not generate identifiable autoantibodies but show signs of excessive inflammation. This second category of diseases are increasingly being referred to as ‘autoinflammatory‘. As you recall, given the complex interplay between the innate and adaptive systems, most diseases fall somewhere on a spectrum between purely autoimmune and purely autoinflammatory.
But how does one diagnose an ‘immune-mediated’ disease? One of the key takeaway principles from this portion of the course is that in order to implicate something as primarily immune-mediated, there needs to first be a thorough investigation to make sure that the immune response is not being generated in response to an infection or malignancy. As you recall, the immune system has 3 key functions: Defense (protection against microbes), Surveillance (identification and elimination of cells showing signs of malignancy) and Tolerance (identifying and minimizing response to self). A common theme we will revisit this week is the interconnections between these three functions of the immune system. Practically speaking, this means that Immune-mediated diseases are all by definition diagnoses of exclusion. Though the array of different clinical criteria for diagnosis of rheumatologic disease may seem overwhelming, a key takeaway is that the same general approach is often utilized when ascertaining a diagnosis. The history, exam and labs are used to demonstrate:
- Evidence of tissue destruction:
- can be clinical: objective arthritis, rashes
- often supported by radiologic imaging or tissue biopsy
- Evidence of loss of tolerance:
- identification of autoantibodies
- identification of cell mediated response
- abnormalities in innate responses/hyperinflammation
- Exclusion of alternative causes:
- evaluation for infection
- evaluation for malignancy
As you can see, portions of this week will give us a chance to revisit some key concepts from your I&I course and is a good opportunity to refresh and synthesize your understanding of immunology. You do not need to remember everything from I&I but recalling some key facts will help you navigate the week. Remember you can always go back to the I&I Canvas site and use the ‘Search’ function if you need to find specific information.
Remembering the timing of the two systems – innate or rapid, stereotyped first line defense often the first hours to days of a response and the adaptive response, a slower, more nuanced evolving system that generates memory and takes 7-10 days to reach full effect on first exposure. Recalling the timing of action of these two systems can be very helpful in thinking through presenting signs and symptoms in patients to help you try to identify which aspects of immunity might be involved in causing dysfunction.
Key Innate Concepts to Remember:
- Key Tissue resident Cells:
- Mast cells
- Dendritic Cells
- Macrophages
- Key Circulating Cells:
- Neutrophils
- Eosinophils
- Monocytes (really innate and adaptive)
- Key Circulating Molecules:
- Complement system
- Key Cytokines
- TNF-alpha
- IL-1
- IL-6
Key Adaptive Concepts to Remember:
- Key Cells
- B-cells (CD20 positive)
- antibody isotypes: IgM, IgG, IgA, IgE
- T-cells (CD3 positive)
- CD8+ cytotoxic cells
- CD4+ helper cells
- CD4 subsets
- Th1
- Th2
- Th17
- CD4 subsets
- CD4+ (Fox P3+) regulatory cells
- B-cells (CD20 positive)
- Hypersensitivity Mechanisms (ways to explain the mechanism of tissue destruction by the adaptive immune system)
- Type 1 – Immediate, IgE-mediated (allergy, asthma, eczema)
- Type 2 – IgG or IgM antibodies against membrane bound antigens
- Type 3 – ‘Immune-Complex’ (antibodies to soluble antigens) deposit in small blood vessels causing inflammation
- Type 4 – Delayed type hypersensitivity – T-cell mediated tissue damage
