5 Crystalline Arthropathies
Overview:
The crystalline arthropathies, gout and ‘pseudogout’ (or calcium pyrophosphate deposition [CPPD] disease) are forms of joint pathology caused by deposition of certain types of crystals in joint tissue causing an acute inflammatory synovitis. Over time, repeated bouts of inflammation lead to chronic tissue changes (tophi) and joint destruction
GOUT:

- Gout occurs in 3.9% of US adults and is the most common inflammatory arthritis in men over 40 years old. It is triggered by deposition of monosodium urate (MSU) crystals in joints, bursae and tendon sheaths
- KEY FACT: Uric acid forms monosodium urate crystals at >6.8mg/dL at 37°C
- Clinical Presentation:
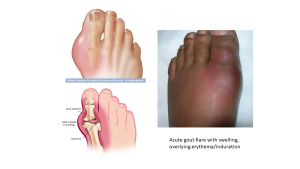
Gout occurs in 3.9% of US adults and is the most common inflammatory arthritis in men over 40 years old. It is triggered by deposition of monosodium urate (MSU) crystals in joints, bursae and tendon sheaths. Gout tends to present with acute onset of joint pain, redness, swelling, and warmth. In gout, the first metatarsophalangeal (MTP) joint is the commonly affected (“podagra”) but any joint can be affected.
 Gout can be thought of as occurring in 4 progressive stages over time:
Gout can be thought of as occurring in 4 progressive stages over time:
-
-
- Aysmtomatic hyperuricemia (can be years)
- Acute gouty arthritis – usually mono articular, flares come and go
- Inter-critical periods
- Chronic gout arthritis (with accumulation of tophi – See figure below) – can me polyarticular, hands, feet knees and elbows
-

- Pathophysiology:
Gout: Hyperuricemia leading to monosodium urate crystal deposition in tissues. Hyperuricemia may be due to increased production of uric acid or decreased excretion. Certain drugs in particular are notable for decreasing uric acid excretion including thiazide or loop diuretics (certain anti-hypertensive medications), cyclosporine, etc in particular. Factors such as male sex, hypertension, chronic kidney disease, type II diabetes, obesity and excessive alcohol intake may also contribute to increased uric acid levels. Macrophages in the tissues engulf the crystals which causes activation of DAMP-related pathways, in particular leading to upregulation of the inflammasome and increased IL-1 production.
- Diagnosis:
- ‘Gold standard:’
- joint arthrocentesis for synovial fluid analysis
- fluid demonstrates intracellular negatively birefringent needle-shaped crystals of uric acid
- (Intracellular means you must observe white cells engulfing the crystals!)
- ‘Clinical’ diagnosis of acute gout can be made in patients with a suggestive history:
- Right demographics, as detailed above
- First presentation usually monoarticular (80-95%), lower extremity predominant (overtime, when patients have chronically uncontrolled gout, attacks can become polyarticular – see more info below!)
- 1st MTP involvement common (90% eventually)
- Bursitis (olecranon, knee), tendonitis
- Hyperuricemia (serum uric acid > 6.8 mg/dL) – though uric acid levels may be normal during an acute attack due to deposition in joints
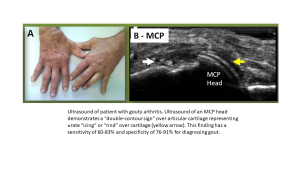
- Characteristic imaging results (erosions on X-ray, double contour sign on ultrasound)
- ‘Gold standard:’
- Treatment:
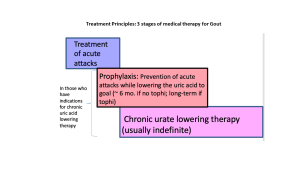
Acute gout: treatment is aimed towards decreasing inflammation with NSAIDs, colchicine, corticosteroids.
Chronic gout: treatment is aimed at decreaseing uric acid levels through lifestyle modifications as well as certain urate lowering medications like Allopurinol or febuxostat can be started. It is important to use prophylactic treatment with anti-inflammatory medications when initiating urate lowering therapy as the changes in distribution of uric acid can precipitate a gouty flare!
- Complications:
Chronic joint damage, tophi (gout), renal complications (uric acid can accumulate in kidneys leading to kidney disease), and increased cardiovascular risk.
PSEUDOGOUT
- Clinical Presentation:
Pseudogout is more likely to affect older individuals (>50 years). Other risk factors include hyperparathyroidism, joint trauma and hemochromatosis. Attacks can be similar to those of acute gouty flare but often involves the knee or wrist and can be more subacute in presentation.
- Pathophysiology:
Pseudogout: Calcium pyrophosphate crystal deposition within the joint space due to altered cartilage metabolism. Chronic degeneration of the joint can result in pseudosteoarthritis
- Diagnosis
Once again gold standard is joint arthrocentesis for synovial fluid analysis with fluid demonstrating positively birefringent rhomboid crystals of calcium pyrophosphate. Other suggestive findings include Xrays demonstrating cartilaginous calcifications known as chondrocalcinosis
- Treatment:
Pseudogout: NSAIDs, colchicine, intra-articular corticosteroids.
