1 Epithelial Histology
What is an epithelium?
An epithelium is the type of tissue that covers surfaces, usually the linings of hollow organs in the body, or in the case of the skin, the outer surface of the body. The figure below shows a schematic of a simple epithelium, modeled after the epithelium lining the small intestine.
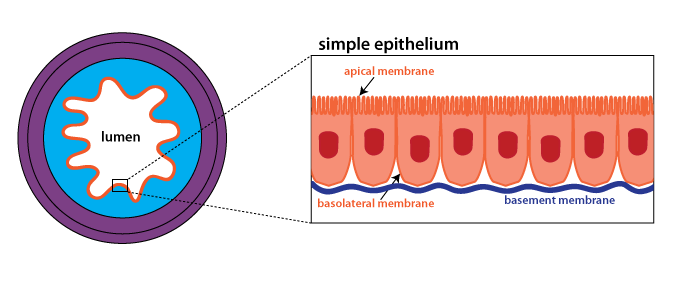
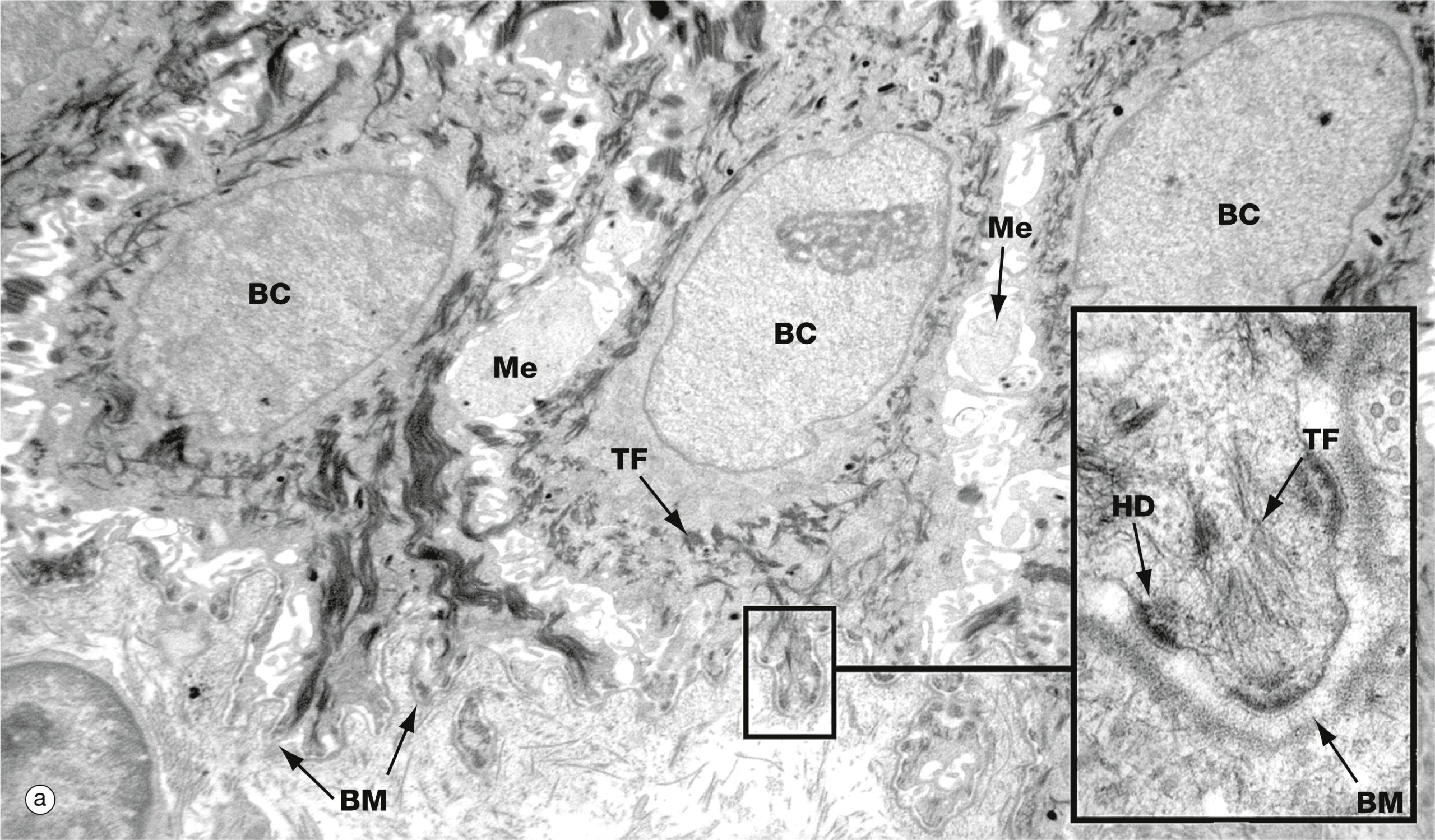
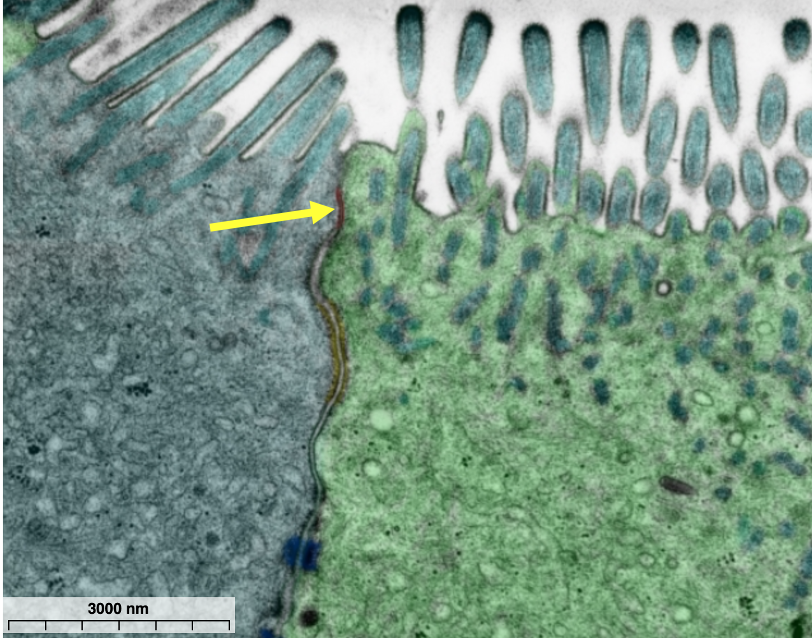
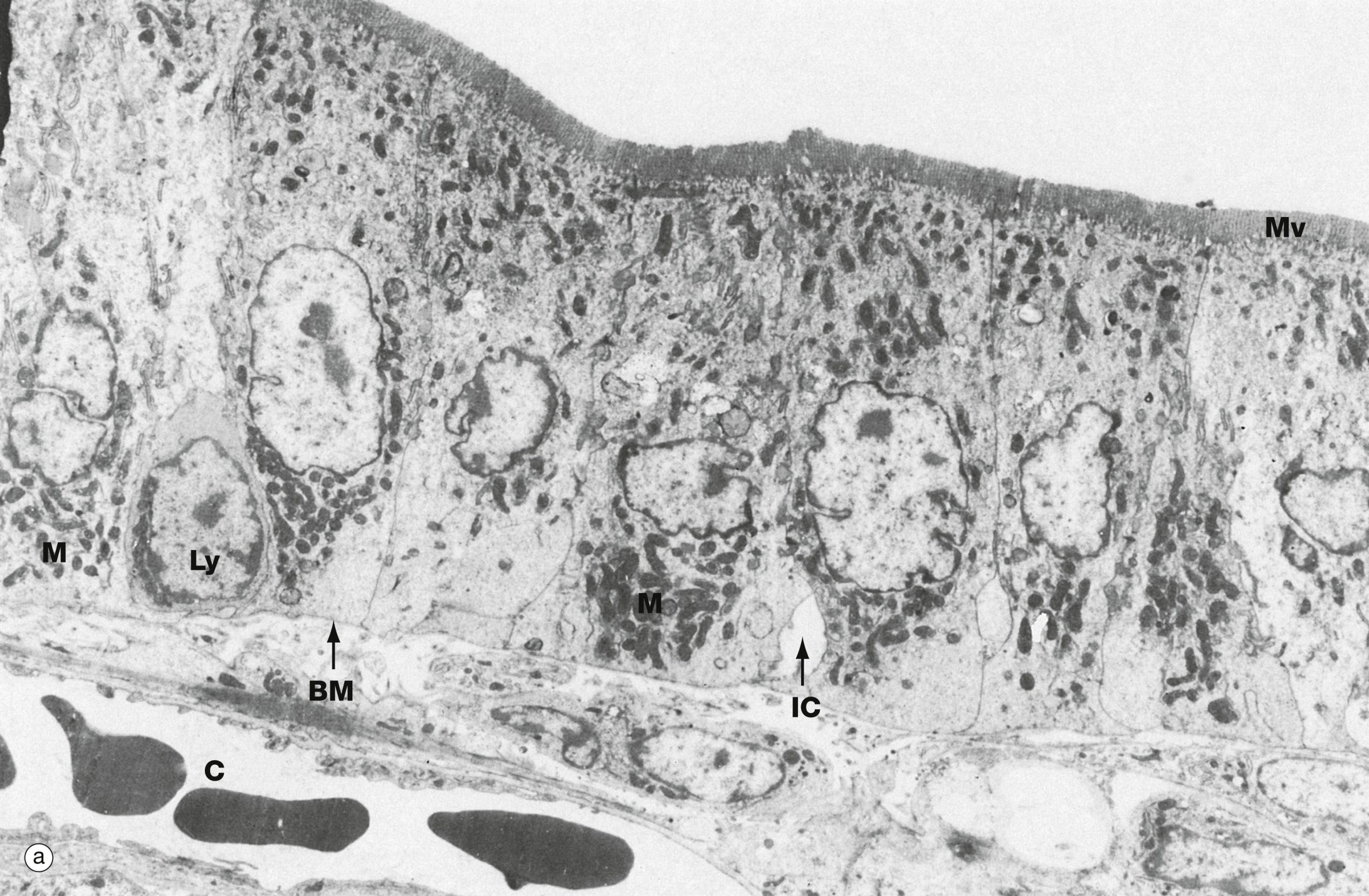
Epithelia are comprised almost entirely of cells. The apical surface faces the lumen (inside of a hollow organ) while the basal or basolateral surface is adjacent to the underlying tissue. In many epithelia, the apical surface is specialized. For instance, in the small intestine, the apical plasma membrane is folded into microvilli (see below) to increase the surface area for absorption of nutrients. Every epithelium has a basement membrane, that binds the epithelium to the underlying connective tissue. The basement membrane consists of a thin layer of extracellular proteins that is located next to the basolateral surface. Blood vessels do not penetrate through the basement membrane. In practice, the basement membrane is too small to be seen except on an electron micrograph (EM). The figure below is an EM of the basal surface of the epidermis in which the basement membrane can be seen.
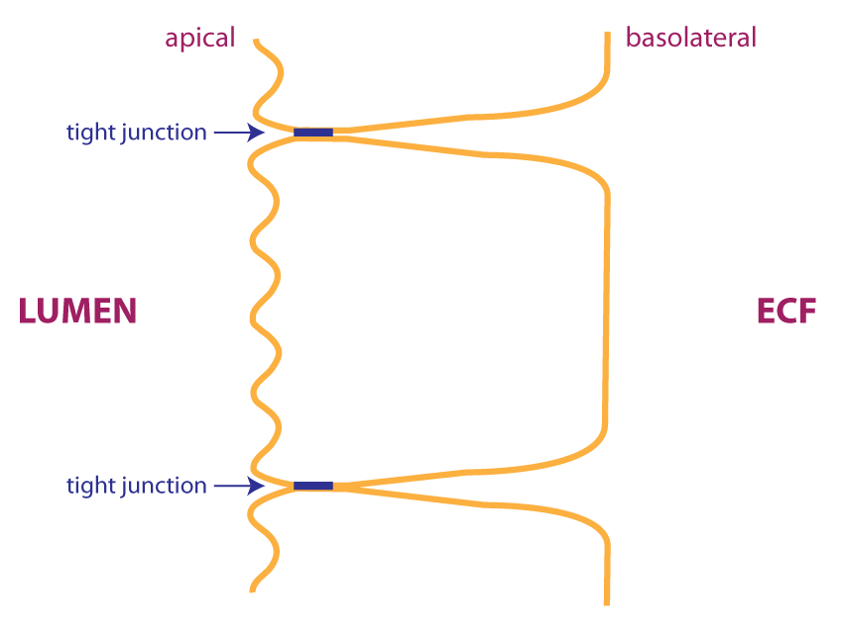
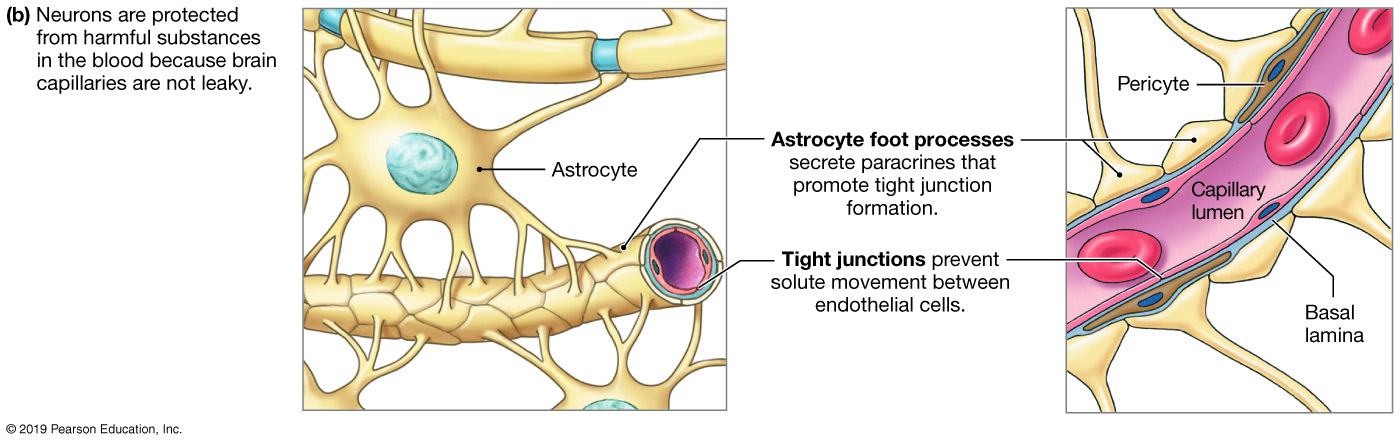
In many cases, adjacent epithelial cells are linked by tight junctions. Tight junctions consist of intercellular proteins that link adjacent cells to prevent the movement of substances between cells. Tight junctions are usually located near the apical surface of a simple epithelium as shown in the figures below.
https://histologyguide.com/EM-view/EM-298-intercellular-junctions/02-photo-1.html
Another effect of tight junctions is to divide the cell membrane into an apical and basolateral compartments. As we shall see, different proteins can be expressed in the apical and basolateral membranes to allow the directional movement of substances across the epithelium.
Epidermis of the skin
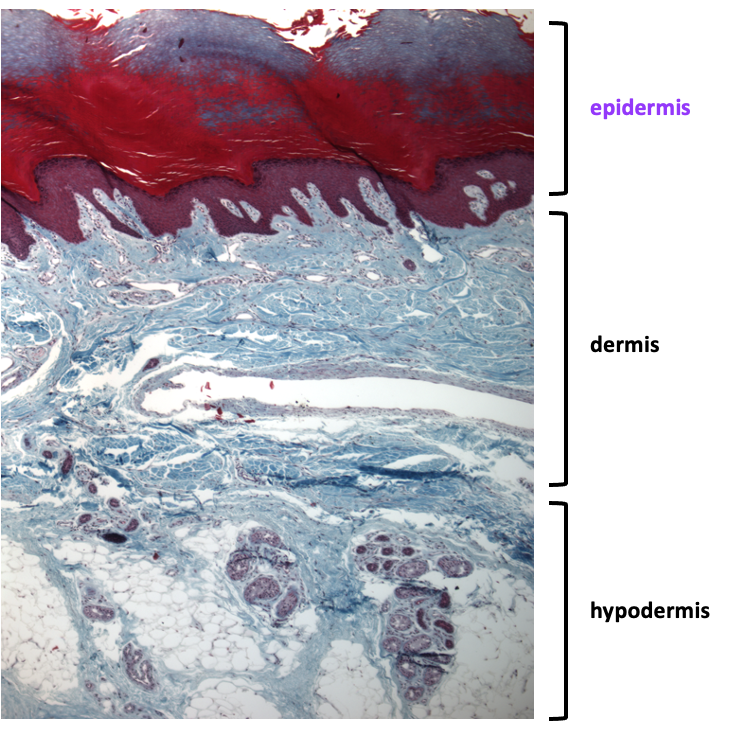
Skin has three layers: epidermis, dermis and hypodermis. The outer region is the epidermis, which is the epithelium that forms the surface of the skin. The middle region is the dermis, which contains dense connective tissue, blood vessels, and nerves. The innermost layer is the hypodermis, which contains loose connective tissue and adipose tissue, along with sweat glands, blood vessels, and nerves.
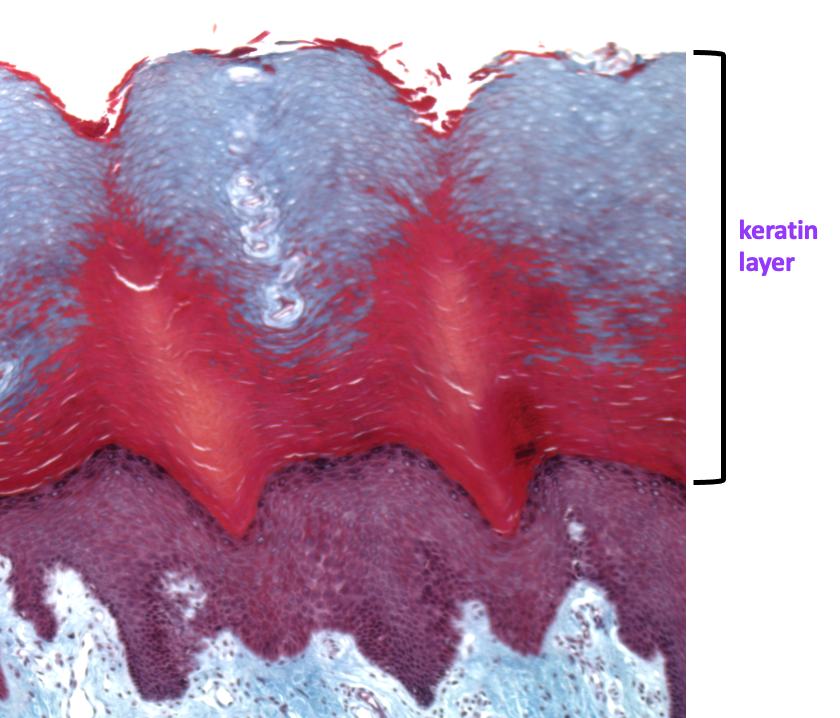
The next image is at higher magnifcation and focuses in on the epidermis. The epidermis is classified as a stratified squamous keratinized epithelium. Cells divide at the basal surface of the epithelium, and as new cells are generated, older cells are pushed towards the apical surface. As cells move apically, they become very flattened (squamous) and they fill up with an intracellular protein called keratin and die. For this reason, cells in the epidermis are referred to as keratinocytes. This type of epithelium is protective, with the keratin layer acting to protect the underlying tissue from abrasion and dehydration.
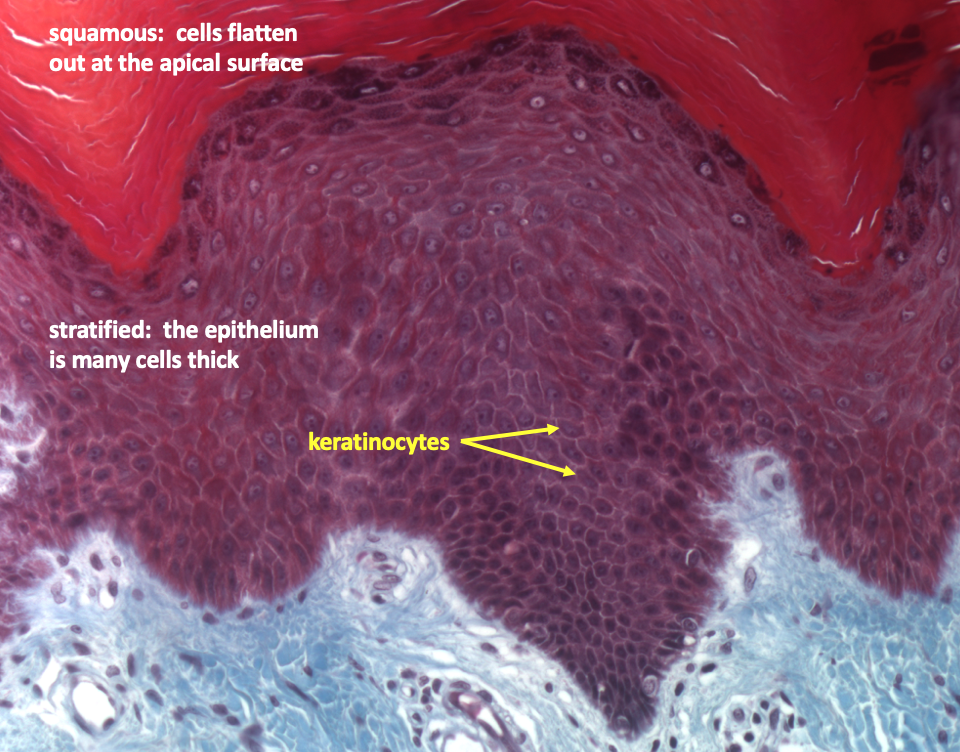
The image below focuses on the keratinocytes at high magnification. Note that cells appear dark at the apical surface, where they are filling up with keratin. The epithelium of the epidermis is stratified because it is many cell layers thick, and squamous because cells become flattened as they are pushed apically. Finally, it is considered keratinized due to the presence of keratin at the apical surface.
Endothelium of blood vessels
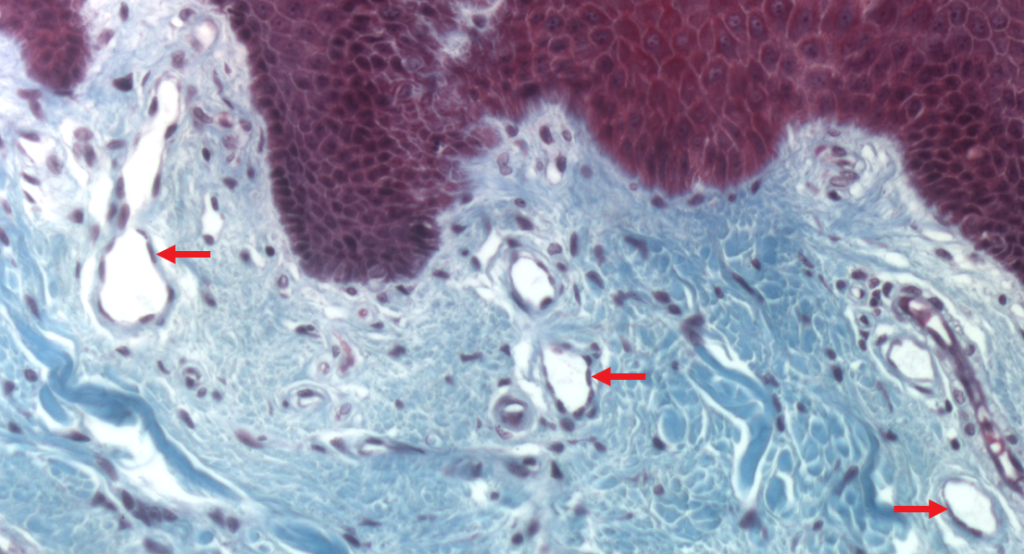
The endothelium is the simple squamous epithelium that lines all blood vessels. The very smallest vessels, capillaries, are made up of just endothelium. The image below shows capillaries in the upper part of the dermis. Note how each white space is outlined by a single layer of thin dark cells; this is the endothelium.
A healthy and intact endothelium acts as a barrier that isolates the blood from underlying tissue, preventing the formation of a blood clots. Endothelial cells also release important signaling molecules, affecting processes such as tissue growth and blood flow.
In the brain, the endothelium together with other cells surrounding the capillaries form a functional barrier known as the blood-brain barrier. Between endothelial cells there are tight junctions , limiting the permeability of the endothelium, and protecting neurons in the brain from toxins and other potentially neuroactive substances in the blood.
Columnar epithelium of the small intestine
The small intestine is a tube made up of smooth muscle, connective tissue and an innermost lining that contains the epithelium. In the digestive tract and other organs in which mucus is secreted on the surface of the epithelium, this lining layer is called a “mucous membrane” or mucosa. The figure below shows how the tissue layers of the small intestine are organized.
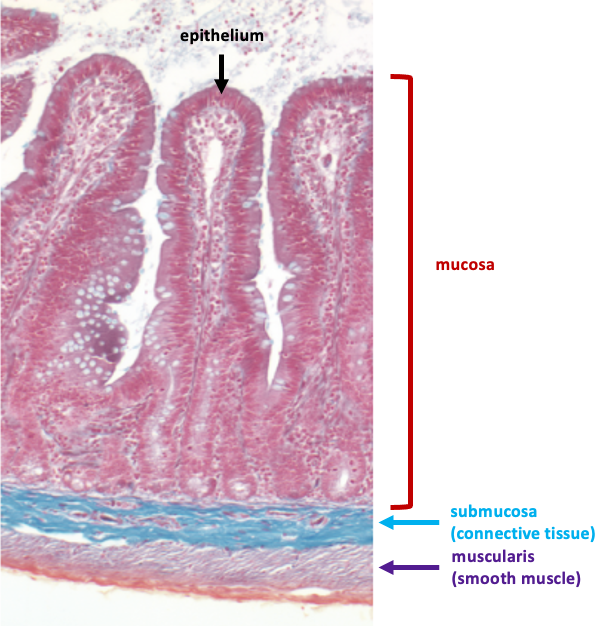
The epithelium of the mucosa in the small intestine folds up and down to form protrusions called villi (singular: villus). The folding of the epithelium increases the surface area available for absorption of nutrients. It is easiest to see the structure of the intestinal epithelium by focussing on the surface of a villus.
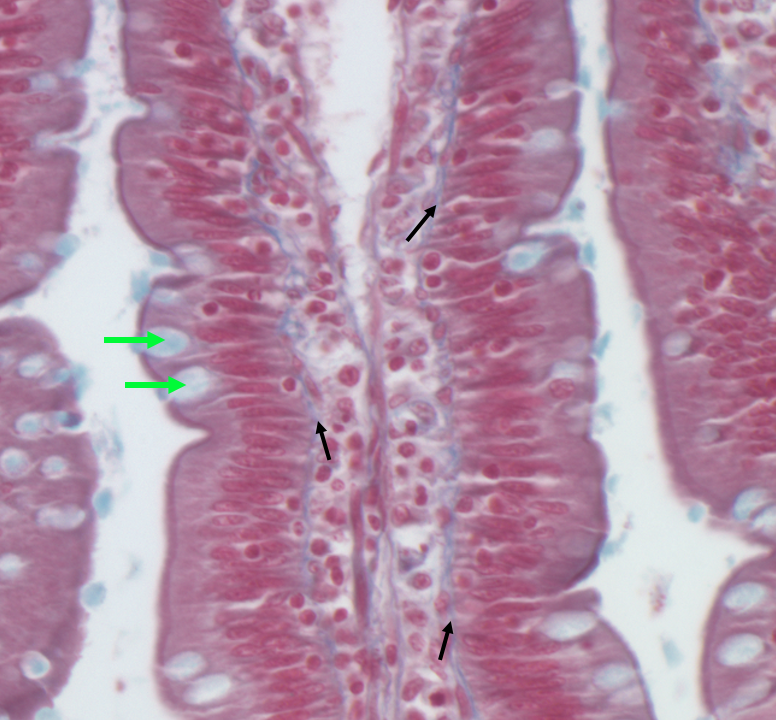
The image above shows part of a villus at high magnification. The intestinal epithelium is classified as a simple columnar epithelium because the epithelial cells, enterocytes, are tall and thin. Scattered among the enterocytes are mucus-secreting cells called goblet cells that stain pale blue. At the apical surface of the enterocytes, there is a dark line which occurs due to a web of proteins that anchor the microvilli, folds of the apical plasma membrane that further increase the surface area for absorption. Another term for the microvilli is “brush border”.
Below is an electron micrograph showing a row of enterocytes. The microvilli are visible as the dark layer at the top of the cells.
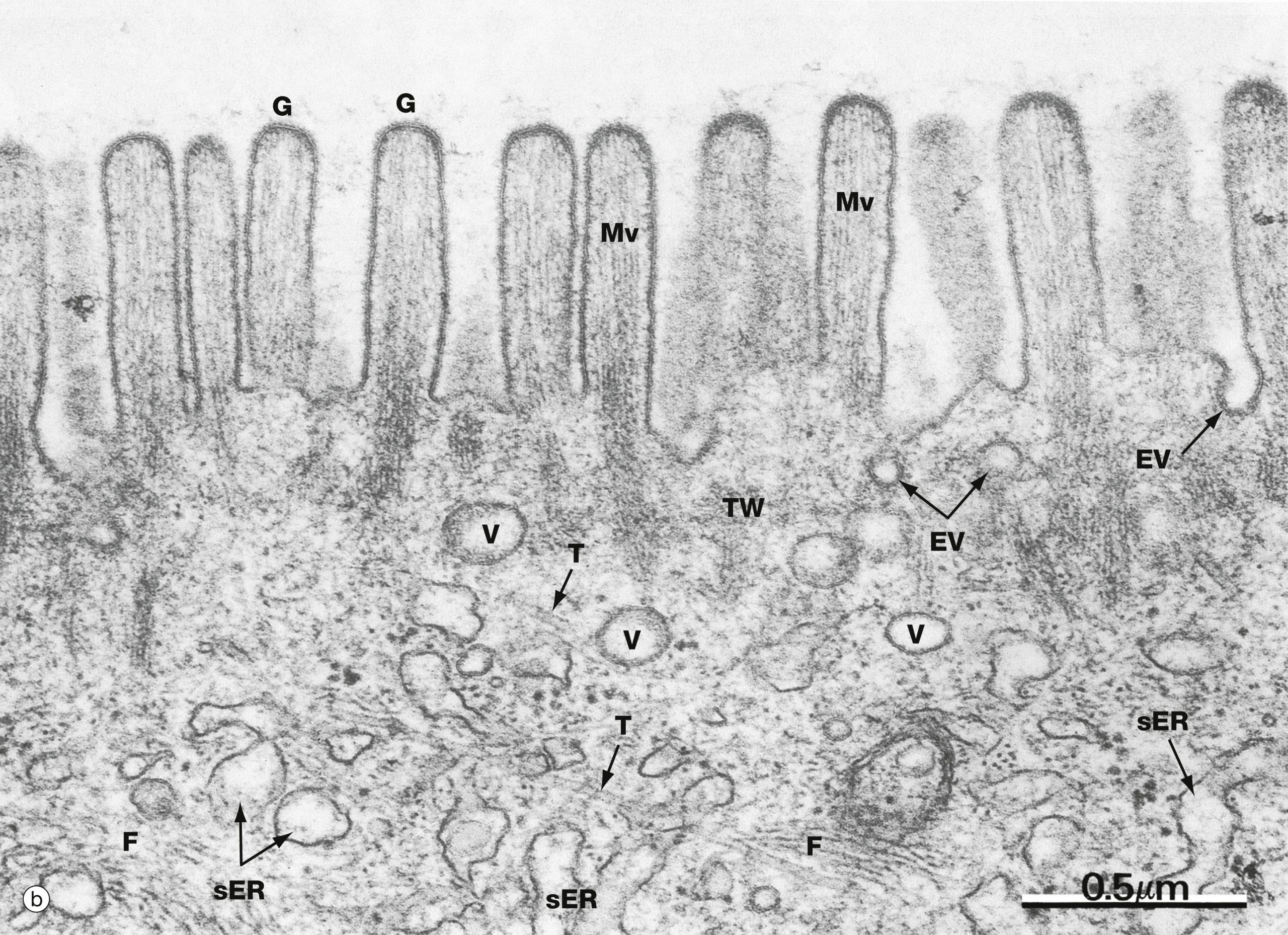
Microvilli are folds in the plasma membrane. This can be seen in a highly magnified electron micrograph focussing on the apical plasma membrane of an enterocyte.
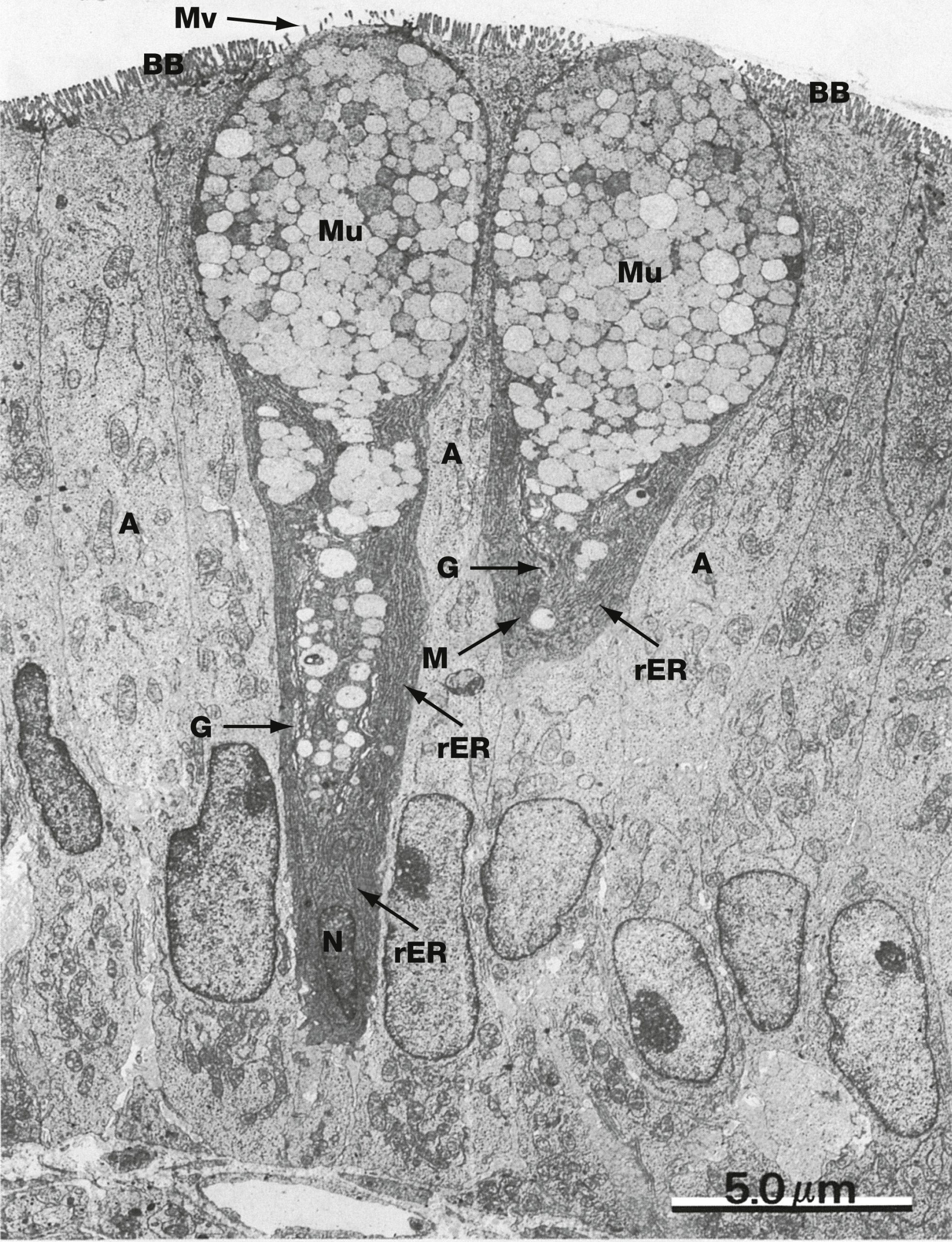
Goblet cells synthesize and secrete mucus. Mucus contains glycoproteins (mucins) that are synthesized in the rough endoplasmic reticulum. The micrograph below shows two goblet cells. The cytoplasm of the goblet cells appears darker due to the abundant rough endoplasmic reticulum. The apical part of each cell is filled with pale vesicles containing mucins.
Pseudostratified ciliated epithelium in the airways
The airway epithelium lines the passages that conduct air into the lungs. Airways conduct air into the lungs; by contrast, the tiny sacs called alveoli, which are found at the ends of the airways, are where gas exchange occurs.
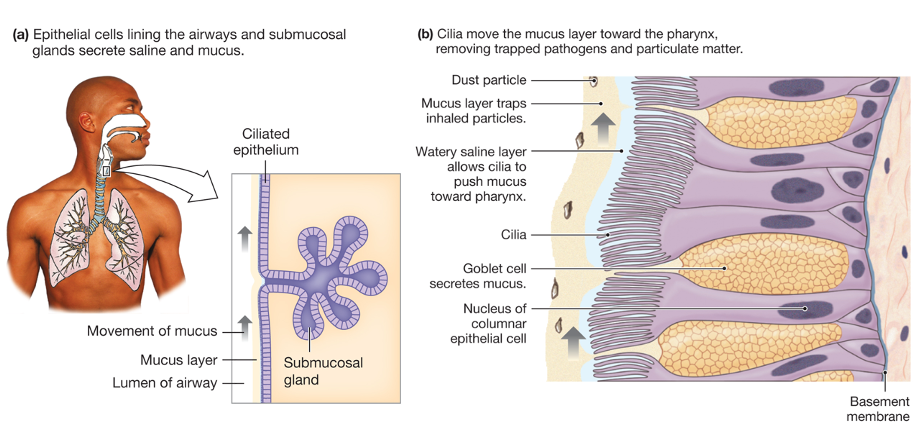
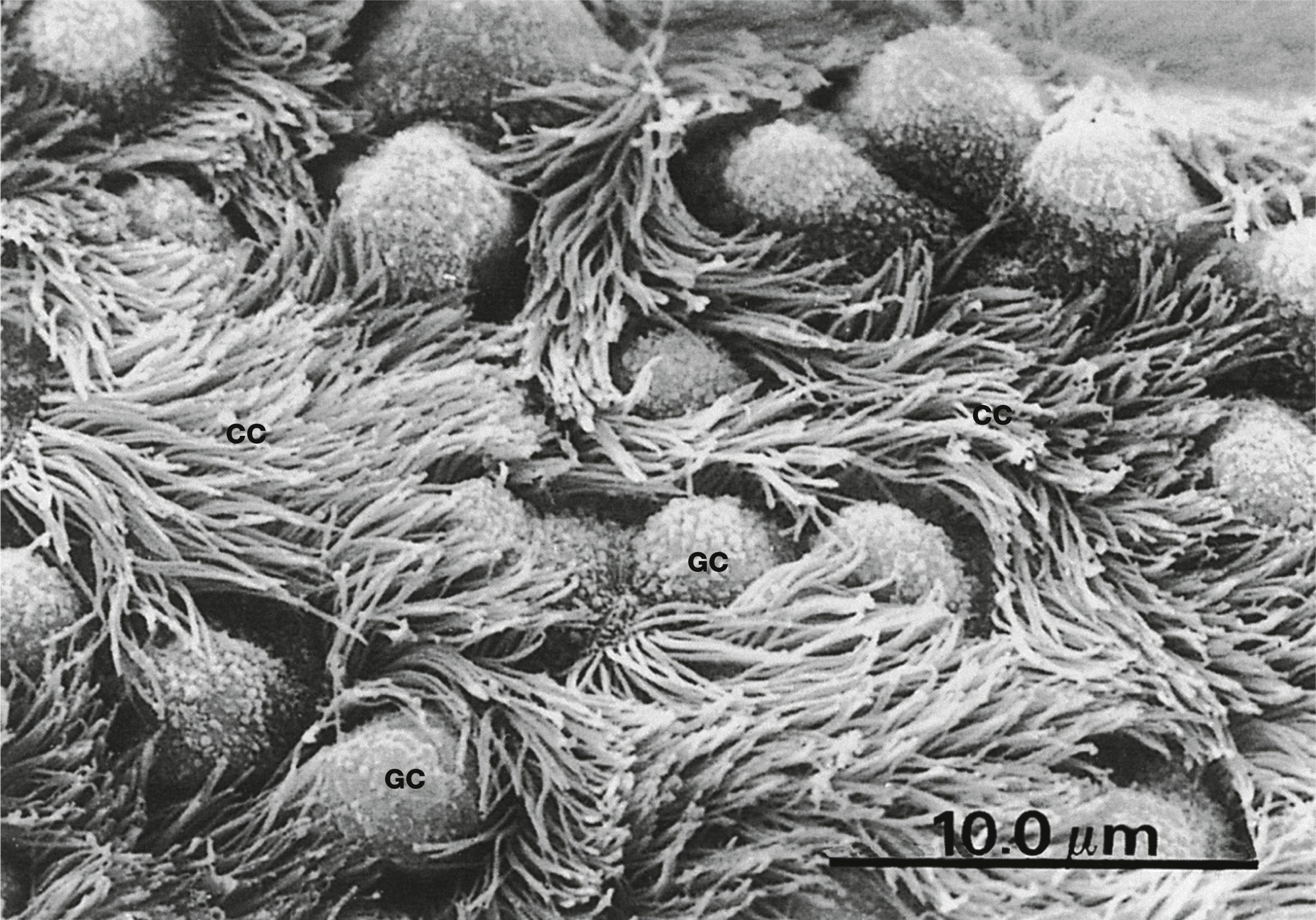
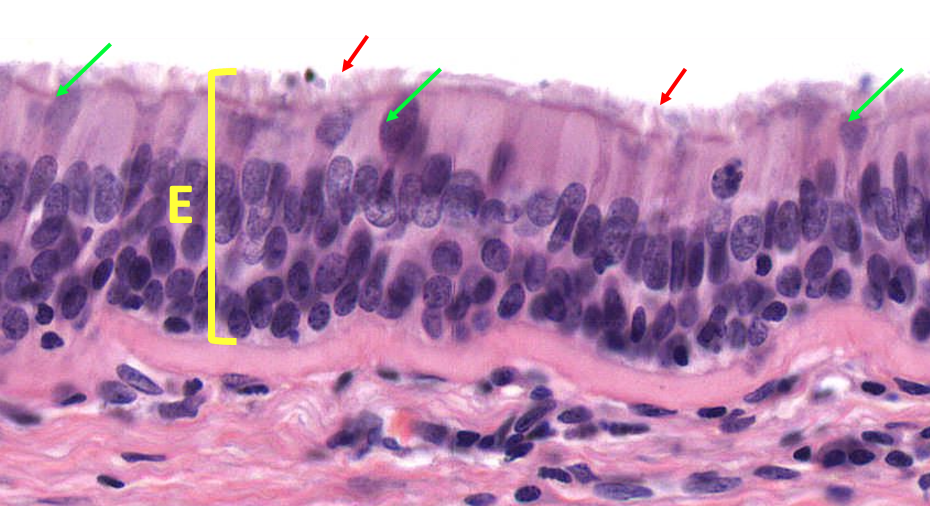
The airway epithelium is classified as a pseudostratified ciliated epithelium. Although it is a simple epithelium, it appears stratified because nuclei of different cells are at different heights, hence the term “pseudostratified” meaning “falsely (pseudo-) stratified”. An important function of this epithelium is the movement of mucus out of the respiratory tract. Mucus, which is secreted by goblet cells and submucosal glands, traps particles and pathogens. The beating of the cilia, located at the apical surface, moves the mucus toward the pharynx (throat) where it can be swallowed.
The image below shows tissue lining the wall of the trachea.
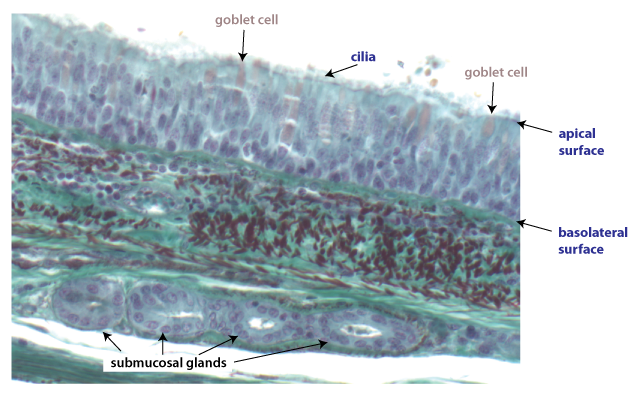
The pseudostratified ciliated epithelium of the airways can be seen in more detail in this higher-magnification image, also from the trachea.
The cilia on the surface of certain epithelial cells can be seen in this scanning electron micrograph.