3 Spondyloarthropathies
 Overview:
Overview:
As introduced in the spine section of the course, ‘spondyloarthropathy’ is an umbrella term used for a related group of diseases that are characterized by an inflammatory joint disease that is RF/anti-CCP negative (hence the term seronegative). These related conditions are frequently affecting the spine (or axial skeleton) as well as the entheses (insertion sites of tendons into bones) though peripheral joints may be involved as well. Extra-articular involvement with occular, GI and skin manifestations are common in this group of diseases. This group of disorders includes: ankylosing spondylitis, psoriatic arthritis, reactive arthritis, and inflammatory bowel disease-associated arthritis. Although given different names, these disorders can be thought of as existing on an overlapping disease spectrum
Clinical Presentation:
- Ankylosing Spondylitis (AS): the prototype disease for our purposes in MJBS. Ankylosis means ‘bony fusion’ and Spondylitis ‘spine inflammation’ referringto the fact that without treatment, these patients can progress to spinal fusion. (Rheumatologists further subdivide this group into those with and without radiographic findings as well as axial versus peripheral subtypes. These details are beyond the scope of this course but you may come across these terms in your Internal medicine or other clinical rotations.)
Clinical features of AS include the insidious onset of low back pain, usually before 40 years of age, associated with prominent morning stiffness, and improving with exercise and non- steroidal anti-inflammatory agents. Arthritis occurs in peripheral joints in approximately 1/3 of patients. Large joints lower extremity joints such as the sacroiliac (SI) joints, hips, knees and ankles are most often affected though shoulders and elbows and TMJ (jaw) joint can also be involved. Enthesitis may present as recurrent tendonitis or bursitis such as Achilles tendonitis or plantar fasciitis. Pathologically, enthesitis is characterized by inflammation where ligaments attach to bone and cartilaginous erosions secondary to formation of subchondral granulation tissue. Without appropriate treatment, the ongoing joint inflammation in patients with AS may progress to bony fusion (ankylosis) of affected joint structures due to inappropriate ‘healing’ responses. This can result in characteristic changes in the spine (see figure) overtime which are irreversible.

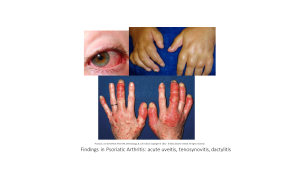
- Psoriatic Arthritis (PsA): though considerable overlap exists with the phenotype of AS including frequent presence of inflammatory back pain, and SI joint involvement, patients with psoriatic arthritis may have unique features including possible dactylitis (dactylitis = inflammation of an entire digit) and more prominent involvement of small joints, including the distal interphalangeal joints (DIPs) in fingers and toes. The rate of Psoriatic arthritis in patients with psoriasis has been difficult to quantify and ranges from 4-30% in certain cohorts. A high index of suspicion for possible joint involvement is warranted for any patients with psoriatic skin disease. Not all patients categorized as having psoriatic arthritis have active skin disease! Skin involvement can flare/occur independently from joint complaints in some patients. The presence of nail pits on exam is suggestive of risk for joint disease and is thought to indicate the presence of low grade inflammation at entheses in the fingers close to the developing nail bed.
- Reactive arthritis: The classic triad of urethritis (painful inflammation of the urteter), arthritis (often mono- or oligo-articular) and acute painful uveitis (inflammation of the anterior portion of the eye) 2-3 weeks following an infectious illness is known as reactive arthritis. Affected joints tend to be large joints and entheses can also be affected. While this is often a self-limited (resolving) illness, symptoms can last up to 6 weeks to several months in adult patients. Common implicated triggering infections include GI and GU pathogens such as Salmonella, Shigella and Campylobacter or Chlamydia/Gonorrhea. Patients tend to be HLA-B27 positive and may be at risk for repeat episodes of inflammatory arthritis with subsequent infections and/or progression to a more chronic/persistent disease such as AS. In most cases the inciting infection is often resolved (ie the process is post-infectious, immune mediated) but a more acute onset (days) should raise suspicion for a true infectious process. Neisseria gonorrhoeae in particular can spread from the GU track by hematogenous spread and lead to a disseminated infection characterized by septic arthritis and/or tenosynovitis (infectious inflammation of tendon sheaths)
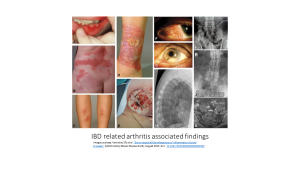
- Inflammatory Bowel Disease (IBD)-related arthritis (aka enteropathic arthrisits): This type of arthritis occurs in 10-20% of patients with Ulcerative colitis, or Crohn’s disease, but can also follow bacterial dysentery (aka reactive arthritis). Two main forms include:
- Peripheral arthritis, especially knees and ankles but also hips, usually associated with active bowel disease; may be associated with erythema nodosum, oral ulcers or uveitis (inflammation of the tissues in the eye from the anterior iris to the more posterior retina).
- Ankylosing spondylitis independent of bowel disease activity: in these patients, joint inflammation may precede overt bowel disease. (See section on extra-intestinal manifestations of AS above.)
All of these seronegative spondyloarthropathy patients may have extra-articular disease manifestations such as inflammatory eye disease (acute, painful uveitis), and or inflammatory bowel disease. Approximately 85-90% of AS patients are HLA-B27 positive, however, given the prevalence of this variant in healthy populations (5-12%) this test is not 100% sensitive or specific and should not be used to confirm or refute a diagnosis. (Top Tip: although enriched in patients with AS and related disorders, only 5-6% of HLA-B27 positive people will develop AS or a related inflammatory condition; patients who are HLA-B27 negative may also develop AS).
Pathophysiology:
The exact pathophysiology is unclear. There is clearly a genetic predisposition, especially with the HLA-B27 antigen, but not all HLA-B27 positive patients will develop disease indicating a role for environmental influences. Alterations in gut microbiome may play an initiating role in certain patients. Remembering from I&I, mucosal immunity is highly dependent on the Th-17 pathway and a dysregulated Th-17 type response is thought to be part of the pathogenesis in many patients. Therapeutic trials have shown the efficacy of Non Steroidal Anti-inflammatory agents, TNF-alpha blockers as well as certain Th-17 pathway cytokine blockers and Janus Kinas (Jak/STAT) signaling pathway blockers indicating roles for these chemical mediators in the pathophysiology of the disease. Mechanical stress and recurrent tissue injury at the entheses may play a role as well.
Diagnosis:
Once again diagnosis for each of these syndromes is largely clinical based on classic symptoms, findings of arthritis/enthesitis on exam. Laboratory studies may show the presence of HLA-B27 as well as elevated inflammatory markers (ESR, CRP) but these studies can be negative/normal. Imaging can be used to evaluate for bony changes on X-ray (SI joint sclerosis, bamboo spine in late ankylosing spondylitis), MRI is more sensitive for early inflammatory changes before Xrays demonstrate bony damage.
Treatment:
NSAIDs, biologic medications (TNF-alpha inhibitors, IL-17 inhibitors, JAk/STAT blockers), physical therapy to maintain mobility, exercise, and occasionally DMARDs for peripheral symptoms.
Complications:
If untreated, the inflammation in the spine results in structural destruction and reactive new bone formation in paraspinus ligaments (syndesmophytes) which can result in ankylosis (bony fusion). These patients are also prone to fractures due to osteoporosis from chronic inflammation. Untreated Ankylosing spondylitis can progress to spinal fusion, restrictive lung disease (due to fusion of costovertebral joints), and early cardiovascular disease related to the effects of ongoing low grade systemic inflammation.
