2 Rheumatoid Arthritis
- Overview:
Rheumatoid Arthritis (RA) is an inflammatory, autoimmune arthritis of uncertain etiology. RA is thought to arise from a complex interplay between genetic factors and certain environmental exposures. For example, the HLA-DR4 allele variant (encoded by the HLA-DRB1 gene) is associated with a modest increase in RA risk; smoking also is associated with a several fold increased risk of RA. RA is characterized by the development of a profuse and erosive synovitis that destroys joints if left untreated. In addition, the inflammatory state induced in RA may involve multiple extra-articular organ systems in certain patients.
- Clinical Presentation:
Clinical features of the disease include persistent polyarthritis, symmetric involvement, prominent morning stiffness, painful joint motion, and muscle atrophy (wasting) around affected joints. Patients may describe loss of grip strength due to pain inhibition. Symptoms may improve somewhat with use, heat and NSAIDs. Swelling, warmth, and erythema can be present but may be minimal in early stages. Later in advanced disease the patient may have subcutaneous nodules (rheumatoid nodules), joint deformities, and the involvement of additional systems as listed below. Systemic symptoms may include fatigue, low-grade fever, and weight loss.
In terms of joints affected, the classic presentation is arthritis of the small joints of the hands (PIPs and MCPs), wrists, and feet (MTPs), especially early on in the disease course. Interestingly, distal-interphalangeal (DIP) joint involvement is rare and should prompt consideration of alternative diagnoses.
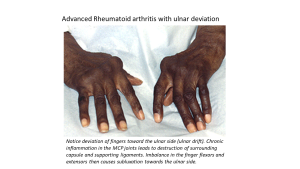
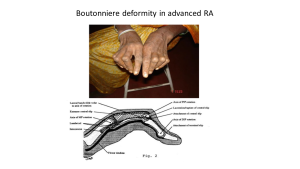
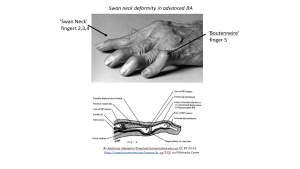
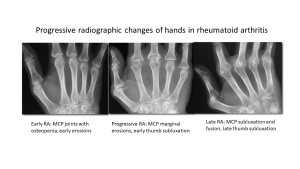
Other joints, including elbows, shoulders, knees, and hips, can also be affected, often later on in disease. The facet joints in the cervical spine are another common site of inflammation in RA though other axial sites such as the sacroiliac joints and thoraco-lumbar spine are less commonly affected in this specific form of inflammatory arthritis and should lead to suspicion for a spondyloarthropathy type disorder (next chapter). Over time, untreated inflammation can lead to erosive changes of the bones and joint deformities including ulnar deviation of fingers and the wrist and characteristic finger pathologies due to disruption of tendinous structures in close proximity to the joints. (See figures).
Patients with RA may develop inflammatory changes in other organs outside the joints. Many of these manifestations are thought to be due to a low-grade form of secondary vasculitis due to immune complex formation and deposition in blood vessels. Skin involvement in RA may include rheumatoid nodules, soft tissue swellings that are subcutaneous and arise along tendon sheaths, in bursae, and about bony prominences. Ocular manifestations also occur and may include forms of conjunctivitis or scleritis. Respiratory, cardiac, renal, gastrointestinal, and neurologic system involvement may also be seen late in disease.
- Pathophysiology:
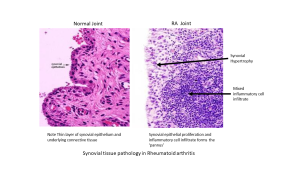
The understanding of the pathophysiology of RA is evolving and may involve induction of inflammation at mucosal sites such as the lungs that then leads to a more general loss of self-tolerance. In particular, enzymes known as protein arginine deaminases (PADs) create post-translational modifications of proteins known as citrullination. The citrullinated proteins by PAD may serve as ‘neoantigens’ that are recognized as foreign by the adaptive immune system and generate antibody production. Studies have indicated that antibodies to these citrullinated proteins (anti-CCP antibodies or ACPA’s) can be found in the serum years prior to diagnosis and may represent an early pre-symptomatic stage. The exact link to subsequent synovial inflammation is unclear but may be due to additional environmental or genetic factors. Antibody-antigen (immune complex) deposition in synovial microvasculature may produce injury resulting in larger regions of synovial tissue injury and exacerbation of the inflammatory response. Though T-cells may initiate the immune actions in the rheumatoid joint, neutrophil activation results in the release of multiple enzymatic factors and proteases which begin the degradation of the joint surfaces and the surrounding ligaments and tendons. The synovium becomes hypertrophic and edematous or engorged, with numerous villi protruding into the joint. Activated fibroblasts make up the majority of cells present within the synovium. These fibroblasts form an aggressive granulation tissue known as pannus which erodes the surrounding cartilage surfaces and subchondral bone within joints. As the joint surfaces are eroded, the subchondral bone is eroded by pannus and resorbed by osteoclasts, and the surrounding soft tissues are attenuated by the erosive and infiltrative nature of the disease process; pain and progressive disability typically result. The immune system attacks the synovial membrane, leading to synovitis, pannus formation, and cartilage and bone erosion. Key inflammatory mediators in this process include TNF-alpha and IL-6.
- Diagnosis:
Diagnosis can be made through clinical exam and laboratory testing. Laboratory abnormalities may include: positive anti-CCP anti-bodies (approximately 50-75% of patients), elevated rheumatoid factor in the serum (IgM autoantibody to IgG, found in about 80% of adult patients), anemia of chronic disease, elevated erythrocyte sedimentation rate (ESR) and/or C-reactive protein. Although positive tests for antinuclear antibody (ANA) are found in 25% of RA patients, ANA testing is not a good screening test for arthritis itself and is more commonly sent in patients presenting with arthritis to assess for the presence of a systemic autoimmune disease such as SLE. Synovial fluid in RA joints is inflammatory, usually demonstrating 2,000 to 50,000 white cells per cubic millimeter.
Imaging studies such as X-ray, MRI, and ultrasound can be used to assess for joint damage. Early in the disease course, plain radiographs are often normal as the synovitis involves soft tissues that are not well visualized on plain films. Occasionally a large effusion can be visualized on a plain film but lack of an effusion on plain films does not rule out arthritis! If left untreated, patients with RA will develop bony changes due to destruction of cartilage and erosion into underlying bony structures. These changes may be seen on radiographs over time. In contrast to osteoarthritis, radiographic findings in rheumatoid joints include symmetric marginal erosions, subchondral or periarticular osteopenia, and in severe disease, subluxation or dislocation of joints on radiographs. Joint space narrowing occurs over time but tends to be more uniform or concentric than that observed in OA which can be more focal. In early disease joint inflammation may be assessed by MRI with gadolinium which can demonstrate effusion, synovial enhancement and bony edema at affected joints. Increasingly bedside MSK ultrasound is also being used in clinical care to demonstrate the presence of subtle effusions, subclinical synovial enhancement and early bony erosions.
- Treatment:
The goals of treatment are to control inflammation in order to preserve joint function, prevent progressive joint changes and decrease risk of secondary complications. There are now a wide number of options for treatment with so called Disease-modifying antirheumatic drugs (DMARDs) like methotrexate, biologics (TNF-alpha and other cytokine blocking agents), jak-kinase inhibitors etc. These medications will be reviewed during the pharmacology sessions this week. It is important to know that while NSAIDs can be helpful for symptom control they are not adequate to prevent long term complications such as erosions in this type of arthritis. Corticosteroids can play a role in symptom management but should be used in the lowest possible doses and for short durations given the significant side effects of longer term treatment.
- Complications:
RA patients with untreated inflammation can develop joint deformities, osteoporosis, anemia and interstitial lung disease. Ongoing chronic inflammation in RA patients is also linked to secondary co-morbidities such as early cardiovascular disease (atherosclerosis, coronary artery disease) as well as an increased risk of malignancy.
