1
Somatic NS efferents. Efferent somatic motoneurons innervate skeletal muscle forming a very large synapse: the neuromuscular junction (NMJ) or motor endplate. They excite action potentials in the muscle by opening depolariz- ing nicotinic ACh receptor ion channels (nAChRs) at the NMJ. Each skeletal muscle fiber is an obligatory follower of the motor axon that innervates it. Each presynaptic action potential propagating in a somatic motor axon elicits one postsynaptic action potential in the skeletal muscle fibers it innervates and one muscle twitch.
Autonomic NS efferents. Almost every organ of the body is innervated by the two autonomic peripheral systems called the sympathetic and parasympathetic nervous systems. In both, the innervation is via a two-neuron relay: first efferent preganglionic neurons and then peripheral postganglionic neurons. The efferent ANS nerve fibers that exit the CNS are called preganglionic because they release their ACh in the peripheral autonomic ganglia to excite the second postganglionic neurons that in turn innervate the peripheral targets of the ANS. The ANS efferent preganglionic nerve fibers form standard, focal, and fast nicotinic synapses on ANS postganglionic neurons. As it is for skeletal muscle, the ACh effect within the ganglion is depolarizing and excitatory, and the postganglionic neuron fires action potentials, acting mostly as a follower: Each preganglionic action potential elicits one or a few postganglionic action potentials in the second neuron. Thus, the somatic motor efferents and the ANS efferents share a common neurotransmitter (ACh) and act on quite similar (but genetically distinct) nicotinic receptors. (ASIDE: The CNS neurons giving rise to autonomic efferents are sometimes called autonomic motor neurons, but to avoid any confusion with somatic motoneurons, we stick to calling them just autonomic efferents here.)
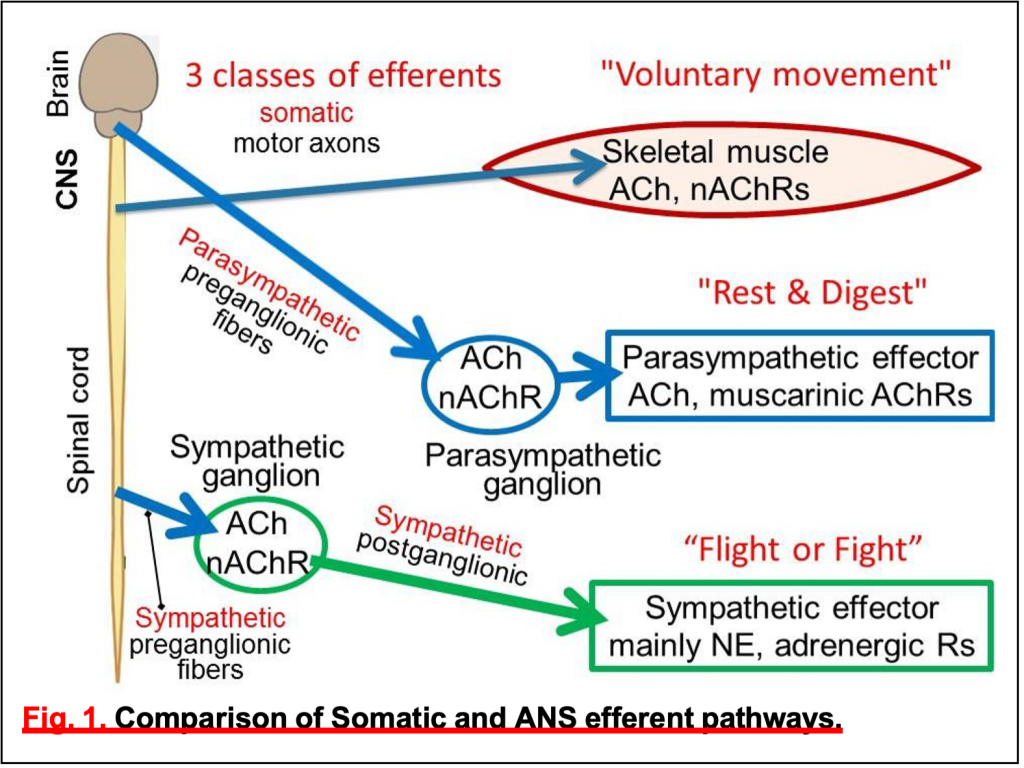
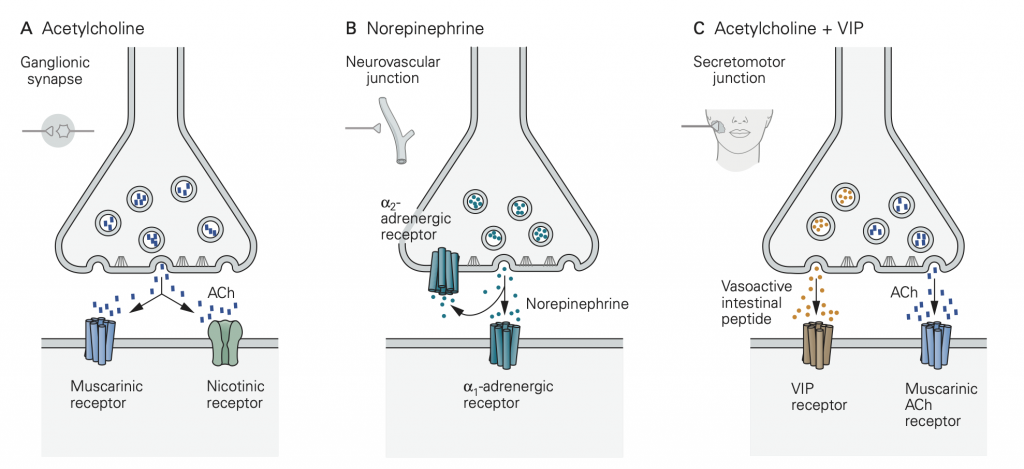
Autonomic postganglionic nerve fibers. We have emphasized that autonomic efferent signals are relayed in a second step by axons of post- ganglionic neurons to their final targets in a two-neuron efferent pathway (Fig. 1)–we call this the “two- neuron rule.” The targets include glands, all muscles, the major organs, epithelia, and blood vessels. Instead of forming terminal focal synapses with point-to-point connections, the postganglionic neurons (the second neurons) of the ANS usually deliver neurotransmitters more diffusely throughout a target tissue by “sprinkled” release from numerous varicosities along the length of their axons. The varicosities are swellings–looking like beads on a string–that you could think of as sprinkler heads arranged along a water pipe. As is true of fast, focal synapses, the varicosities release their neurotransmitters in response to passing action potentials by calcium-dependent exocytosis from intracellular neurotransmitter vesicles concentrated in the varicosity. You should think of the actions of autonomic nervous system axons as broadly regulating groups of cells and tissues rather than as targeting a specific single cell.
Exception: There is an exception to the two-neuron rule in the adrenal gland. The epinephrine-secreting chromaffin cells of the adrenal medulla are directly innervated by the “preganglionic” cholinergic efferent nerve rather than by a two-neuron pathway. However, loosely, one might regard the neuron- related, specialized secretory chromaffin cells as being like postganglionic neurons that deliver their epinephrine hormone/neurotransmitter by vesicular exocytosis, but now in endocrine fashion. They are round cells with no axons but release the hormone from the cell body to blood that circulates everywhere.
Sympathetic postganglionic versus parasympathetic postganglionic neurotransmitterWe have emphasized the common features of postganglionic neurons. We now concentrate on the specialized properties that differentiate the postganglionic sympathetic from the postganglionic parasympathetic nerve fibers–with reference again to Fig.1.
• Sympathetic postganglionic nerve fibers are adrenergic. They release norepinephrine (NE) by exocytosis from synaptic vesicles in their varicosities. (Colored green in Fig. 1)
• Parasympathetic postganglionic fibers are cholinergic. They release ACh by exocytosis from synaptic vesicles in their varicosities. (Colored blue in Fig. 1.)
• Both classes of postganglionic nerve fibers release additional mediators, sometimes called cotransmitters, in addition to NE or ACh. This may include neuropeptides and other small molecules such as ATP or nitric oxide. We do consider them later, but here we emphasize the principal neurotransmitters NE and ACh and their actions.
• Exception: At eccrine sweat glands, sympathetic postganglionic fibers release ACh instead of NE. [ASIDE: Eccrine glands are the common sweat glands of your skin. They are distinguished from the often more smelly apocrine sweat glands found in certain hair follicles.]
Receptors at each synapse: Nicotinic ACh receptors (nAChRs) are fast ligand-gated ion channels used at the cholinergic synapses on skeletal muscle endplates and at the synapses on all postganglionic neurons in autonomic ganglia. They are depolarizing (excitatory), nonselective cation channels that initiate action potentials. These nAChRs relay electrical excitation (action potentials) from the presynaptic neuron to a postsynaptic cell.
Thus, in the ganglion, they help to relay preganglionic action potential messages as postganglonic action potential messages on their way to target organs.
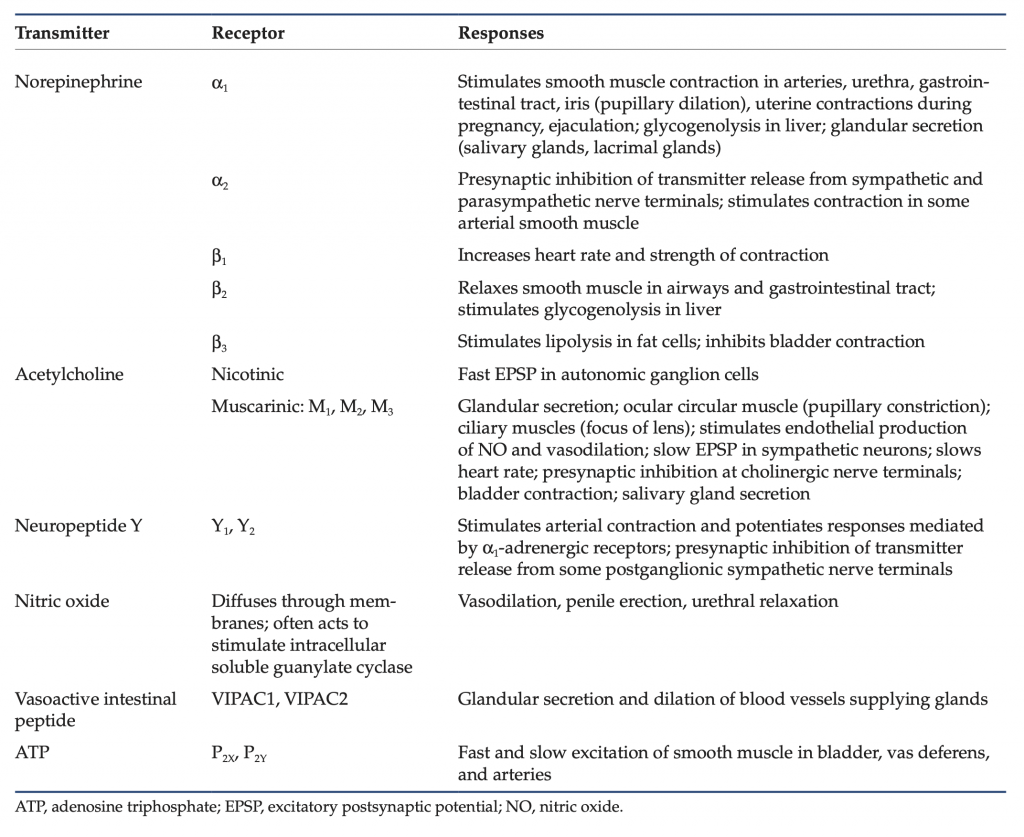
By contrast, various G-protein coupled receptors (GPCRs) are the principal receptors for neurotransmitter in the target organs of the postganglionic sympathetic and parasympathetic nerve fibers. Recall that GPCRs are not ion channels. Rather they initiate cascades of G-protein, calcium, and protein kinase signaling. Thus, action potentials and transmitter release from the postganglionic nerve fibers initiate biochemical signaling cascades in the target tissues, rather than action potentials. Like the postganglionic varicosities that stimulate them, these GPCRs on the target are not discretely organized in specialized postsynaptic structures but rather are diffusely spread over the surface of target cells and tissues. For ANS responses the key GPCRs are:
- Muscarinic ACh receptors (mAChRs, several kinds) mediating parasympathetic effects.
- Adrenergic receptors(α1, α2, and β) mediating sympathetic effects.
- Additional receptors responding to other cotransmitters like ATP, peptides, and NO.