1
- Overview:
Osteoarthritis (OA) is the most prevalent form of chronic arthritis, affecting over 32 million people in the United States. OA historically has been also called degenerative joint disease (DJD) or osteoarthrosis and is characterized by the degeneration of joint cartilage and underlying bone. OA is associated with aging and with progressive abnormalities in the joint surfaces. Injury and overuse may play a role in accelerating the disease as well. The etiology of OA is incompletely understood, but there are a variety of factors known to play an important role in the pathogenesis, including biomechanical factors, proinflammatory mediators, and proteases. Although OA is not inherently an autoimmune or primarily immune-mediated disease, increasing evidence suggests that there is a role for local inflammatory responses in the propagation of tissue destruction (think back to the I&I concepts of damage-associated molecular pattern or DAMPs and how those can trigger inflammation). However, OA is classically distinguished from primary immune-mediated diseases like Rheumatoid arthritis, Spondyloarthritis and JIA by its lack of significant inflammatory cells in the synovium and synovial fluid.
- Clinical Presentation:
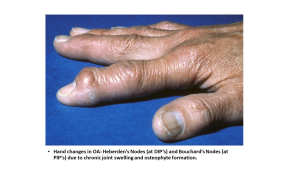
OA generally produces an aching type of pain that is worse with use, better after rest and gets worse as the day goes on. The onset of pain is generally gradual though patients may present to care for more acute episodes of pain related to overuse. OA most commonly occurs in larger weight bearing joints such as the hip and knees (especially in males) and in distal finger joints including distal interphalangeal (DIP), proximal interphalangeal (PIP) and the first carpometacarpal (CMC) joints (especially in females). These site predilections may reflect the effect of trauma from repeated mechanical stress; a good history including occupation, lifestyle/sports and hobbies can help identify which joints are more likely to be affected in a given individual. A small effusion may be present, though the cell counts are low (<1000-2000 WBC from a synovial aspirate). Crepitus and bony enlargement are common in advanced disease.
 Pathophysiology:
Pathophysiology:
When the joint surface is examined microscopically, one sees fibrillation, fissures, and chondrocyte clones in the articular cartilage as well as debris in the joint cavity. On a biochemical level one finds a decrease in glycosaminoglycan content as well as decreased water content in the cartilage.
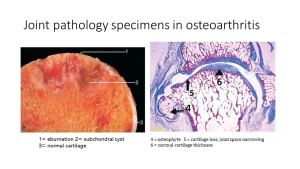
Functionally, the articular cartilage loses its weight-bearing ability and the joint loses its range of motion. Over time, loss of cartilage may lead to areas of exposed bone. When examining a pathology specimen this is called eburnation. The subchondral bone reacts with an attempt to reinforce itself creating areas of thickening or sclerosis. However, over time tiny fractures in the bone surface form and allow synovial fluid to be forced in past the surface and into the less dense areas of bone beneath resulting in subchondral cysts. Reactive new bony formation can also occur at the edge of the bone creating bony protuberances called osteophytes.
- Diagnosis:
Diagnosis of OA is primarily clinical based on history and physical exam. X-rays show joint space narrowing, osteophytes, and subchondral sclerosis. MRI may be used in atypical cases. Screening labs and serologic testing may be sent to differentiate from inflammatory arthritis. Findings of elevated ESR, CRP, or positive serologies should prompt consideration of alternative diagnoses.
 Treatment:
Treatment:
Non-pharmacological or lifestyle modifications are often first line and include weight management, physical therapy, low-impact exercise, joint protection strategies.
Pharmacological: NSAIDs, acetaminophen can be used for pain relief. The role of intra-articular corticosteroids for pain relief is controversial, with some concern that repeated use can lead to faster disease progression. Surgical joint replacement (arthroplasty) can be performed for advanced disease in joints such as hips and knees and even shoulders, elbows and wrists. The quality and durability of joint replacement options continues to improve though some joints such as fingers and ankles are still more difficult to replace.
- Complications:
Chronic pain, joint deformities, reduced mobility, disability, and decreased quality of life.
