7 Lab 5 Oculomotor Control and Anatomy (under construction 8/25/25)
Specific Learning Objectives
- Identify the major foramina of the orbit and the structures which pass through them.
- Distinguish the extraocular muscles and describe the function and innervation of each, including the levator palpebrae superioris muscle.
- Describe the H-test, including how it is used to isolate and test the integrity of each of CN III, IV & VI.
- Compare common clinical features associated with a lesion to cranial nerves III, IV, VI, their anatomical pathways or brainstem nuclei of origin.
- Compare saccades, smooth pursuit, and vergence movements
- Describe the clinical features of internuclear ophthalmoplegia and explain the neural circuitry that underlies this syndrome
- Define the terms “right-way eyes” and “wrong-way eyes”; localize the lesions that cause these conditions including both the supratentorial and infratentorial structures, and explain why these symptoms occur.
- Outline the parasympathetic and sympathetic pathways of the orbit, including target structures and their functions. Explain how damage along the sympathetic pathway leads to the three core symptoms of Horner’s syndrome.
Bones and Foramina of the Orbit
Review the bones and foramina of the orbit.
3 question quiz:
Extraocular muscles, movements and nerves
This first movie reviews a dissection of the orbit to demonstrate the location of structures in the orbit.
This movie focuses on details of the actions of the muscles.
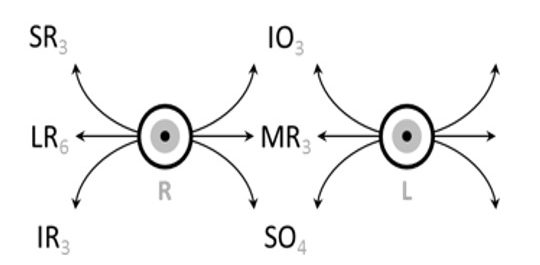
Clinical testing of extraocular muscles is accomplished with the H-test, diagramed below; the cranial nerves that innervate the muscles as well as the abbreviations of the muscles ar shown.
SR Superior rectus – Oculomotor nerve
LR Lateral rectus – Abducens nerve
IR Inferior rectus – Oculomotor nerve
IO Inferior oblique – Oculomotor nerve
MR Medial rectus – Oculomotor nerve
SO Superior oblique – Trochlear nerve
And here is an image showing normal eye movement responses in an H test.
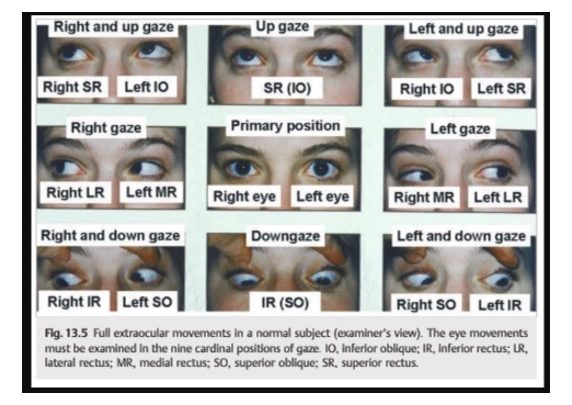
Check your knowledge about muscle testing in the H-test:
Drag and drop the muscle tag (that includes the cranial nerve that innervates it) to the appropriate direction of testing.
Here is a tool that allows simulation of eye position and movement after nerve damage-give it a whirl!
Review the radiology of the orbit and eye with this drag and drop image.
The palpebrae
Cranial Nerve Palsies affecting Eye Movements
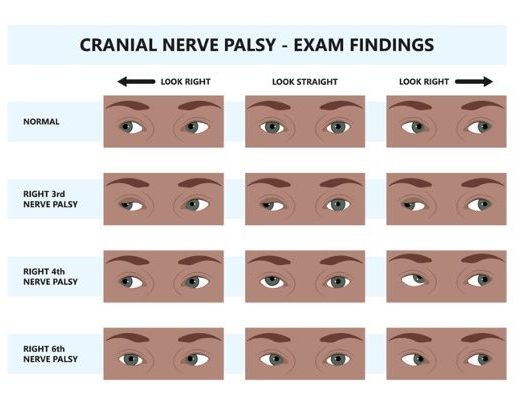
Lesions of individual cranial nerves result in changes in eye position at rest (in the primary position of the H test) along with abnormalities in conjugate movement with attempted saccades. In most cases, when the two eyes are not aligned correctly, the patient experiences diplopia (double vision). Sometimes, patients will subconsciously adopt a new head position that engages the vestibulo-ocular reflex to bring the eyes back into alignment and resolve the diplopia.
When presented with an image that appears to show eye misalignment, it is important to understand the context and what eye movement the patient may be attempting to execute. Pay attention to both eyes, and any indications in the image caption or graphic design of whether the image shows eyes at rest or attempting a directional movement.
For example, in the image below, right eye medial deviation results when an intact subject looks to the left (see top row, right image). However, right eye medial deviation at rest (bottom row, center image), while looking the same in a graphic or photo, may result from a right abducens nerve palsy, and would be due to unopposed action of the medial rectus muscle innervated by the unaffected left oculomotor nerve. Checking both eyes can help clarify the examination. We suggest you work through the image below to learn how to distinguish the manifestations of lesions of cranial nerve 3,4, and 6.
Check your understanding of lesions to cranial nerves driving extraocular muscles.
Gaze control
Gaze refers to the coordinated movement of the eyes and head to maintain a stable view of an object. The intricate control of gaze involves complex neural pathways, including cranial nerves III, IV, and VI, which innervate the extraocular muscles, gaze centers in the brainstem, and cortical control areas. These movements are categorized into conjugate and disconjugate gazes.
- Conjugate Gaze: This describes the coordinated movement of both eyes in the same direction, such as when you look left or right. It’s essential for maintaining binocular vision and is controlled by gaze centers in the brainstem, such as the paramedian pontine reticular formation (PPRF) for horizontal gaze and the rostral interstitial nucleus of the medial longitudinal fasciculus for vertical gaze. These centers ensure the eyes move as a single unit.
- Disconjugate Gaze: Also known as vergence, this is the movement of the eyes in opposite directions. For example, when you focus on a nearby object, your eyes move inward (convergence), and when you look at a distant object, they move outward (divergence). Disconjugate gaze is vital for depth perception and maintaining a single, focused image as the distance to an object changes.
Here is a video on horizontal conjugate movement
Brainstem Lesions and Gaze Palsies
- Internuclear Ophthalmoplegia (INO): This is a classic finding from a lesion in the medial longitudinal fasciculus (MLF), the heavily myelinated tract that connects the CN VI nucleus to the contralateral CN III nucleus. In unilateral INO, when the patient attempts to look to one side, the abducting eye shows nystagmus, while the adducting eye fails to move past the midline. Multiple sclerosis is a common cause in young adults, while stroke is more common in the elderly.
- One-and-a-Half Syndrome: A lesion in the pons that affects both the MLF and the adjacent abducens nucleus/paramedian pontine reticular formation (PPRF) on the same side. The patient will have a total horizontal gaze palsy to the side of the lesion and an internuclear ophthalmoplegia on attempted gaze to the other side. The only remaining horizontal movement is abduction of the eye opposite the lesion.
Autonomically innervated structures of the orbit and eye
Recall the sympathetic innervation of the eye originates from the lateral horn at the T1 spinal cord level which contains the cell bodies of the pre-ganglionic neurons. These neurons synapse in the superior cervical ganglion, the most rostrally-located ganglion within the sympathetic chain. Axons of the post-ganglionic neurons form a plexus around and follow the internal carotid artery superiorly into the cranial vault. This explains why a carotid dissection may disrupt sympathetic function and may result in Horner’s syndrome.
Clinical correlate: Horner’s syndrome is the result of damage anywhere along the sympathetic pathway to the face (see image on the above). The classic triad of symptoms is mild ptosis (drooping eyelid), anhidrosis (lack of sweating), and miosis (constricted pupil) due to the decreased function of the superior tarsal muscle (a smooth muscle that assists with eyelid elevation), facial sweat glands, and the dilator pupillae, respectively.
Contrast this with the symptoms of CN III palsy—severe ptosis, “down and out” position of the pupil, and mydriasis (dilated pupil)—related to the loss of somatic motor and parasympathetic innervation. Notice how damage to one division of the autonomic nervous system shifts the balance in favor of the functional division (e.g. pupil presentation).

Lacrimal gland