9 Clinical Nutrition
Introduction
Nutrition is one of the areas in medical education which integrates many organ systems and content areas. As such, you will likely recognize many processes discussed in this chapter from other blocks. The goal of this chapter is to discuss micronutrient and macronutrient functions and conditions of excess and deficiency. Furthermore, we will focus on the nutritional assessment as a means to evaluate for nutritional deficiencies, with a focus on malnutrition and components of a healthy diet. Please note, micronutrient function and situations of excess and deficiency are covered more heavily on the boards when compared to other topics in clinical nutrition.
It should be noted that vitamin deficiencies in their pure form, however, are rarely seen in current American clinical practice except in unusual circumstances. Similarly, vitamin excess with clinical manifestations is also rare.
Nutrient Terminology
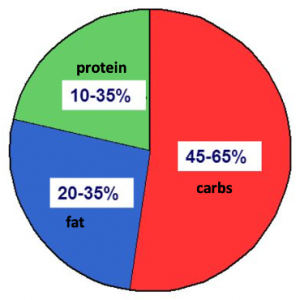
Nutritional requirements have been expressed in the past as the RDA (Recommended Dietary Allowance), standards developed by the Food and Nutrition Board of the National Academy of Sciences. The RDA for a micronutrient or macronutrient is the amount that is necessary to maintain normal function and prevent biochemical or clinical signs of deficiency states. The goal of RDAs to ensure adequacy (prevent deficiency) and, because nutrient requirements vary between individuals they are calculated to provide the amount of nutrients that are sufficient to meet the basic needs of the vast majority (97%) of the population, without causing toxicity. The Tolerable Upper Intake Level (UL) is the highest level of intake that is likely to pose no risks of adverse health to almost all individuals in the general population and an Adequate Intake (AI) is an intake suggested by observation or experiment as sufficient to meet nutritional goals even if insufficient scientific evidence is available to define an estimated average requirement. Finally, the Acceptable Macronutrient Distribution Range (AMDR) is the range of intake for a particular energy source that is associated with reduced risk of chronic disease while providing intakes of essential nutrients (Figure 1).
Macronutrients, Micronutrients and Trace Elements
Dietary nutrients can be broadly divided into two categories: macronutrients and micronutrients. Dietary macronutrients include carbohydrates, proteins and lipids. Macronutrients represent the major sources of energy (or calories) in the diet. Figure 1 shows the AMDR for macronutrients. Macronutrient proportions are often emphasized by public health guidelines and popular diets, though globally, there is wide variation in the proportion of macronutrients associated with adequate growth and development.
Micronutrients consist of vitamins, minerals, electrolytes and trace elements. These nutrients facilitate optimal cell metabolism, maintain cell integrity, and prevent cell death. Vitamins are not synthesized and therefore must be ingested. The vitamins are roughly classified as fat-soluble (A,D,E,K) and water-soluble (vitamin C and B vitamins).
In general, favorite vitamin topics for boards include vitamin b12 deficiency, vitamin D metabolism, vitamin K deficiency, thiamine deficiency, vitamin C deficiency, vitamin B6 deficiency, vitamin A deficiency, folate deficiency and niacin deficiency. Vitamin B12, folate and Vitamin K are covered in Blood & Cancer, we will touch on them in this course as well.
Eating a variety of foods is the best way to get all the vitamins and minerals needed. Whole or unprocessed foods such as fresh vegetables, fruits and whole grains are the best way to ensure optimal intakes of vitamins and minerals.
Macronutrients – Carbohydrates
The majority of living matter on the planet is classified as carbohydrate (CHO) and, accordingly, carbohydrate constitutes the largest portion of the human diet. Carbohydrates provide 4 kcal of energy per gram consumed. Depending on the pattern of food intake, carbohydrates account for 45 to 70% of caloric intake. The average American ingests 300 grams of carbohydrates daily, compromising 1000 to 1200 kilocalories, or about 55% of the recommended daily energy intake. The National Academy of Sciences has suggested an RDA for carbohydrate of 130 grams per day in adults and an acceptable range of carbohydrate intake as 45 to 65% of total energy intake. Preferred dietary sources of carbohydrates are whole grains, vegetables, and fruits. Added sugars should be avoided.
Naturally occurring carbohydrates include simple sugars, starch, fiber (table 1). Simple sugars can be further divided into monosaccharides (glucose from cane sugar, fructose from fruits, honey and many sweeteners containing high fructose corn syrup) and disaccharides (sucrose from sugar cane and beets, and lactose from milk). Starches are long polymers of glucose and are the principal form of carbohydrates in cereal grains and vegetables. Fiber is poorly digestible or undigestible plant components.
There are generally two types of fiber: soluble fiber and insoluble fiber. Soluble fiber, also known as functional fiber, dissolves in water and turns into gel in the digestive tract. Soluble fiber can coat the gastrointestinal lining, may sometimes impair absorption of nutrients, but does have beneficial effects on blood sugar and blood lipids. Insoluble fiber, also known as dietary fiber, passes through the digestive system intact, adding to the bulk of stools. Digestible fiber prevents constipation. Examples of dietary fiber include whole wheat flour, wheat bran, cauliflower, green beans. The Food and Drug administration recommends 20 to 25 grams of fiber intake per day from raw vegetables and unprocessed grains. The American diet is known to be low in dietary fiber. There are many health benefits of dietary fiber. Fiber is known to decrease mortality in people with diabetes, fiber lowers LDL cholesterol. LDL cholesterol causes atherosclerosis and leads to cardiovascular disease. Therefore, adequate fiber intake and protect against cardiovascular disease.
| Carbohydrate Type | Subtype | Major Dietary Sources |
| Sugar |
|
Most dietary carbohydrates Dairy products, sugar beets Fruits, vegetables, honey Table sugar Milk sugar |
| Oligosaccharides |
|
Wheat and rye products, onions, garlic, legumes, nuts, some fruits and vegetables |
| Starch |
|
Cereals, tubers |
| Fiber |
|
Legumes, oats, barley, fruits/vegetables, bran of cereal grains, peels |
| Polyols |
|
Artificial sweeteners, apples, stone fruits, cauliflower, mushrooms and snow peas |
Table 1. Carbohydrate classification
Macronutrients – Dietary Lipids
Dietary lipids provide an important source of energy (9 kcal/gram), and serve as precursors or constituents of cell membranes and steroid hormones, prostaglandins, thromboxanes, prostacyclin, and leukotrienes. Dietary fat is also important to optimize absorption of fat-soluble vitamins. Recommended AMDR for fat ranges from 20-35% of total energy intake for adults (Figure 1).
Greater than 95% of ingested fats are triglycerides. The major categories of triglycerides are (1) saturated fats, (2) monounsaturated fats, (3) polyunsaturated fats. Saturated fats are primarily derived from animal products. Beef, pork and dairy products contribute substantially to the intake of saturated fats in this country. There are also plant sources of saturated fats including palm oil, coconut oil and cocoa butter. Saturated fat can be produced endogenously, and is therefore not essential in the diet. Saturated fat increases LDL cholesterol, which can increase the risk of cardiovascular disease. Dietary intake of saturated fat should be limited.
Trans fatty acids are physiologically similar to saturated fats, and result from the reduction of polyunsaturated fatty acids for use in hard margarines. Trans fatty acids are found in fast foods, cakes and pastries, and deep fried food. They are known to increase the risk of heart disease and raise LDL cholesterol, the American Heart Association recommends complete avoidance of trans fat.
Unsaturated fats are divided into monounsaturated fats and polyunsaturated fats. Monounsaturated fats are found in olive and canola oils, avocados and nuts. Polyunsaturated fats our derived primarily from plant sources (corn, safflower and sunflower oils). the fat stripe from fish and canola oil are rich sources of polyunsaturated fats. Soybeans also contain significant saturated fat. Unsaturated fats have many health benefits period they lower the rates of cardiovascular disease and all-cause mortality. They are known to lower LDL cholesterol and triglyceride levels. There are two fatty acids that cannot be synthesized by human cells. Linoleic and linolenic acids are considered essential fatty acids. While absolute requirement of these essential fatty acids is not known, very small amounts of dietary fat seem to be enough to prevent deficiency syndromes.
Macronutrients – Protein/Amino Acids
Proteins function as constituents for cell structure, enzymes, antibodies, hormones, neurotransmitters, and nucleic acids. Proteins also transport many substances within the blood. Proteins are composed of amino acids. There are 20 amino acids that are needed for protein synthesis in humans. Nine of these amino acids are indispensable (essential) and must be obtained from diet because they cannot be synthesized by the body. The remaining amino acids can be synthesized from other amino acids or metabolic precursors. An amino acid is partially indispensable if it can be synthesized endogenously but not in the quantity that fulfills the body’s requirement (table 2).
| Indispensable Amino Acids | Partially Indispensable Amino Acids | Dispensable Amino Acids |
|
|
|
Table 2. Amino acid classification
In addition to serving as building blocks, dietary protein can also serve as a fuel source. The carbon skeletons of amino acids are an important substrate for gluconeogenesis. Excess dietary protein, as well as metabolized protein from muscle breakdown, is converted to glucose. Protein provides four kilocalories per gram of energy content. Dietary protein provides 10 to 20% of energy intake in the American diet. The recommended dietary allowance for protein is 0.8 grams per kilogram of body weight. As a proportion of macronutrient intake, 10 to 35% of total calorie intake as protein in adults is usually sufficient.
Micronutrients – Fat Soluble Vitamins
Fat soluble vitamins include Vitamins A, D, E, K. Fat soluble vitamin deficiencies develop from conditions that lead to fat malabsorption (cystic fibrosis and celiac disease are examples). Fat soluble vitamins are found in fatty foods such as oily fish, vegetable oils, dairy foods, liver and animal fats including butter and lard. Fat soluble vitamins dissolve in fat and can be stored in the body for longer periods than water soluble vitamins because adipose deposits are slowly metabolized.
Vitamin A (beta-cartone, aka retinol)
Vitamin A is needed for gene expression which influences cell differentiation, immunity, hematopoiesis, and growth and development. It directs cells away from proliferation and toward maturation. Thus, deficiency of Vitamin A can lead to dysregulated cell differentiation which can particularly affect epithelial cells. Also critical in the visual cycle (retinal function), and embryonic development. Dietary sources of vitamin A include liver, dairy, eggs, yellow orange and red vegetables, some fruits.
Due to its broad effects, deficiency of vitamin A may have many manifestations due to dysregulated maturation of epithelial cells. The symptoms include: keratomalacia (softening/clouding of the cornea), xeropthalmia (dryness of conjunctiva and cornea), night blindness, dry/rough skin with hyperkeratotic eruptions, and increased risk of infection (nutritionally acquired immunodeficiency) due to decreased barrier from infection from poorly differentiated epithelial cells as well as decreased immune cell production. Vitamin A deficiency is the leading cause of preventable blindness in young children. Additionally, vitamin A deficiency is associated with increased rates of death from severe infections, especially in Africa and South-East Asia. Vitamin A supplementations is recommended for populations endemic for vitamin A deficiency.
Toxicity of vitamin A can be either acute or chronic. With acute vitamin A toxicity symptoms include nausea, vomiting, vertigo, blurred vision. Chronic vitamin A toxicity can cause alopecia, dry and scaly skin, hepatic toxicity and liver enlargement. Vitamin A is known to be teratogenic and fetal effects include cleft palate and cardiac abnormalities.
Vitamin A can be used to treat various medical conditions. All-trans retinoic acid is used to treat acute promyelocytic leukemia. Isotretinoin is used to treat acne
Vitamin D
Vitamin D functions include gene expression, calcium metabolism, and immunity.
Vitamin D is a steroid hormone produced by the skin. The skin uses sunlight 2 make vitamin D3 from 7-dehydrocholesterol. Vitamin D is also present in fortified dairy, fish, liver, Cod liver oil.
Vitamin D is essential for intestinal absorption of calcium and phosphate. Without vitamin D, bones are unable to appropriately mineralize and hypocalcemia (low serum calcium) may develop. Without appropriate mineralization, osteomalacia (adults) or Rickets (children) will develop.. Vitamin D excess can lead to excess calcium absorption from the gut and hypercalcemia (high serum calcium) can develop.
Vitamin E
Vitamin E functions to protect lipid rich membranes (eg lipoproteins) by inactivating oxygen free radicals in membranes. It is found in vegetable oils, nuts, grains, wheat germ. Vitamin E deficiency is very uncommon. In rare cases, peripheral neuropathy and hemolysis can occur. Groups at risk for vitamin E deficiency are those with severe malnutrition, fat malabsorption syndromes (e.g., cystic fibrosis), and genetic defects of alpha-TPP, the protein that facilitates the incorporation of Vitamin E into the VLDL particle. Toxicity can occur when intake exceeds 1000 mg/d. With toxicity, there is increased platelet dysfunction and risk of bleeding (by interfering with the absorption and function of Vitamin K).
Vitamin K
Vitamin K is an important cofactor in blood coagulation and coenzyme in synthesis of proteins involved in bone mineralization. Vitamin K is derived from gut bacterial synthesis, green vegetables, cooking oils (soy, canola, olive). Because there are several coagulation factors that are dependent on Vitamin K (Factor II, factor VII, Factor IX, Factor X) deficiency leads to clotting disorder leading to hemorrhage. There is no known toxicity, but Vitamin K interacts with warfarin and therefore it is important to eat a similar amount of vitamin K every day for people who are taking warfarin.
Newborns high risk for Vitamin K deficiency due to low hepatic synthesis of clotting factors, poor placental transfer, lack of adequate supply in breast milk. Synthetic vitamin K is given at birth.
Micronutrients: Water-Soluble Vitamins
Water soluble vitamins dissolve in water, are rapidly eliminated, largely in the urine and have limited stores (with the exception of B12 and B9, see below). A person requires a daily intake of water-soluble vitamins to maintain adequate stores. Water soluble vitamins are found in most foods, but especially milk, vegetables, fruit and grains. Unlike fat-soluble vitamins, water soluble vitamins can be destroyed by oxidation (air exposure) or heat. Cooking, especially boiling, can cause the loss of substantial water-soluble vitamins. The best cooking methods to preserve optimal amounts of vitamins are grilling, microwaving, and steaming.
The B vitamins are heavily involved in energy production and hematopoiesis. They act as co-enzymes, molecules that enable enzyme function. They participate in a variety of reactions including redox reactions, generation of leaving group potential, carboxylation reactions, rearrangements, acyl activation and transfer, and one carbon transfers.
Vitamin C
Vitamin C functions as antioxidant and is involved in collagen synthesis. The dietary sources of vitamin C are fruits and vegetables. Vitamin C deficiency can lead to a condition called scurvy characterized by swollen gums, bruising, petechiae, hemarthrosis, anemia, poor wound healing, subperiosteal hemorrhages. Groups at increased risk for deficiency include elderly, people with diabetes, and smokers. Vitamin C is the only nutrient with a specific RDA for smokers. Individuals who smoke required 35 mg/day more vitamin C than people who do not smoke. For unclear reasons, diabetes in associated with increased turnover of Vitamin C. Toxicity is characterized by mild GI upset and kidney stones. The upper limit for Vitamin C intake is 2g/day.
Vitamin B1 (thiamine)
Thiamine has many roles: decarboxylation, glycolysis, energy generation (used as a co-factor for several dehydrogenase reactions, in the citric acid cycle). Specifically, thiamine pyrophosphate (TPP) is a coenzyme that supports energy transformation and the production of NADBP and ribose-5-phosphate. Thiamine also plays an unidentified role in the propagation of nerve impulses and takes part in myelin sheath maintenance. Dietary sources for thiamine are grains, legumes, nuts, and seeds. There is no know toxicity of thiamine. Thiamine deficiency will impair glucose breakdown and the generation of ATP, resulting in energy deficits. This is worsened by glucose infusion and highly aerobic tissues (heart/brain) are affected first. The clinical syndromes that occur from thiamine deficiency are wet beriberi and dry beriberi, and Wernicke-Korsakoff syndrome.
Those at risk for deficiency include those with intestinal resections, people with chronic alcoholism, people in liver failure and chronic dialysis patients. Chronic alcohol exposure decreases thiamine absorption in the gut and increases thiamine excretion in the kidney. In liver failure, people have decreased ability to convert thiamine to its biologically active form of TPP. During dialysis, all water-soluble vitamins (including thiam) are susceptible to moving into the dialysate and placing the patient at increased risk for deficiency.
The diagnosis is made by an increase in red blood cell transketolase activity following vitamin B1 administration. Serum thiamine levels can also be checked. However, people are often treated based on history and symptoms alone. In people in whom you have a high suspicion for thiamine deficiency, give intravenous thiamine prior to any glucose infusion to prevent precipitating Wernicke encephalopathy.
Dry beriberi affects the nervous system and is characterized by anorexia, vomiting, dry skin, exhaustion, neurologic and neuromuscular degeneration. It can mimic Guillain-Barré Syndrome. The severity of the neuropathy is characterized by the severity of the thiamine deficiency. It is treated with thiamine and is often reversible.
Wernicke-Korsakoff Syndromes are both forms of dry beriberi. They are a spectrum of disorders including Wernicke’s encephalopathy which is an acute state that is life-threatening and characterized by confusion, ophthalmoplegia, and ataxia. Symptoms are reversible with IV glucose. Korsakoff’s syndrome is the chronic state that is characterized by amnesia, confabulation, and psychosis. Thiamine administration will not lead to improvement of Korsakoff’s syndrome.
Wet beriberi is thiamine deficiency with cardiovascular involvement with or without neuropathy. People may have peripheral vasodilation which leads to high output heart failure. This condition is treated with thiamine and is often reversible.
Vitamin B2 (riboflavin)
Riboflavin, as FAD, supports energy transformation as a co-enzyme that becomes reduced in many redox reactions, including glycolysis, the TCA cycle, and fatty acid oxidation. It also plays an important role in glutathione recycling by providing reducing equivalents to glutathione reductase to produce reduced glutathione. Riboflavin deficiency is very rare, it may be seen in association with other deficiencies. It is largely characterized my inflammatory changes in the mouth such as cheilosis, angular stomatitis, glossitis, as well as corneal vascularization. Dietary Sources for riboflavin are dairy, meat, fortified grains, green vegetables.
Vitamin B3 (niacin)
Niacin encompasses two molecules – nicotinic acid and nicotinamide. In terms of function in the body, niacin’s biologically active form is NAD and NADPH. NAD supports the catabolism of all macronutrient fuels. NADPH supports biosynthetic reactions including fatty acids, cholesterol and steroid hormones. In addition to the co-enzyme role, nicotinic acid has been demonstrated to both lower VLDL levels and raise HDL. The mechanisms of action are not completely known. Niacin deficiency, also known as pellagra, is characterized by the four “D’s”; Dermatitis, diarrhea, dementia, and death. Dietary Sources of niacin include meats, fish, nuts, cereals, legumes. Toxicity includes flushing, hepatitis, insulin resistance. Nicotinic acid has been demonstrated to both lower VLDL levels and raise HDL. The mechanisms of action are not completely understood.
Vitamin B6 (pyridoxine)
Vitamin B6, as pyridoxal phosphate (PLP), is a co-enzyme for an estimated 140 enzymes in the body. PLP plays a role in amino acid metabolism, glycogenolysis and gluconeogenesis, and heme synthesis. Groups at a higher risk for B6 deficiency include dialysis patients, persons on isoniazid treatment, chronic anticonvulsant therapy, and chronic alcoholics. There is a risk of B6 toxicity at doses above 500mg/day chronically from supplementation. This presents as peripheral neuropathy. As a result, the upper limit is set at 100mg/day from supplements. Pyridoxal phosphate deficiency is characterized by polyneuropathy, oxalate stone formation, seborrheic dermatitis, microcytic anemia, glossitis, cheilosis. Dietary Sources include fish, pork, beans, poultry, seeds, grains.
Folate (Vitamin B9)
Folates are a family of enzyme co-factors that carry single carbons, often referred to as one-carbon carriers, for a variety of biosynthetic reactions. Folate describes two different molecules. In the body, we find tetrahydrofolate (THF)and a variety of folate intermediates produced from THF. Folic acid is the synthetic, fully oxidized form of folate that can be converted to THF. Folic acid is found in supplements and fortified or enriched foods. Folic acid became part of the enrichment process in 1998, and is commonly found in a variety of enriched grain products. Folates are also absolutely required in nucleic acid metabolism, as they are necessary for both purine and pyrimidine synthesis. Thus, in folate deficiency, nucleic acid synthesis will be impaired and present as megaloblastic, macrocytic anemia. B12 status will also have a major impact on folate-mediated one carbon metabolism.
Groups at higher risk for folate deficiency include people with chronic alcoholism, persons with malabsorptive disorders, prolonged anticonvulsant therapy, and persons with genetic mutations in MTHFR. Groups with increased folate requirements include pregnancy, infancy, and persons on chemotherapy with methotrexate. Folate deficiency is the most common vitamin deficiency in the United States. While toxicity of folate from foods is not an issue, high dose supplementation of folic acid may mask a B12 deficiency. Thus, the upper limit is set at 1000ug/day from supplements.
In women of child bearing age, folate deficiency during preconception or prenatal increases the risk for neural tube defects. Since the neural tube closes in the first month of pregnancy before many women are aware they are pregnant, women contemplating pregnancy should take 400 ug folic acid/day from fortified foods, supplements, or both. Folic acid is recommended because it has a much higher bioavailability at 85-100% compared to food folates that have 50% bioavailability.
Folate uptake and status can also be impaired with diseases of the jejunal mucosa (such as celiac and tropical sprue), use of certain anticonvulsant’s and birth control drugs (which interfere with splitting of polyglutamate to absorbable monoglutamate), and chronic excessive alcohol intake.
Folate deficiency leads to macrocytic megaloblastic anemia, hypersegmented PMNs, leukopenia, thrombocytopenia, glossitis, stomatitis, neural tube defects in newborns.
Vitamin B12 (cyanocobalamin)
B12, or cobalamin, is required for two reactions in the body. It is a cofactor for methionine synthase that facilitates the movement of the methyl group from 5-methyl THF to homocysteine to produce both THF and methionine. It is also a cofactor for methylmalonyl-CoA mutase, the enzyme that converts methylmalonyl-CoA to succinyl CoA. This is the final step in processing a variety of amino acids and odd-chain fatty acids for entry into the TCA cycle.
Dietary B12 is supplied mostly by animal foods. Vegans and vegetarians are also at high risk for deficiency. Other than inadequate intake, deficiency is caused by malabsorption, lack of intrinsic factor, or absence of terminal ileum. Anti-intrinsic factor antibodies are diagnostic for pernicious anemia. There are 3-4 years of B12 storage in the liver, so deficiency develops over several years.
When anemia occurs, it is the same characteristics as anemia in folate deficiency, presenting as a megaloblastic, macrocytic anemia (due to secondary folate deficiency). Again, due to limited methionine synthase activity, the conversion of 5-methyl THF to THF will be limited. Without THF, the other folate intermediates necessary to produce both purines and pyrimidines will be not produced and result in the hematological outcomes described above. Neurological symptoms are also present in 75-90% of persons with B12 deficiency. Table 3 compares the syndromes of folate and B12 deficiencies.
Folate supplementation can mask a B12 deficiency and resolve the related hematological outcomes, but it will not resolve the neurological outcomes.
Deficiency of B12 is characterized by macrocytic, megaloblastic anemia, hyper-segmented PMNs, neuropathy and subacute combined degeneration due to abnormal myelin, and glossitis.
| Hematocrit | MCV | Homocysteine | Methylmalonic Acid | Neurologic Symptoms | |
| Folate deficiency | LOW | HIGH | HIGH | NORMAL | NO |
| B12 deficiency | LOW | HIGH | HIGH | HIGH | YES |
Table 3. Comparison of clinical features in folate vs. B12 deficiency
Biotin (Vitamin B7)
Biotin, as biocytin, is a co-enzyme for five carboxylase enzymes, which catalyze critical reactions in intermediary metabolism facilitating the generation of fatty acids, conversion of amino acids into TCA cycle intermediates, and pyruvate to oxaloacetate. Beyond a co-enzyme role, biotin plays a role in epigenetic modifications by biotinylation of histones. Biotinylation of histones is associated with decreased gene expression or gene silencing. Biotin has been demonstrated to influence gene expression related to glucose metabolism in favor of hypoglycemia. The dietary sources for biotin are eggs, liver, cereals, vegetables.
Biotin deficiency is rare except for patients on Total Parenteral Nutrition (TPN). Those at higher risk include persons with prolonged antibiotic use, antiseizure medications, and consumption of raw egg whites (7-8 per day) in conjugation with a biotin deficient diet. Raw egg whites contain the protein avidin that avidly binds to biotin during digestion. Heat will denature avidin.
Excess biotin ingestion will interfere with many laboratory assays that use biotin. Excess biotin displaces biotinylated antibody-antigen complexes which can cause false elevation or false lowering of measured analytes (depending on which type of assay is used). This commonly affects thyroid function testing.
Vitamin B5 (pantothenic acid)
Pantothenic acid is a component of coenzyme A (CoA). Pantothenic acid containing CoA is essential to the TCA cycle, fatty acid synthesis, beta oxidation, in addition to many more metabolic processes. The dietary sources are eggs, meats, cereals, and legumes. Pantothenic acid deficiency is extremely rare. The symptoms are dermatitis, enteritis, alopecia, adrenal insufficiency.
Minerals/Electrolytes/Trace Elements
The minerals – calcium, phosphate, and magnesium are essential nutrients, as are the major electrolytes – sodium, potassium, and chloride. In addition, trace elements – iodine, iron, zinc, and copper are necessary for normal body function.
Despite the daily importance of minerals, electrolytes, and elements, this subject matter is not heavily tested on the boards. Below you will find a table for your reference.
Of the minerals, electrolytes, and trace elements listed below, Zinc is occasionally seen in board questions. As mentioned blow, zinc is an essential mineral for activity of over 100 enzymes and important in the formation of zinc fingers (extremely diverse protein motifs that are used in DNA recognition, RNA packaging, transcriptional activation, regulation of apoptosis, protein folding and assembly, and lipid binding). With zinc deficiency, some can develop delayed wound healing, hypogonadism, decreased adult hair (axillary, facial, pubic), anosmia, dysgeusia (distorted sense of taste) acrodermatitis enteropathica. Acrodermatitis enteropathica is a rare genetic autosomal recessive disorder, characterized by periorificial dermatitis, alopecia, and diarrhea. It is caused by mutations in the gene that encodes a membrane protein that binds zinc.
| Electrolyte | Mineral Source | Symptoms of Deficiency |
Function |
Symptoms of Toxicity |
| Sodium | Table salt, seafoods, animal foods, milk, eggs | Hyponatremia | Major cation of extracellular fluid, determines water distribution, osmolarity | Edema, hypertension |
| Potassium | Fruits, milk, meat, vegetables, legumes | Muscle weakness, mental apathy, cardiac failure | Major cation of intracellular fluid, important in regulation of pH, osmolarity, and cell membrane transport, maintains normal muscle irritability. | Confusion, poor respiratory function, decreased cardiac function |
| Calcium | Milk and milk products, sardines, turnip greens, mustard greens, broccoli | Tetany, cramps, seizure, rickets, growth delay in children, osteoporosis and ostoemalacia in adults | Essential for iron transport across cell membranes, formation of bones and teeth, blood clotting, nerve transmission, heart contraction. | Constipation, increased risk of kidney stones, impaired renal excretion. |
| Phosphorus | Milk and milk products, meat, fish, poultry, whole grain cereals, legumes and nuts, baking powder | Neuromuscular, skeletal, renal, and hematological manifestations | Component of every cell and many metabolites, especially DNA, RNA, ATP, & phospholipids, important in PH regulation. | Hypocalcemia and tetany in infants. |
| Magnesium | Whole grain cereals, nuts, met, milk, legumes | Anorexia, growth failure, EKG changes, cramps, tetany seizures | Essential cofactor of many enzymes, critical in energy production and transfer for protein synthesis, contractility of muscle and excitability of nerves | Decreased blood pressure, nausea, vomiting, flushing, confusion, abnormal EKG, decreased reflexes and breathing, cardiac arrest |
| Iron | Fortified cereals, liver, kidney, heart, lean meat, dried beans | Hypochromic, microcytic anemia | Component of hemoglobin, myoglobin, and respiratory enzymes catalyzing oxidation/reduction in cells | Hemosiderosis, hemochromatosis |
| Zinc | Meat, liver, eggs, seafood (especially oysters), whole grain cereals
Zinc lozenges contain 12mg of zinc per lozenge and toxicity can easily be reached |
Poor growth, loss of appetite, hypogonadism, loss of taste and smell, poor wound healing. | Cofactor of > 100 metalloenzymes, critical in DNA, protein, and nucleic acid synthesis | Anemia, nausea, vomiting. Zinc can inhibit copper absorption and chronic doses of zinc >50 mg/day can lead to copper deficiency which is associated with anemia. |
| Copper | Liver, kidney, oysters, chocolate, nuts, legumes, cereals, dried fruits, poultry, shellfish, meat | Anemia, neutropenia, leukopenia, wound dehiscence, growth retardation, heart failure, bone demineralization | Cofactor in collagen metabolism and hemoglobin synthesis | Iron deficiency |
| Fluoride | Major source is supplemented drinking water; ubiquitous although variable quantities, in food stuffs | Pathological decalcification fo calcified tissues | Component of calcified bone | Mottling of and brittle bone |
| Selenium | Cereals, meat, liver, poultry, fish, seafoods, dairy products | Cardiomyopathy, myopathy, anemia | Cofactor of glutathione peroxidase, functions with vitamin E to protect cell membranes & organelles from oxidative damage. | Hair loss, nail changes |
| Manganese | Weat bran, whole grains, legumes, blueberries, nuts, instant coffee & tea | Weight loss, inadequate skeletal mineralization, dermatitis | Oxidative cofactor in mucopolysaccharide synthesis and reproduction | Symptoms resembling Parkinsonism and Wilson’s disease |
| Chromium | Brewer’s yeast, whole grains, margarine, vegetable oils, molasses | In rats: impairment of glucose tolerance, impaired growth, increased cholesterol | Glucose tolerance | Neuropathy |
| Iodide | Seafoods, iodized salt | Goiter | Integral in thyroid hormone synthesis | Goiter |
Table 4. Minerals, electrolytes, and trace elements
Nutritional Assessment
The focus of the comprehensive nutrition assessment is to identify risk factors that may contribute to undernutrition, protein energy malnutrition, dehydration, unintended weight loss and other nutritional problems, as well as identifying other nutritional needs. A comprehensive nutritional assessment includes anthropometric measurement of body composition (weight, BMI, and change in weight); biochemical measurements of serum protein, micronutrients, markers of inflammation, and metabolic parameters (liver function, blood glucose, kidney function); medical, social or psychological factors that may preclude adequate intake; and measurement of dietary intake. Taking a nutritional history helps to identify underlying mechanisms that put patients at risk for nutritional depletion or excess. These mechanisms include: inadequate intake, impaired absorption, decreased utilization, increased losses, and increased requirements of nutrients.
A diet history may elucidate specific nutrient problems. In order to do this, you must assess usual daily food intake. In soliciting a diet history from a patient, try to use straightforward language and open-ended questions.
An accurate diet history involves keeping food records for at least three days, but in clinical practice, most information will be obtained from a 24-hour recall.
Start by asking about any dietary restrictions or habits (gluten free, plant-based, keto, intermittent fasting, etc). The number of meals and snacks consumed per day. Standard meals (breakfast, lunch, dinner) are not consumed by all people. A more open ended question could be: “what time do you eat your first meal of the day?” It is important to know who in the household is responsible for meal planning and food preparation. The frequency of restaurant or fast food dining should be assessed. Different food groups (fruits, vegetables, animal-based proteins, other proteins (tofu, legumes), grains, dessert. Types of beverages consumed should also be known.
Typically, the comprehensive nutritional assessment is performed by a clinical dietitian. However, understanding components that go into a comprehensive nutritional assessment will inform your own dietary history for your patients.
There are several factors at play that can impact an individual’s eating behavior. These factors include the physical environment, the macroeconomic framework, the social environment, and personal factors. Social determinants of health play a major role in the nutritional status of people in United States.
Certain population sub-groups in the United States are vulnerable to malnutrition. Vulnerable groups are women (especially of child-bearing age), non-Hispanic Blacks, people of low socio-economic status, underweight people, individuals with obesity, and individuals with poor diets.
Food choices are likely to be influenced by the accessibility and affordability of food retailers—travel time to shopping, availability of healthy foods, and food prices. Some people and places, especially those experiencing low income, may face greater barriers in accessing healthy and affordable food retailers, which may negatively affect diet and food security. Therefore, it is particularly important to have cultural awareness when collecting a nutrition history and making diet recommendations to your patients.
Understanding groups that are at high risk of malnutrition and micronutrient deficiencies can lead to better and earlier identification of deficiencies and tailor nutrition screening and prevention programs to be most effective.
Malnutrition and Weight Loss Malnutrition
Malnutrition
American public health efforts have placed great emphasis on obesity recently. In contrast, malnutrition is often under-appreciated and under recognized in developed countries. Current estimates suggest that as many as 69% of hospitalized patients are malnourished.
Malnutrition is defined as “an acute, subacute or chronic state of nutrition, in which varying degrees of overnutrition or undernutrition with or without inflammatory activity have led to a change in body composition and diminished function”. Malnutrition may be due to starvation (e.g. anorexia, food insecurity), chronic disease (e.g. pancreatic cancer, sarcopenic obesity, diabetes), or acute disease (e.g. severe infection, trauma). Identification of malnutrition can influence patient care and prognosis. For example, malnourished patients require longer hospital stays, are more likely to discharge to a rehab facility instead of home, present with impaired respiratory and cardiac functions and decreased immune function, and therefore have higher morbidity and mortality rates. Surgical patients with malnutrition have a 4 times higher risk of pressure ulcer development.
The 2012 adult malnutrition consensus statement from ASPEN and the Academy of Nutrition and Dietetics presents a framework for diagnosis of malnutrition according to the following criteria, where identification of two of the following six characteristics are recommended for diagnosis:
- Insufficient energy intake relative to need
- Weight loss
- Loss of muscle mass
- Loss of subcutaneous fat
- Localized or general fluid accumulation that may sometimes mask weight loss
- Diminished functional status as measured by hand grip strength or functional assessment
It is recommended that these factors be routinely assessed upon admission and at frequent intervals throughout the patient’s stay at an acute, chronic or transitional care setting.
The terms marasmus and kwashiorkor are seldom used in clinical practice. Marasmus describes chronic energy deficit and starvation and is characterized by skeletal muscle wasting and loss of subcutaneous fat reserves. Kwashiorkor describes a malnutrition state characterized by peripheral edema with or without ascites, hypoalbuminemia, and leaky capillary membranes.
Weight Loss
Unintentional weight loss is also referred to as involuntary or unintended weight loss. This term excludes weight loss as an expected consequence of treatment (eg, weight loss from diuretic therapy in patients with heart failure) or as a result of a known illness. Patients who experience involuntary weight loss require careful monitoring: a loss of 5% or more in 12 months suggests cachexia. Unintentional weight loss is associated with increased mortality. This is especially relevant for nursing home residents, regardless of the underlying diagnosis.
Cachexia – Weight loss from loss of muscle mass with or without fat loss. Other criteria seen in cachexia are fatigue, decreased muscle strength, and anorexia. Patients often have lab abnormalities as well with elevated CRP, anemia, or hypoalbuminemia.
Sarcopenia – Sarcopenia is a geriatric syndrome characterized by loss of muscle mass, strength, and performance.
Etiology
There are many causes of unintentional weight loss. Most frequently, weight loss is due to decreased food intake (except for conditions that cause increased energy expenditure, such as hyperthyroidism) which can occur due to poor appetite, inability to eat, or lack of food. Any chronic medical condition can cause anorexia and weight loss. Therefore, the differential diagnosis is broken down by organ system. Malignancy and nonmalignant gastrointestinal causes are the most common. The major causes of weight loss are listed in table 5.
| Major Causes |
| Malignancy (pancreatic cancer, lung cancer, GI malignancies, |
| Nonmalignant GI diseases (GERD, celiac disease, IBD) |
| Psychiatric disorders (depression, dementia, delirium, eating disorders) |
| Endocrinopathies (hyperthyroidism, diabetes, adrenal insufficiency) |
| Infectious diseases (HIV, tuberculosis, chronic fungal, bacterial, or helminth infection) |
| Advanced chronic disease (heart failure, renal failure, pulmonary cachexia) |
| Neurologic diseases (stroke, dementia, Parkinson’s) |
| Medications/substances |
| Rheumatological diseases (severe RA, giant cell vasculitis) |
| Chronic vigorous exercise |
| Medications/Substances Associated with Weight Loss |
| Alcohol |
| Cocaine |
| Amphetamines |
| Drug withdrawal syndromes |
| Tobacco |
| Prescription drugs (anti-seizure medications, diabetes medications, thyroid medications) |
| Herbal/non-prescription drugs (caffeine, nicotine, long list of herbal medications) |
Table 5: Major causes of weight loss.
Evaluation
Because the differential diagnosis is so broad, there is no single diagnostic approach for all patients. First, the degree of weight loss must be established. For people who have had a greater than 5% of body weight lost, evaluation should be more intensive.
A complete history should be taken which includes determining the pattern of weight loss, especially the speed of weight loss and prior history of weight fluctuations. Furthermore, it is necessary to assess for intentional weight loss, that might be evidence of disordered eating.
Eating disorders are characterized by a persistent disturbance of eating that impairs health or psychosocial functioning. This includes anorexia nervosa, avoidant/restrictive food intake disorder, bulimia nervosa, pica. The diagnosis is based on the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
Determining the presence of associated symptoms and medications is critical in narrowing the diagnosis. For example, symptoms of malignancy can include fever, night sweats, fatigue. Symptoms specific to a certain type of malignancy are black or bloody stools in the case of colon cancer and pulmonary symptoms in the case of lung cancer). Symptoms of malabsorption (steatorrhea, bloating, watery diarrhea) can indicate a non-malignant GI cause. Additionally, a depression assessment tool (eg, PHQ9) should be used to screen for depression.
Other critical historical pieces include a thorough medication assessment, including supplements.
Physical exam and laboratory evaluation are key components of diagnosis. Initial diagnostic testing is basic and should include complete blood count, electrolytes with renal function, glucose and hemoglobin A1C, TSH, liver function, and inflammatory markers (ESR or CRP). A more targeted evaluation can be done if there are key historical features that suggest a diagnosis.
Treatment
Identification of the underlying cause should be the focus of treating weight loss. Treatment of weight loss often involves a multidisciplinary approach with multiple team members including speech therapy, dietitian, social work, and the medical team. Common strategies to treat unintentional weight loss include dietary changes, nutritional modifications, appetite stimulants, and environmental changes such as assistance with groceries and/or meal preparation.
Diet modification and use of food changes in people who have chewing, or swallowing difficulties may lead to weight gain. Nutritional supplements are used (mostly in liquid form). The purpose of nutritional supplements is to provide extra calories, but they are not intended to serve as a meal replacement and should therefore be given separately from meals.
Several medications to stimulate appetite are available, but none reduce mortality in older patients with unintentional weight loss. Megestrol (Megace), the most commonly studied medication, has been shown to improve appetite and increase weight gain in patients with cancer and AIDS cachexia. Adverse effects of megestrol include gastrointestinal upset, insomnia, impotence, hypertension, thromboembolic events, and adrenal insufficiency. Like all treatments, a risk and benefit discussion needs to be had with patients.
Mirtazapine (Remeron), a serotonin antagonist used to treat depression, causes weight gain in many patients who take this drug for depression. Weak evidence (no randomized controlled trials, all underpowered) has shown that mirtazapine causes weight gain in older patients with weight loss. Dizziness and orthostatic hypotension are side effects and therefore this medication carries significant risk in the elderly population.
Cannabinoids are used in palliative medicine to manage weight loss, pain, appetite and sleep disturbance. Initial trial data shows many patients gain weight with the use of cannabinoids. A more thorough evaluation of side effects is needed.
Components of Healthy Nutrition
Through this century, the US Department of Agriculture has issued food guides (“Dietary Guidelines for Americans”) to serve as foundations for the American diet. Earlier guides focused on ensuring adequate intake to prevent malnutrition syndromes and conformed well to the RDA for major nutrients. by the 1970s it was clear that dietary excess was in fact a major health issue and recommendations changed to include moderation of the intake of some nutrients. The USDA dietary guidelines are very reasonable extensions of current nutritional knowledge to the general population, and provide a basic strategy that should be applied to most patients in medical practice.
The last publication was in 2020 (dietaryguidelines.gov). The goal of the dietary guidelines are to provide advice on what to eat and drink in order to promote health, reduce risk of chronic disease, and meet nutrient needs. The guidelines are designed for policymakers, nutrition and health professionals, and health policy programs. State and local governments, schools, the food industry, and other community groups use these guidelines to develop programs, policies and communication for the general public.
Increasing attention is being paid toward the lack of cultural and ethnic diversity on the field of American dietetics. The USDA dietary guidelines do not adequately address cultural variation in intake. This disparity adds to the systemic inequities that impact nutrition in marginalized communities such as availability of healthy and affordable food options.
The USDA Dietary Guidelines, 2020 – 2025:
- Follow a healthy dietary pattern at every life stage.
- Customize and enjoy nutrient-dense food and beverage choices to reflect personal preference, cultural traditions, and budgetary considerations.
- Focus on meeting food group needs with nutrient-dense foods and beverages, and stay within calorie limits
- A variety of vegetables from all of the subgroups: dark green, red and orange, legumes (beans and peas), starchy, and other
- Fruits, especially whole fruits
- Grains, at least half of which are whole grains
- Dairy products; including milk, yogurt, cheese, and/or fortified soy beverages
- Protein foods, including seafood, lean meats and poultry, eggs, legumes, and nuts, seeds, and soy products
- Oils, including vegetable oils and oils in food, such as seafood and nuts
- Limit foods and beverages higher in added sugars, saturated fat, and sodium, and limit alcoholic beverages
- Added sugars – Less than 10 percent of calories per day from added sugars. Avoid foods and beverages with added sugars for those younger than age 2.
- Saturated fats – Less than 10 percent of calories per day starting at age 2
- Sodium – Less than 2300 mg per day (and even less for children younger than 14 years old)
- Alcoholic beverages – adults of legal drinking age can choose not to drink. If alcohol is consumed, intake should be limited to up to one drink per day for women and up to two drinks per day for men
Popular Diets
The diet industry in the United States is a multi-billion dollar industry. Programs tend to be overly restrictive, unpractical, and unsustainable. Diets are often marketed for the purpose of weight loss and due to the unsustainable nature of these program and contributing physiologic factors, weight regain is common. There are very few diets that are known to have evidence proven beneficial health effects.
Mediterranean Diet is a plant-based eating plan that includes daily intake of whole grains, olive oil, fruits, vegetables, beans and other legumes and nuts. The main focus of the Mediterranean diet is on healthy fats. Meat is not completely eliminated, but red meat is rarely consumed. Fish, seafood, dairy and poultry are included in moderation. Olive oil is the primary sources of added fat in the Mediterranean diet. Because olive oil is a monounsaturated fat, this eating plan lowers LDL cholesterol. The PREDIMED study was a primary prevention trial in patients with high cardiovascular risk looking at diets high in nuts or olive oil compared to a control diet. There was a lower incidence of cardiovascular events in the arms consuming more nuts or olive oil. There is strong evidence to support the health benefits of a Mediterranean diet.
The ketogenic or “keto” diet is a low-carbohydrate, high-fat (70-80% of total daily calories), and moderate-to-low protein diet. The diet avoids carbohydrate-rich foods like bread, pasta, starchy vegetables, and fruit, while foods high in saturated fat, like meat, lard, and butter, and unsaturated fats, such as nuts, seeds, avocados, plant oils, and fish, are allowed. Low glucose intake kickstarts a prolonged fasting state and ketone production once the liver’s glycogen stores are depleted, which will produce mild ketosis (covered in more detail in “Glucose Metabolism”). The keto diet has been shown to facilitate short-term weight loss and short-term improvements in blood glucose, and blood pressure. The fat-rich diet leads to increase in LDL cholesterol levels. However, individuals may experience symptoms of extreme carbohydrate restriction such as hunger, fatigue, mood and cognitive changes, constipation, and headaches. There is no scientific proof of superiority, safety, and sustainability of the ketogenic diet.
Plant-based diets can range from entirely plant based (vegan) to plant forward diets with an emphasis on plant-based foods but not strictly limited to them. There is good evidence to show that plant based diets are associated with lower risk of cardiovascular mortality in the general population, decrease the risk for diabetes and weight gain, and are associated with slower declines in kidney function over time.
