13 Skeletal Tissues
Introduction
The tissues of the skeletal system, bone and cartilage, are specialized types of connective tissue. Unlike epithelia, connective tissue consists of scattered cells and an abundance of extracellular material.
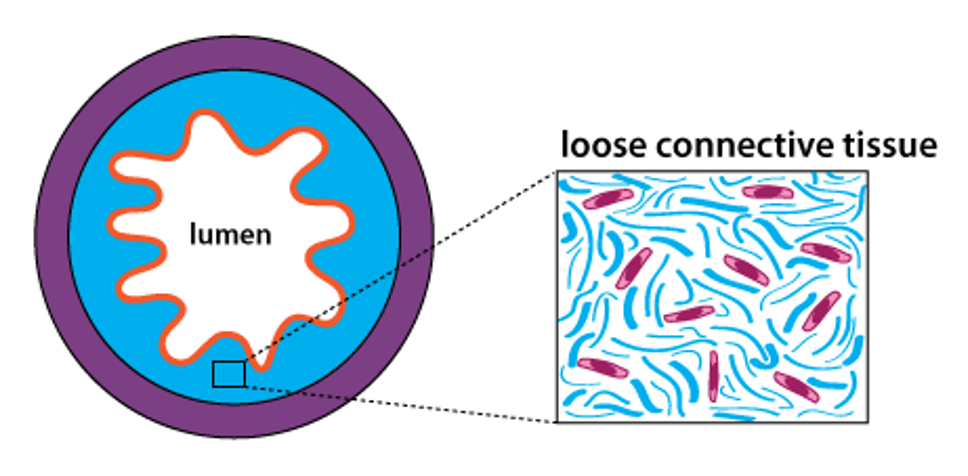
Connective tissue cells (pink in the figure above) synthesize and secrete proteins such as collagen that assemble into large fibers (cyan in the figure above) to give structure to the tissue. Bone tissue is rigid and strong because mineral salts of calcium are deposited within the framework of collagen fibers. Cartilage is solid and flexible because it contains a large amount of proteoglycans (sugar-linked proteins) among the collagen fibers of the extracellular matrix. The proteoglycans contribute to the physical properties of cartilage that allow it to resist compression.
Bone
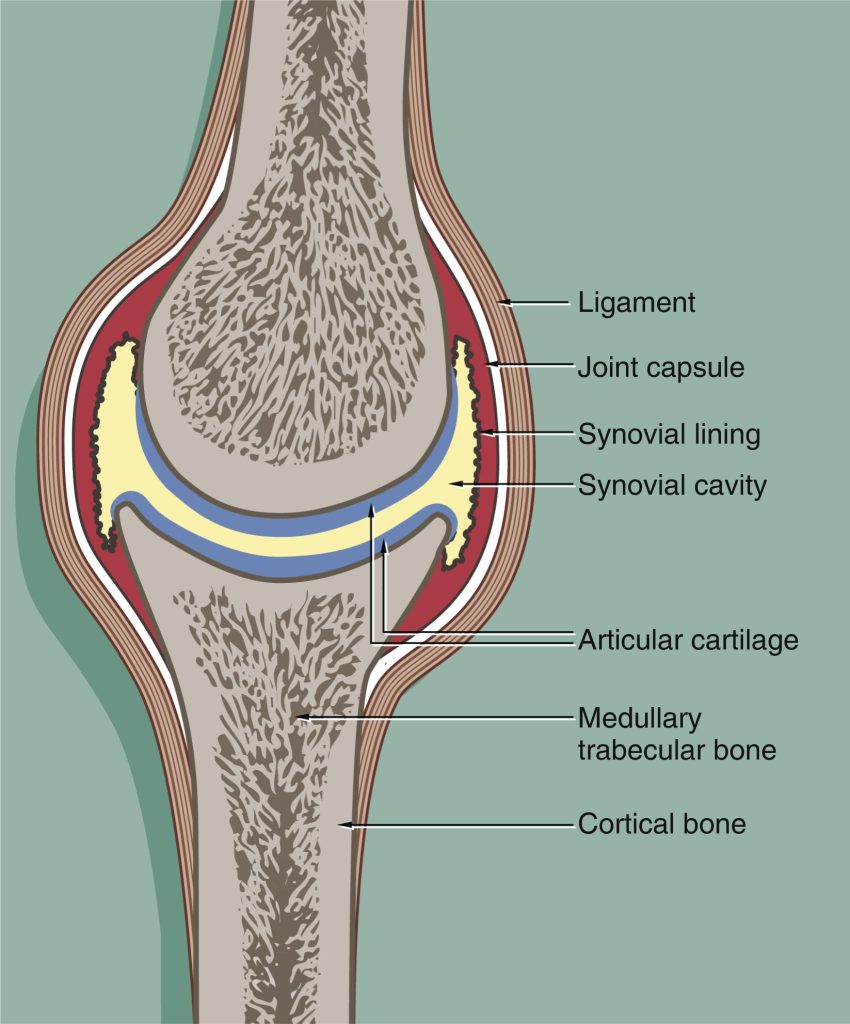
At the gross level, it is possible to distinguish two basic types of bone tissue: compact bone and trabecular bone (trabecular bone is also called spongy bone or cancellous bone). Compact bone is dense and solid, while trabecular bone consists of a fine network of interlocking struts. Compact bone forms the outer layer of long bones, while trabecular bone is found in the central cavity, and also at the ends of bones.
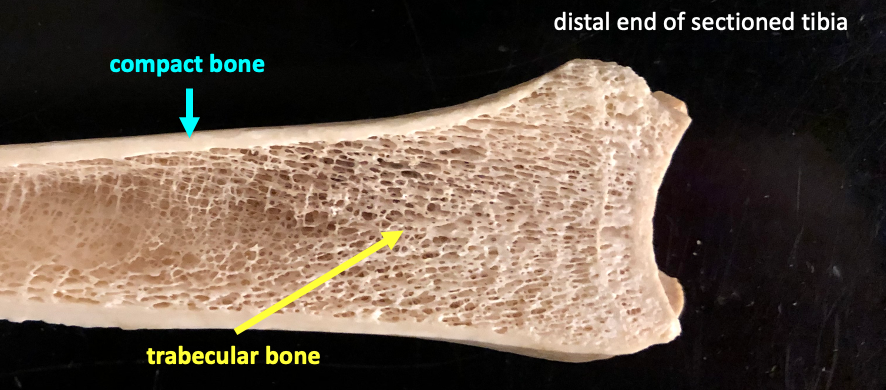
The figure above shows a tibia that has been sectioned longitudinally, so that you can compare compact bone to trabecular bone.
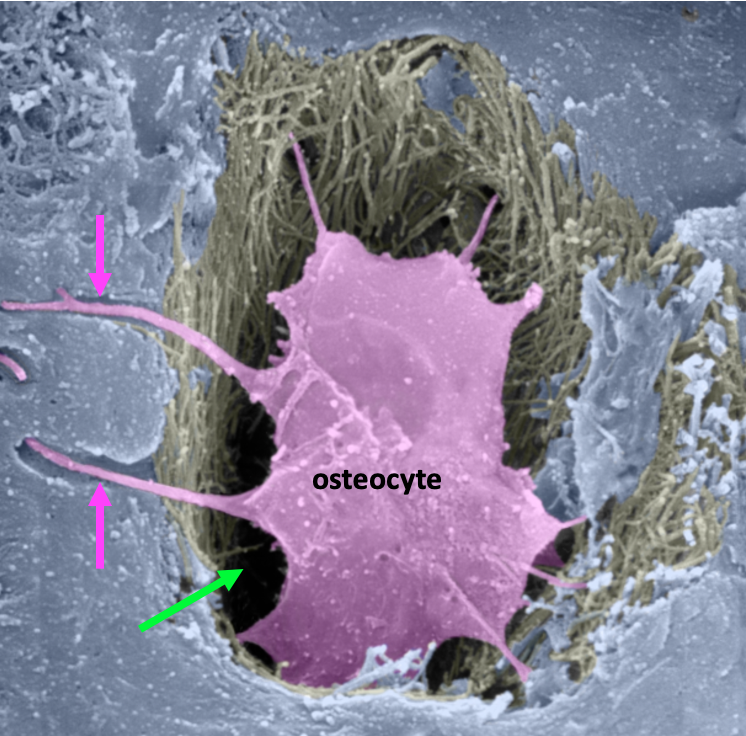
Bone cells are called osteocytes. They develop from precursor cells called osteoblasts that are important in the process of bone remodeling. Osteocytes are encased in bone matrix and have many fine processes that extend away from the cell in tiny channels called canaliculi (singular: canaliculus). The figure below is a scanning electron micrograph showing an osteocyte.
Below is a schematic diagram illustrating the structure of bone tissue.
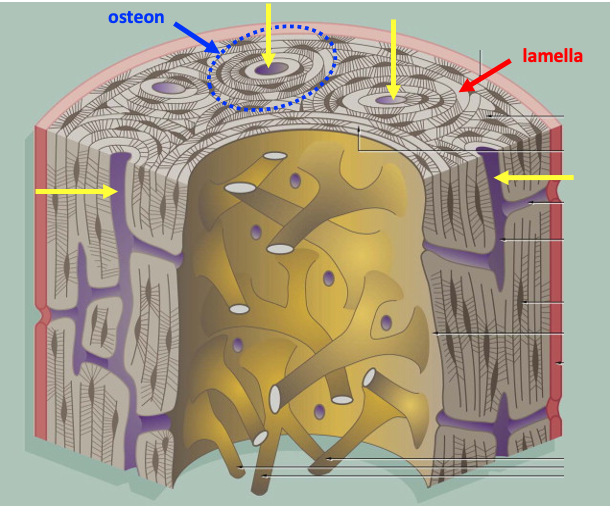
Compact bone consists of many parallel units called osteons that are tightly packed together to form the strong outer layer of bone. The osteon consists of concentric layers of bone matrix; a layer of bone matrix is called a lamella. The concentric lamellae surround a central Haversian canal. In the living tissue, the Haversian canals are occupied by blood vessels and nerves. Osteocytes are located in spaces between the lamellae.
The slides below are of thin ground sections of dried compact bone, and so the living cells are not visible. However, this type of preparation is good for revealing the spaces and fine channels that are occupied by osteocytes in the living bone.
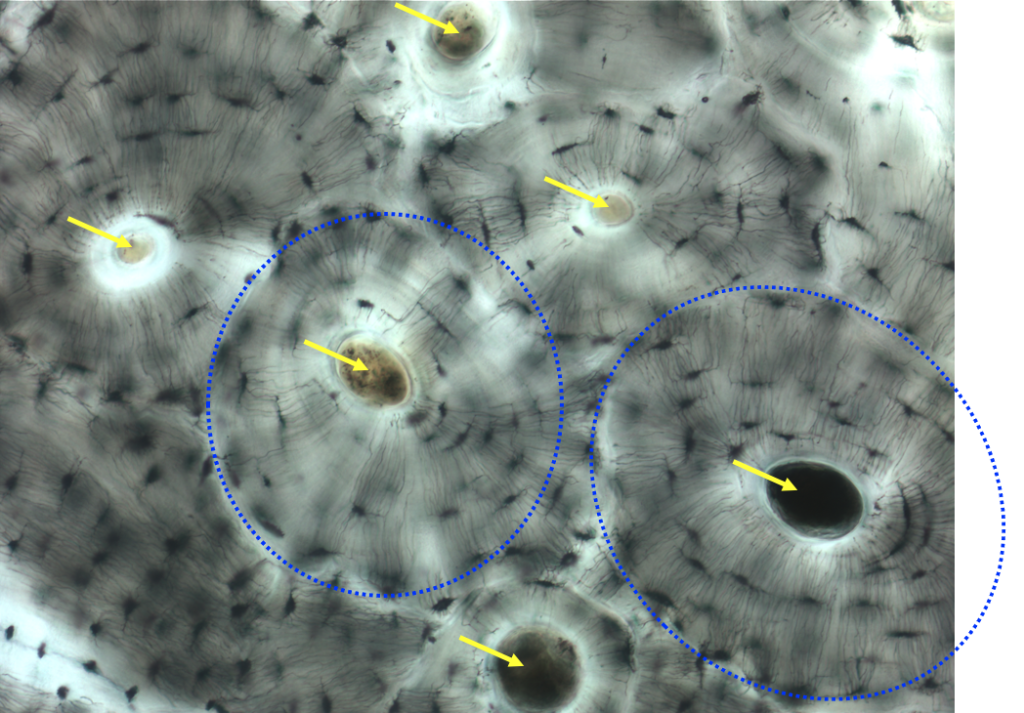
The picture above shows compact bone at low magnification. The large circles that you see at the centers of the osteons are the Haversian canals.
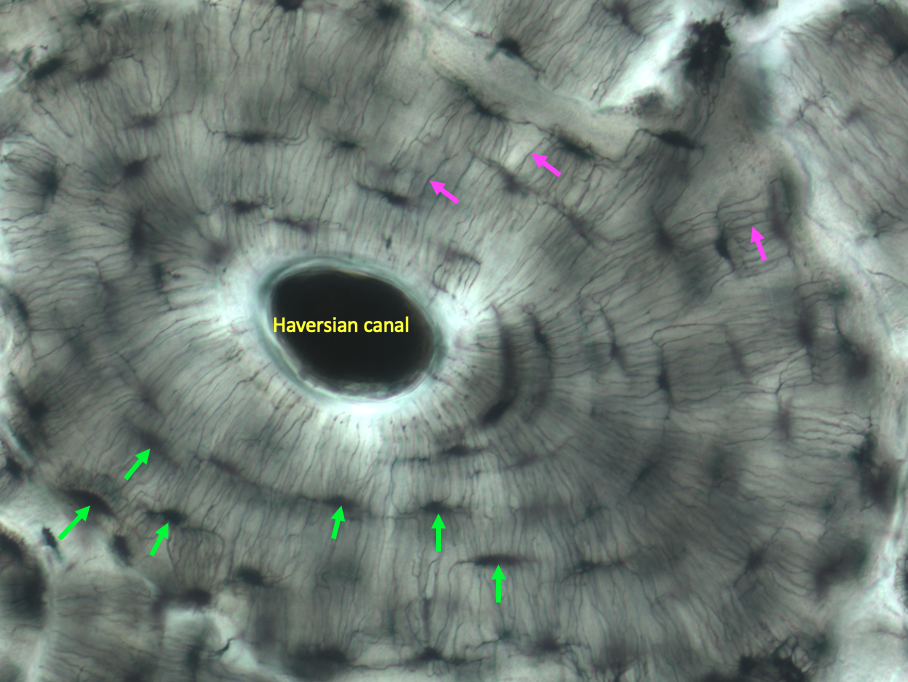
In the higher magnification view above, you can see that there are black spaces between the lamellae that are arrayed around the central Haversian canal. These spaces are called lacunae (singular: lacuna). In living bone, each lacuna contains an osteocyte. Because osteocytes are enclosed within layers of bone, they need to have a way to receive nutrients and communicate with other cells. So each osteocyte extends fine cellular processes through narrow channels called canaliculi (singular: canaliculus). In the image above, the canaliculi are the fine black lines extending perpendicularly from each lacuna.
Cartilage
The most common type of cartilage in the body is called hyaline cartilage. Hyaline means glassy. A layer of hyaline cartilage, the articular cartilage, is found at the ends of bones within synovial joints, providing a smooth articular surface.
Hyaline cartilage also forms structural rings and plates in the respiratory tract. The trachea is the large central airway that connects the upper respiratory tract (nasal passages, oral cavity, throat structures) to the airways that lead to the lungs.
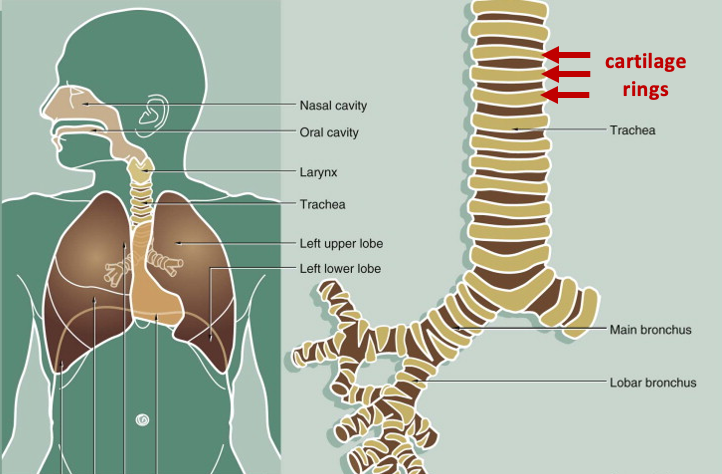
The trachea is held open by rings of cartilage. These rings do not form a complete circle; instead they have the shape of a C. The picture below shows the end of one of the C-shaped rings of cartilage extending off to the lower left.
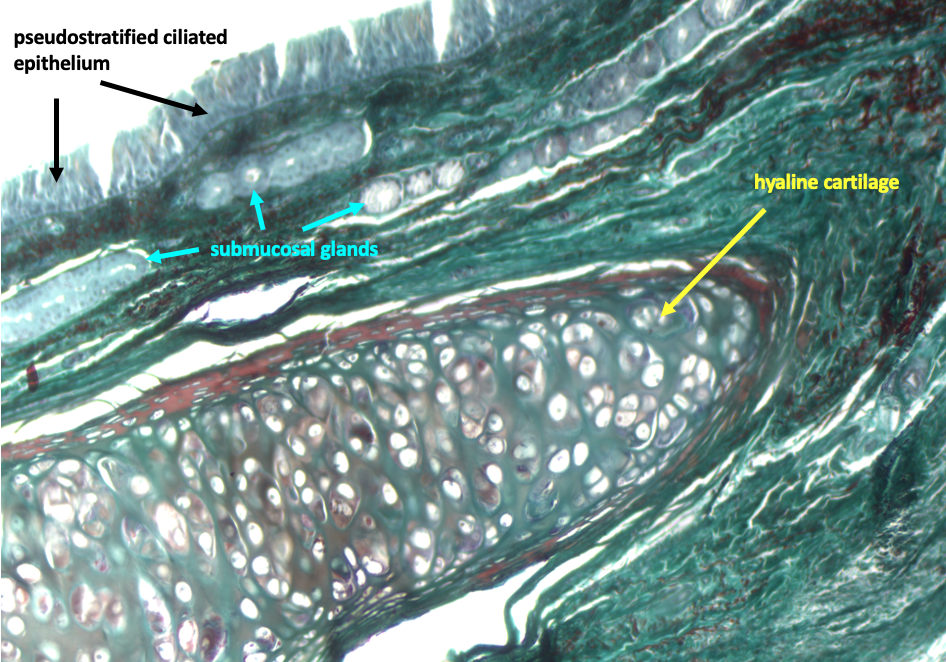
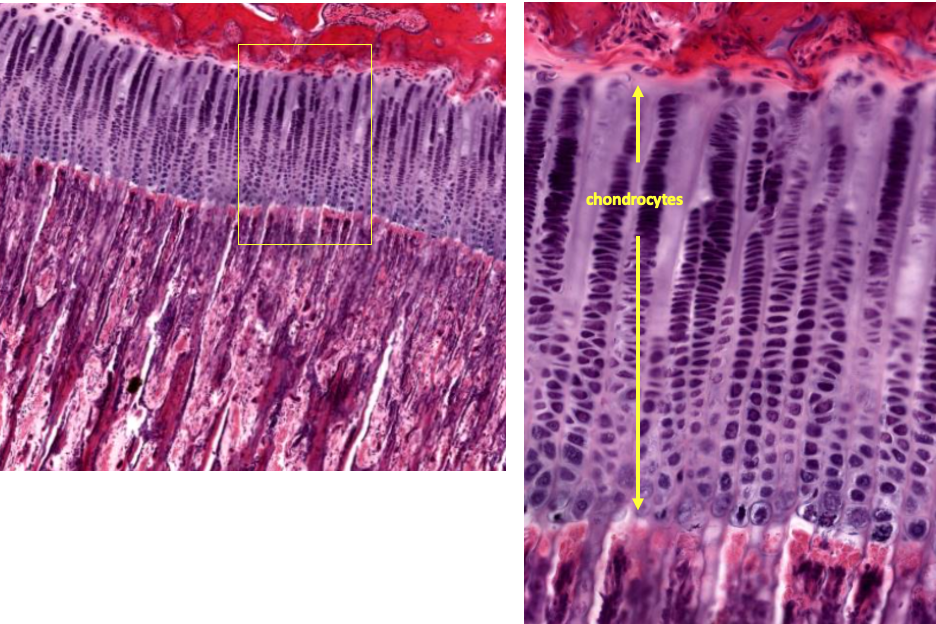
At the microscopic level at high magnification, cartilage has the appearance of Swiss cheese.
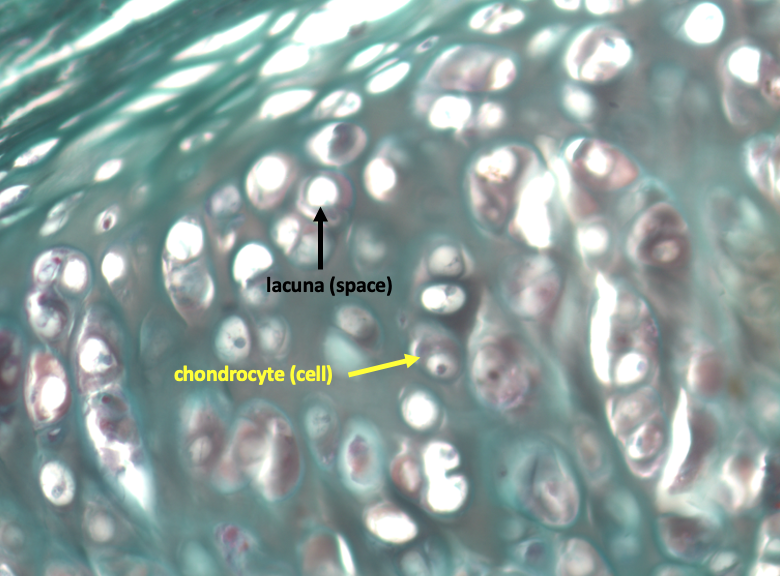
In the living tissue, each space that you see is occupied by a cartilage cell, called a chondrocyte. As in bone tissue, the spaces are called lacunae (singular: lacuna). Unlike bone, cartilage is not penetrated by blood vessels. This limits how thick cartilage can become since nutrients must diffuse through the tissue to reach cells. Cartilage also has much less capacity for repair. Damage to articular cartilage is what occurs in arthritis.
Epiphyseal Growth Plate
The long bones develop by a process known as endochondral ossification. “Endochondral ossification” means literally “bone formation (ossification) within cartilage (endochondral).” The figure below illustrates the steps involved in endochondral ossification.
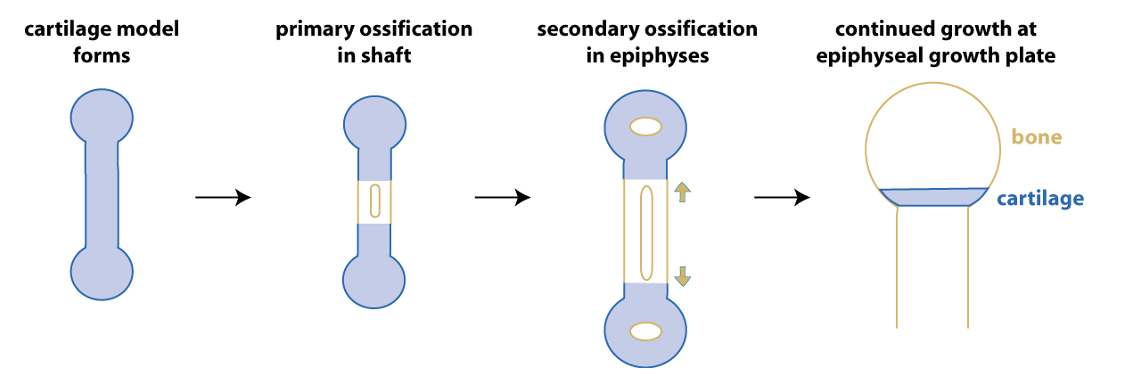
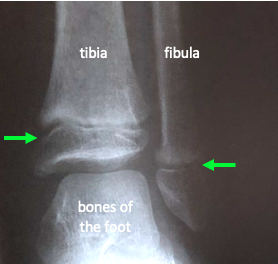
Initially, connective tissue cells condense in a spot, differentiate as chondrocytes, and form a cartilage model of the bone. The initial conversion to bone (primary ossification) occurs in the shaft of the bone. Ossification moves outward from the center of the shaft, while secondary ossification centers form at the epiphyses (the ends of the bone). Eventually there is a transverse plate of cartilage, the epiphyseal growth plate, left at each end of the bone. This is the site where bone continues to grow during childhood. The figure below shows an x-ray of the ankle region of a 6 year old child. The epiphyseal growth plates appear as dark lines on an x-ray because they are cartilage, and not bone.
The next figure shows a low magnification view of a section of growing bone. The bone tissue stains deep red, while the cartilage of the epiphyseal growth plate is purple.
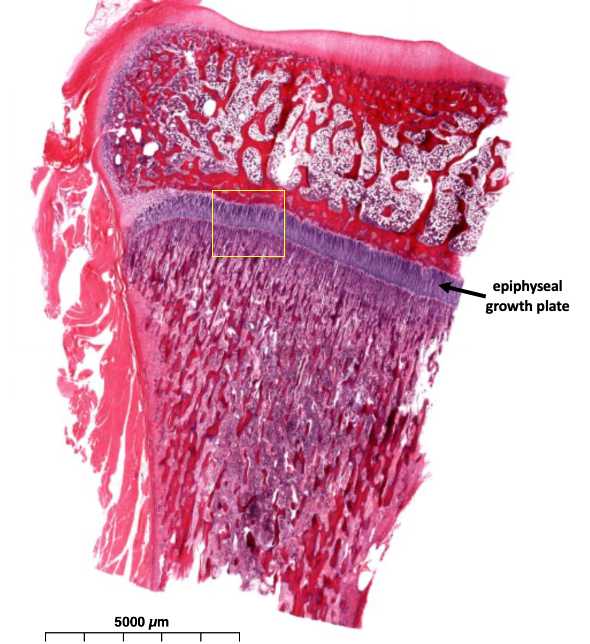
The figure below shows the epiphyseal growth plate at high magnification. The dividing cells in the growth plate are chondrocytes.