24 Renal Clearance
In this chapter we will explore the concept of renal clearance through the evaluation of a patient with chronic kidney disease. Information about the patient is presented in blockquotes in blue boldface. Questions are presented periodically, which you should try to answer yourself before clicking to see the response. In a quiz section test, you will be expected to be able to answer these questions, as well as being able to identify terms in purple bold face. In class we will do the calculations that are presented here in the pink textboxes.
Patient D
A 54-year-old woman with an 11-year history of type 2 diabetes presented for care. Her blood pressure (BP) was 155/90 mm Hg, and the glycated hemoglobin level was 7.6 mg per deciliter. The medications she was taking include:
- metformin
- ACE inhibitor
- statin
- thiazide diuretic
Metformin is a drug that is used to control hyperglycemia in type 2 diabetics. Statin drugs inhibit a key enzyme in cholesterol synthesis causing a decrease in LDL cholesterol, which decreases the risk for cardiovascular disease. The ACE inhibitor and the thiazide diuretic are two drugs that treat high blood pressure.
She was first noted to have proteinuria 4 years earlier; her serum creatinine level then was 1.1 mg per deciliter. A 24-hour urine collection was performed and analyzed. Her urinary protein excretion was 2.8 g per 24 hours. At the time of presentation, her serum creatinine level was 2.1 mg per deciliter.
Proteinuria means protein in the urine. Normally, proteins are not filtered because they are too large to pass through the filtration membrane. Proteinuria is a sign of kidney disease. A sign is something that can be discovered or measured in an examination, as opposed to a symptom, which is a change that the patient experiences as a consequence of a disease.
The second factor that is being monitored in this patient is serum creatinine. This is a measure of the concentration of creatinine in the blood. Creatinine is a metabolic breakdown product of creatine, which is found in skeletal muscle.
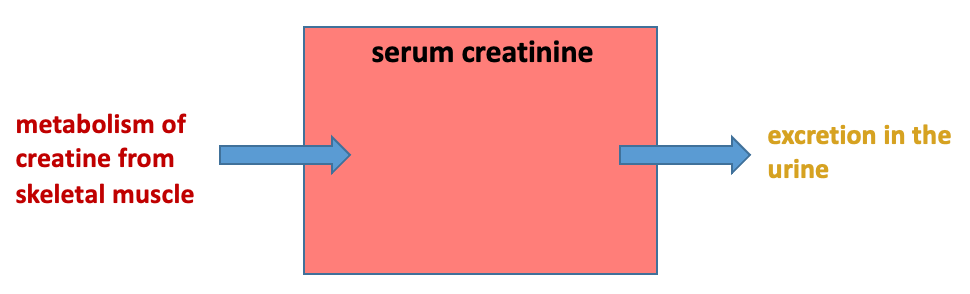
Normally, small amounts of creatine are converted to creatinine and slowly released to the blood. The concentration of creatinine in the blood depends upon how fast it is removed by the kidneys.
Glomerular Filtration Rate
The increasing proteinuria and serum creatinine measures indicate that this patient has kidney disease. An important measure of kidney function is the glomerular filtration rate (GFR). The GFR is the rate at which fluid leaves the glomerular capillaries and enters Bowman’s space. The measured GFR is the sum of the single nephron glomerular filtration rate for all the functioning nephrons in both kidneys. If a disease process is causing damage and loss of nephrons, this will cause a decline in the GFR.
The average GFR in a healthy young adult is about 115 ml/min, although GFR varies according to sex and also is usually normalized to body surface area to account for individuals of different sizes. This patient who has diabetes and proteinuria has diabetic nephropathy, the most common form of chronic kidney disease. Chronic kidney disease occurs when some process causes steady damage to the kidney over the course of years. Chronic kidney disease is diagnosed when GFR falls below 60 ml/min.
Renal Clearance
There are different techniques for determining GFR, but we want to focus on the method that makes use of the concept of renal clearance. Renal clearance is the rate at which a substance is removed from the blood plasma by the kidneys. Renal clearance is defined as the volume of plasma that is cleared of a substance by the kidneys per unit time. The formula for clearance is:
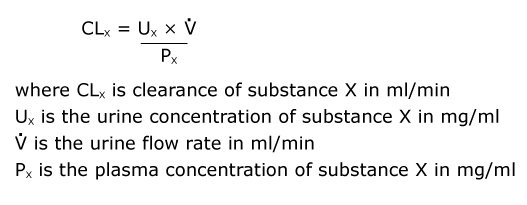
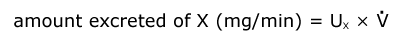
Note that the numerator of the clearance formula, urine concentration (mg/ml) times urine flow (volume in ml/min) yields the amount excreted (technically rate of excretion in mg/min).
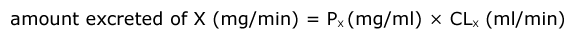
To determine the volume of plasma “cleared” per unit time, we divide this number by the plasma concentration. Another way of thinking about clearance is to recognize that the amount excreted is equal to the plasma concentration times the volume of plasma cleared.
Renal clearance treats the situation as though the kidneys are totally removing a substance from discrete volumes of plasma. That isn’t really the way the kidneys work; nevertheless, clearance is a useful concept.
Measurement of GFR
GFR can be directly measured by measuring the renal clearance of inulin. Inulin is a plant carbohydrate, and so it must be injected into the body. Inulin is used to measure clearance because of two key properties:
- inulin doesn’t bind to blood proteins, meaning it is freely filtered
- inulin is neither reabsorbed nor secreted
To understand why the clearance of inulin is equal to the glomerular filtration rate, we need to understand how substances get into the urine so that they are excreted. This requires a review of the processes that occur in the kidney, which are shown in the figure of a diagrammatic nephron below.
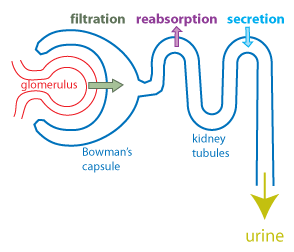
The first step in urine formation is filtration, in which about a fifth of the plasma that flows into the glomerular capillaries moves across the filtration membrane and into Bowman’s space. This filtrate then flows through the renal tubule where substances may be transferred from the forming urine back into the extracellular fluid (reabsorption) or substances may be transferred from the extracellular fluid into the forming urine (secretion). The amount of a substance that ends up in the urine is just the sum of these three processes: the amount filtered, plus any amount secreted, minus any amount reabsorbed.

In the case of inulin, there is no reabsorption and no secretion.
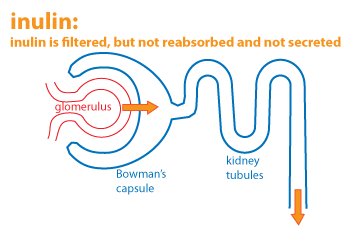
The only way that inulin gets into the urine is by filtration. Thus the volume of urine cleared of inulin is the same as the volume that was filtered. In other words, the clearance of inulin is the glomerular filtration rate (GFR).
The patient was enrolled in a clinical trial in which inulin clearance was determined. Inulin was injected and then the following measurements were made:
- urine flow rate: 1.2 ml/min
- urine concentration of inulin: 5.0 mg/ml
- plasma concentration of inulin: 0.25 mg/ml
What is the renal clearance of inulin?
What is the GFR?
Creatinine Clearance
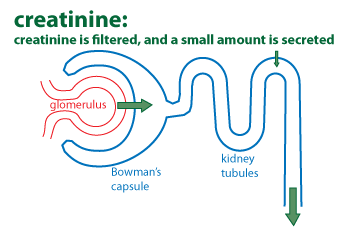
Because inulin needs to be injected, inulin clearance is not routinely measured. Instead, clinicians monitor creatinine and determine creatinine clearance.
The 24-hour urine collection that the patient had done was used to determine creatinine clearance. The following measurements were made:
- volume of urine: 1810 ml collected in 24 hours
- urine concentration of creatinine: 0.5 mg/ml
- plasma concentration of creatinine (given earlier): 2.1 mg/dL
What is the renal clearance of creatinine?
This calculation requires us to do some conversions. Note that the plasma creatinine concentration is given in mg/dL, which we need to convert to mg/ml. A deciliter (dL) is equal to 100ml. As well, the urine flow rate needs to be converted from ml/24hr to ml/min. Whenever you are doing calculations such as this, always be sure to follow the units. If you make the calculation correctly, the units should work out.
Next we will determine how much creatinine was secreted. Recall that the amount excreted (amount in the urine) will be the sum of the renal processes:

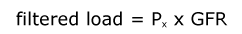
To determine the amount secreted, we must first determine the amount of creatinine filtered (the filtered load).The filtered load is equal to the rate at which fluid flows into Bowman’s space (the GFR), multiplied by the concentration of creatinine in Bowman’s space. Since filtration is just bulk flow of water and small molecules into Bowman’s space, then the concentration in Bowman’s space is the same as the plasma concentration. Thus, the equation for determining filtered load is:
The amount secreted will just be the difference between the filtered load and the amount excreted in the urine.
What is the filtered load?
How much creatinine is secreted?
Estimating GFR
Because only a small amount of creatinine is secreted, creatinine clearancecan be used as a rough estimate of GFR and a way to gauge kidney function.
In routine screening for kidney function, estimated GFR (eGFR) is calculated using a serum creatinine measurement plugged into various equations. These equations were developed from data in which both GFR and serum creatinine were measured in many patients and correlated mathematically, while adjusting for factors such as age, sex, and body weight of the patient.
Older eGFR formulas included an adjustment for Black race. The inclusion of race in eGFR formulas was problematic because race is not a biological determinant in the way that age and sex are. Furthermore there is a large variability in the degree of African ancestry among individuals identifying as Black. The National Kidney Foundation and the American Society for Nephrology have re-evaluated the use of race in these equations and issued a recommendation in September 2021 to use a race-free method for estimating GFR. Due to the efforts of a group of UW medical students, in June 2020, UW Medicine began using a formula for eGFR that is not adjusted by race. You can read more about that change in this article from the UW Daily.
In class, we will do the calculations for the questions posed in the pink boxes. On Quiz Section Test 5, there will be several calculation problems similar to the ones above. To prepare for this quiz section test, you should:
- Be able to convert units (i.e. mg/dL to mg/ml).
- Be able to calculate renal clearance from data provided.
- Know that the inulin clearance is equal to the GFR.
- Know how to calculate filtered load.
- Be able to determine the amount reabsorbed or secreted.
Additional practice problems and their solutions are available on the course Canvas page. Please note that although the practice problems may be multi-part questions, questions on the quiz section test will be limited to a single calculation.
